ONCOLOGY FOR THE INTERNIST
CANCER SCREENING
Devapiran Jaishankar
Associate Professor
ETSU
Disclosures
• No disclosures
Questions? Questions? Questions?
• Is there a guideline ?
• What is the guideline ?
• Has there been a change ?
• Why ?
• How do I adopt it for the patient in front of me ?
Cancers to Screen ?
• Cervical cancer
• Lung cancer
• Colon cancer
• Breast cancer
• Prostate cancer
USPSTF Grades of Recommendation
Annals of Internal Medicine ; June 2012
Levels of
Certainty
High
Consistent results
Moderate
Sufficient evidence,
confidence constrained,
future recommendations
may alter
Low
Insufficient evidence
not generalizable
Why we screen for cervical cancer
• Annual incidence: 6.6 per 100,000 women
• 12,000 new cases in 2010 in the US
• 4200 deaths in 2010 in the US
• Dramatic decrease in mortality
• Most cases in the US related to inadequate screening
Cervical cancer
Who should we screen
• All women with a cervix regardless of sexual history
• Women aged 21-65
• The guidelines do not apply to the following patients
•
•
•
•
1. High grade precancerous lesion
2. Prior cervical cancer
3. In utero exposure to DES (diethylstilbestrol)
4. Immuno compromised status - HIV positive patients
Cervical cancer screening
Guidelines Summary
Annals of Internal Medicine; June 2012
Cervical cancer screening methodology
•
Conventional cytology as good as liquid based cytology
• HPV testing slightly more sensitive but with higher false
positives
• HPV testing positive more often in younger women
( age < 30-35 years)
• Cervical cancer common in older women (age 35-55)
Cervical cancer
Potential harms to screening - treatment
Surveillance
• Pain:
15%
• Bleeding: 17%
• Discharge: 9%
vs Surveillance and Immediate colposcopy
vs
39%
vs
47%
vs
34%
• Cervical conization or Loop electrosurgical excision
–
–
–
–
Pain:
67%
Bleeding 83%
Discharge 63%
Adverse outcomes with future pregnancies
(preterm delivery < 40 weeks, low birth weight and perinatal mortality)
What is adequate cervical screening
history in the elderly ?
• Current guidelines define adequate screening as
–
–
–
–
3 consecutive negative cytology results or
2 consecutive negative HPV tests
Within the ten year period before stopping cervical cancer screening
With the most recent test performed within the last 5 years
• Screening women who have never been screened reduces
mortality by 74% ( even if age > 65 )
• 29% of all invasive cervical carcinoma in women never
screened
• 50% of invasive cervical carcinoma in women never screened
or not screened in the last 5 years
Cervical cancer biology
• Invasive cervical carcinoma is almost universally linked to
HPV infection
• HPV infection of the cervix is generally transient
• When this infection is not cleared by the immune system
• And the HPV strain happens to be an oncogenic strain
• Incorporation of the oncogenic HPV genome into the host
• Development of precancerous lesions: CIN
• Invasive cervical carcinoma
• Long preclinical phase: Infection Pre cancer Invasive cancer
Lung Cancer Screening
• USPSTF: Recommendation I :
Insufficient evidence for or against screening of asymptomatic
patients with
– Low dose helical CT
– CXR
– Sputum cytology
• American Cancer Society: Interim guidance:
– To discuss the NLST results in the appropriate setting
• NCCN: mentions possible mortality benefit in the right setting
but makes no concrete recommendations
Lung Cancer Screening
What is the right setting ?
NLST and I- ELCAP: 2 landmark screening trials
• NLST National Lung Cancer Screening Trial:
Eligibility criteria
•
•
•
•
•
•
Patients aged 55-70
More than 30 pack year history of smoking
Smokers and non-smokers ( quit within last 15 years)
No metallic implants in chest or back
No prior history of lung cancer or symptoms suggestive of
Not home O2 dependent
NLST
National Lung Cancer Screening Trial
• 53,454 patients at 33 US medical centers
• High risk patients
• August 2002 through April 2004
• Randomized to 3 annual screenings
• Low dose CT vs CXR (PA view)
• And then surveillance for another 3.5 years
• Data collected through Dec 31st 2009
Baseline
characteristics
of patients
Overall patients were
Younger
Better educated
Former smokers
Compared to the 20022004 US census survey
NEJM 365;5 Aug 4th 2011
NLST
Results
Low dose CT
CXR
24% positive test result
Of which 96% false positive
6.9% positive test results
Of which 94% false positive
1060 cancers
645 per 100,000 person years
941 cancers
572 per 100,000 person years
247 deaths/ 100,000 personyears
309 deaths per 100,000 personyears
NLST
What is a positive test ?
• Non calcified nodule: CXR
• Non calcified nodule > 4mm in size: CT
• Adenopathy, Pleural effusion
NEJM; August 4th 2011
NLST
Follow up of positive test results
Low dose CT
18,146 positive results
CXR
5043 positive results
•
•
•
•
•
•
•
•
•
•
CT chest:
PET:
Per cut bx:
Bronch:
Surg bx:
8,807 (50%)
1,471 (8.3%)
322 (1.8%)
671 (3.8%)
713 (4.0%)
• Lung cancer 649 (3.6%)
CT chest:
PET:
Per cut bx:
Bronch:
Surg bx:
3,003 (60%)
397 (8.0%)
172 (3.5%)
225 (4.5%)
239 (4.8%)
• Lung cancer 279 (5.5%)
NLST
Complication rate
Lung cancer diagnosed
No lung cancer diagnosed
Low dose CT: (649)
None = 71% (465)
Major = 11% (75)
Mod = 14% (95)
Death = 1.5% (10)
CXR group: (279)
None = 76% (214)
Major = 8.6% (24)
Mod = 12.5% (35)
Death = 3.9% (11)
Low dose CT: (17,053)
None = 99.6% (16,992)
Major = 0.1% (12)
Mod = 0.3% (44)
Death = 0.1% (11)
CXR group: ( 4,674)
None = 99.7% (4,658)
Major = 0.1% (4)
Mod = 0.2% (9)
Death = 0.1% (3)
NLST
Stage and Screening
Low dose CT
CXR
Stage
Stage
•
•
•
•
•
•
•
IA 416/1040
IB
IIA
IIB
IIIA
IIIB
IV
40%
10%
3.4%
3.7%
9.5%
11.7%
21.7%
•
•
•
•
•
•
•
IA 90/519
IB
IIA
IIB
IIIA
IIIB
IV
21.1%
10%
3.4%
4.5%
11.7%
13.1%
36.1%
NLST
Final Results
Diagnosis of lung cancer
645 cases vs 572
low dose CT vs CXR
Rate ratio, 1.13;
95% confidence interval (CI)
1.03 to 1.23
Cancer related mortality
247 deaths per 100,000
person years vs 309
Relative reduction of 20%
95% CI (6.8 to 26.7)
P = 0.004
NEJM August 4th 2011
NLST
Mortality statistics
All cause mortality
CT
CXR
1865/ 26722 = 6.9%
1991/26732 = 7.4%
Lung cancer mortality
427/26722 = 1.59%
503/26732 = 1.88%
NEJM August 4th 2011
Lung cancer screening
Summary
•
•
•
•
Low dose helical CT does detect more lung cancer
These lung cancers are at an earlier stage
High false positive rate
Lower lung cancer death rate
– Relative risk reduction 20%
– Absolute risk reduction < 1%
• Lower lung cancer death rate offset by higher cardiorespiratory complications and death
• All cause mortality marginally better with screening
Colon cancer
Screening
• Colorectal cancer is the third most common type of cancer
• Leading cause of cancer death in the US
• Current levels of screening lag other effective cancer screening
tests
• Effective screening can save over 18,000 lives a year
• Screening guidelines do not apply to
– Lynch syndrome, FAP syndrome
– Inflammatory Bowel Disease
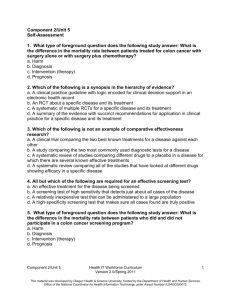
From: Screening for Colorectal Cancer: U.S. Preventive Services Task Force Recommendation Statement
Ann Intern Med. 2008;149(9):627-637. doi:10.7326/0003-4819-149-9-200811040-00243
Figure Legend:
Screening for colorectal cancer: clinical summary of a U.S. Preventive Services Task Force (USPSTF) recommendation.For a
summary of the evidence systematically reviewed in making these recommendations, the full recommendation statement, and
supporting documents, please go to http://www.preventiveservices.ahrq.gov. FOBT= fecal occult blood testing.
*These recommendations do not apply to individuals with specific inherited syndromes (the Lynch syndrome or familial
adenomatous polyposis) or those with inflammatory bowel disease.
Date of download:
10/13/2012
Copyright © The American College of Physicians.
All rights reserved.
Colon cancer
Screening Tools
• Fecal Occult Blood Test: FOBT
– Hemoccult II / SENSA
• Fecal Immunochemical Test: FIT
• Sigmoidoscopy
• Colonoscopy
• Not recommended
– CT Colonography
– Fecal DNA test
Colon Cancer Screening
Stool Tests
• Overall sensitivity for cancer = 70%
• Specificity > 90% ; less than 10% false positive rate
• Hemoccult tests for peroxidase activity of heme
– Dietary heme (fruits and vegetables especially if raw)
– Red meat
– Vitamin C
• FIT: Fecal Immunochemical Test tests for human heme
• Fecal DNA tests for denovo/ somatic mutations in the mucosal
lining of the bowel
Colon Cancer Screening
Endoscopic tests
Colonscopy
• Perforation: 3.8/ 10,000
• M. Bleeding: 12.3/ 10,000
• Serious complic: 25/ 10,000
–
–
–
–
–
–
–
Perforation
Major bleeding
Diverticulitis
Sev abdominal pain
Hospital admission
Cardiovascular events
Death
Sigmoidoscopy
• Perforation: 4.6/ 10,000
– Point estimate
• Serious complic: 3.4/ 10,000
Untoward and
Unexpected side
effects of …..
colon cancer
screening
Colon Cancer Screening
Net Benefit
• Annual high sensitivity fecal occult blood testing
– 256-259 life years gained for every 1,000 persons screened
– 2654 colonoscopies per 1,000 persons over 10 years
• Flex- Sig every 5 yrs + FOBT every 3 yrs
– 257 life years gained for every 1,000 persons screened
– 1655 colonoscopies per 1,000 persons over 10 years
• Colonoscopy every 10 years
– 271 life years gained for every 1,000 persons screened
– 3756 total colonoscopies per 1,000 persons over 10 years
Colon Cancer Screening
Summary
• Start- age 50 : stop- age 75
• Screening vs Surveillance guidelines
• Do not recommend routine screening: ages 75-85
• Recommend against any screening after age 85
• Subsets where screening guidelines do not apply
• Positive result colonoscopy : gold standard
• CT colonography, Fecal DNA: Grade I recommendations
Breast Cancer Screening
• Commonest cancer in women worldwide
• Most common cause of cancer related death world wide
• Second most common cause of cancer death in the US
• Lifetime risk in the US: 1 in 8
• Screening guidelines not applicable > 20-25% lifetime risk
– Based on genetic testing
– Strong family history
– Prior chest wall irradiation
Risk factors for
Breast Cancer
Risk assessment tools
Gail model
Claus model
NEJM September 15th 2011
From: Screening for Breast Cancer: U.S. Preventive Services Task Force Recommendation Statement
Ann Intern Med. 2009;151(10):716-726. doi:10.7326/0003-4819-151-10-200911170-00008
Figure Legend:
Screening for breast cancer using film mammography: clinical summary of USPSTF recommendation.For a summary of the
evidence systematically reviewed in making these recommendations, the full recommendation statement, and supporting
documents, please go to www.preventiveservices.ahrq.gov.
Date of download:
10/13/2012
Copyright © The American College of Physicians.
All rights reserved.
Risks of Screening Mammography
• False positive results
–
–
–
–
More common in younger women ( 49% over 10 years)
Short term anxiety
possible small but significant risk of long term effects
Other associations
• False negatives
– Insufficient data
• Radiation risk
– 86 cancers and 11 deaths / 100,0000 women screened
• Over diagnosis ?
From: Screening for Breast Cancer: U.S. Preventive Services Task Force Recommendation Statement
Ann Intern Med. 2009;151(10):716-726. doi:10.7326/0003-4819-151-10-200911170-00008
Figure Legend:
Screening for breast cancer using methods other than film mammography: clinical summary of USPSTF recommendation.For a
summary of the evidence systematically reviewed in making these recommendations, the full recommendation statement, and
supporting documents, please go to www.preventiveservices.ahrq.gov.
Date of download:
10/13/2012
Copyright © The American College of Physicians.
All rights reserved.
Incidence of Breast Cancer
SEER data: NCI 2010
Risk reduction in Breast cancer
Relative or Absolute
NEJM 365:11
Breast cancer screening groups
Annals of Internal Medicine; 17 November 2009
Models &
Screening
strategy
Percentage of breast cancer
mortality reduction
vs
Number of mammograms
Per 1,000 women
Annals of Internal Medicine; 17 November 2009
Breast cancer screening
Annual vs Biennial
Annals of Internal Medicine; November 2009
Risk vs Rewards
Age and breast cancer screening
Annals of Internal Medicine; 17 November 2009
Guidelines Galore
Warner E. N Engl J Med 2011;365:1025-1032.
NEJM: September 15, 2011
Breast Cancer Screening
Summary
•
•
•
•
•
•
Do not screen prior to age 40
Discuss screening age 40 -49
Routine screening age 50 onwards: every 1-2 years
Possibly stop screening at age 75
Encourage “ Breast awareness”
May consider clinical breast exam ? Annual ? Start age 40
• Do not hesitate to exam and image the breast, no matter what
age, if clinical symptoms or signs warrant it
Prostate cancer
overview
• Annual data in the US
– 240,000 new diagnoses
– 28,000 deaths
• Median age at diagnosis: 67 years
• Median age at death: 81 years
• Autopsy studies reveal occult prostate cancer
– 30% of men older than 50 years
– 70% of men older than 70 years
Prostate Cancer
The Big Picture
NEJM November 2011
The case for or
against the PSA
90 % of cases diagnosed in
the US are due to screening
Lifetime risk doubles
9% to 16% with PSA
Causes of raised PSA
BPH, infection,
ejaculation, perineal trauma
instrumentation, cancer
NEJM November 2011
Prostate cancer screening
The guideline wars
NEJM November 2011
European Randomized Study of
Screening for Prostate Cancer
• ERSPC
ERSPC
Cancer diagnoses
8.2 % screening group
4.8% control group
Cancer death
2.8 per 1000: screening
3.5 per 1000: control
20% relative risk reduction
To prevent 1 death
need to screen 1410 pts
need to dx 48 cancers
over 9 years
NEJM March 2009
PLCO
Project
1993-2001: 76,693 patients
Annual PSA + DRE
vs
Usual care
2820 cancers: screen
2322 cancers: control
50 deaths: screen
44 deaths: control
Contamination rate: 40%
NEJM March 2009
PLCO Project
Prostate Lung Colon Ovarian
NEJM March 2009
SPCG
Scandinavian Prostate Cancer Group
• Enrolled 1989-1999 follow up through 2009
• 695 patients
• Localized prostate cancer
– T1-T2 lesions
– PSA < 50
– Negative bone scan
• Predominantly diagnosed with symptoms and not PSA
screening
SPCG-4
Radical prostatectomy vs
Watchful waiting
695 pts
12.8 years
347 166 55
348 201 81
Prostate cancer related
mortality 14.6 % vs 20.7%
Need to treat = 15
NEJM May 2011
PIVOT
Prostate cancer
intervention vs observation
trial
1994-2002
44 V.A and 8 NCI sites
Any grade histology
Median age: 67
Median PSA: 7.8
T1c disease: 50%
Gleason >/= 7: 48%
NEJM July 2012
PIVOT
Prostate Cancer Intervention vs Observation Trial
• All cause mortality
• 171 (47%) vs 183( 49.9%)
• HR: 0.88, p=0.22
• Prostate cancer mortality
• 21 (5.8%) vs 31 (8.4%)
• HR: 0.63, p=0.09
• Median survival 13 yrs
• Subgroup analysis showed benefit
in PSA > 10 and
NEJM July 2012
Treatment related Toxicity
Prostate Cancer
NEJM July 2012
Prostate cancer screening
Summary
NEJM November 2011
Cancer screening summary
• Cervical cancer:
• Colon cancer:
Screening works. Target the unscreened
Screening works. Needs larger adoption.
• Lung cancer:
Not ready for mainstream?
Target high risk groups.
Fraught with issues
• Breast cancer:
Screening works but who and how often.
Benefits are possibly more modest than
expected.
• Prostate cancer:
Screening unlikely to decrease mortality.
THANK YOU