CNS Antiparkinsonian Drugs
advertisement

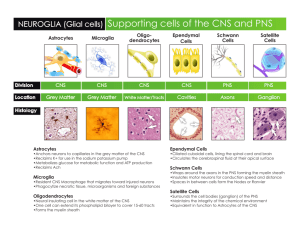
CNS -Antiparkinsonian Drugs Discuss the signs and symptoms exhibited by a patient with Parkinson’s Disease Describe the actions and intended effects of medications used to treat the signs and symptoms of Parkinson’s Disease CNS Antiparkinsonian Drugs Parkinson’s Disease: Disease of the basal ganglia & related neuronal groups + neurotransmitter deficiencies “shaking palsy” Bradykinesia – slowing down in the initiation & execution of movement Rigidity – increased muscle tone Tremor at rest Impaired postural reflexes CNS Antiparkinsonian Drugs Degeneration of dopamine-producing neurons in the substantia nigra of the midbrain Disrupts the balance of: dopamine (DA) – neurotransmitter for normal functioning of the extrapyramidal motor system (control of posture, support, and voluntary motion) Acetylcholine (Ach) and the basal ganglia Symptoms do not occur until 80% of the neurons in the substantia nigra are lost CNS Antiparkinsonian Drugs CNS Antiparkinsonian Drugs Five Stages Flexion of affected arm - tremor / leaning toward unaffected side Slow shuffling gate Increased difficulty walking – looks for support to prevent falls Further progression of weakness – assistance with ambulation Profound disability – may be confined to wheelchair CNS Antiparkinsonian Drugs Tremor First sign Affects handwriting – trailing off at ends of words More prominent at rest Aggravated by emotional stress or increased concentration “Pill rolling” – rotary motion of thumb and forefinger NOT essential tremor – intentional CNS Antiparkinsonian Drugs Rigidity Increased resistance to passive motion when limbs are moved through their range of motion “Cogwheel rigidity” -- Jerky quality – intermittent catches of movement Caused by sustained muscle contraction Muscle soreness; feeling tired & achy Slowness of movement due to inhibition of alternating muscle group contraction & relaxation in opposing muscle groups CNS Antiparkinsonian Drugs Bradykinesia Loss of automatic movements: Blinking of eyes, swinging of arms while walking, swallowing of saliva, self-expression with facial and hand movements, lack of spontaneous activity, lack of postural adjustment Results in: stooped posture, masked face, drooling of saliva, shuffling gait (festination); difficulty initiating movement CNS Antiparkinsonian Drugs Drug Therapy Correcting the imbalance of neurotransmitters within the CNS Dopaminergic – enhance release or supply of dopamine (DA) Anticholinergic – antagonize or block the effects of overactive cholinergic neurons in the striatum Monoamine Oxidase Inhibitor Decreases MAO (the degradative enzyme for DA) Results: DA levels are increased Catechol-O-Methyl Transferase (COMT) Inhibitor Betablocker Antihistamine CNS Antiparkinsonian Drugs CNS Antiparkinsonian Drugs CNS Antiparkinsonian Drugs CNS Antiparkinsonian Drugs CNS Antiparkinsonian Drugs Anticholinergic Drugs: decrease the activity of Ach Benztropine (Cogentin) Antihistamines – decreases rigidity Benadryl Betablockers – decreases rigidity Inderal Monoamine oxidase inhibitor (MAOI): Selegiline (Eldepryl ) Catechol-O-Methyl Transferase (COMT) Inhibitor Entacapone (Comtan) CNS Antiparkinsonian Drugs Drug Therapy Sinemet early in disease becomes ineffective Early: DA receptor agonist -- directly stimulate DA receptors Parlodel, Requip, Mirapex Moderate to severe symptoms: Sinemet is added to therapy CNS Antiparkinsonian Drugs CNS -- Antiparkinsonian Drugs Nursing Process Assessment Head-to-toe Neuro GI/GU Ability to swallow Psychological and emotional coping Parkinson progression Medication History Length of time on medications Changes in medications and effects Safety Ability to perform ADLs independently CNS -- Antiparkinsonian Drugs Nursing Process Nursing Actions Exact timing of medication – cannot be administered late Oral doses given with food Avoid foods in Vit B6 – reverse effects of levodopa Wheat germ, whole grain cereals, muscle & glandular meats (particularly liver), legumes, green leafy vegetables, bananas Force fluids >2,000 mL/day High roughage, high fiber diet CNS -- Antiparkinsonian Drugs Patient Education “Wearing off” – “On-Off” phenomenon – gradual worsening of symptoms as medication begins to lose effectiveness, despite maximal doses “Drug Holiday” when levodopa no longer working effectively (usually 10-day period of hospitalization) Community resources to assist patient and family Safety Effect on blood pressure – Hypotension Hypertensive crisis of MAOI accidentally taken “Sleep attacks” – newer dopamine agonists (pramipexole & ropinirole) GI: Constipation – high fiber, high roughage, increased fluids GU: urine color changes – brownish-orange (entacapone) CNS – Antiparkinsonian Drugs Monitoring Therapeutic Effects Therapeutic Response: Improved sense of well being Ability to perform ADLs Ability to concentrate and think clearly Less intense parkinsonian manifestations Observe for Adverse Effects: Confusion, anxiety, irritability, depression, paranoia, headache, weakness, lethargy, nausea, vomiting, anorexia, palpitations, postural hypotension, tachycardia, dry mouth, constipation, urinary retention, blurred vision, dark urine, difficulty swallowing, and nightmares CNS – Antiparkinsonian Drugs Carbidopa in Parkinson’s disease is to be used: a. As successful monotherapy. b. In conjunction with levodopa to block peripheral conversion to dopamine. c. To decrease the incidence of gastrointestinal side effects associated with levodopa. d. 2 and 3 CNS – Antiparksonian Drugs Discuss the normal course of progression of Parkinson’s disease. Include the rationale for drug therapy to alleviate the symptoms.