Non-Calendar Year Plans

November 11, 2010
Health Care
Reform: Are You
Ready for 2011?
Melissa B.
Kurtzman, Esq.
Philadelphia, PA mkurtzman@littler.com
267.402.3036
Agenda
2011 Benefit Plan
Changes
Grandfathered Plans
Are they worth it?
Non-Discrimination
Rules
Limits to Flex Plans
Changes Taking Effect in 2011 (Generally)
Calendar Year Plans
Effective as of January 1,
2011*
Non-Calendar Year Plans
Effective for Plan Years
Starting on or after September
23, 2010*
* The changes taking effect during this period are referred to as the 2011 Changes
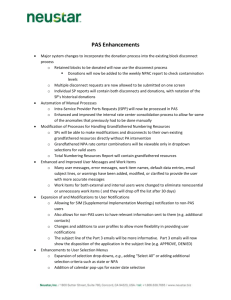
2011 Changes
2011 Change
Restriction on
Lifetime Limits
No Rescission of Coverage
Mandatory Dependent Coverage
Pre-existing Condition Exclusion –
Individuals Under Age 19
Required Preventative Services
Nondiscrimination Rules Extend to
Insured Plans
Expanded Claims Review Process,
Internal Review Process, External
Review
Expanded Disclosures
New Patient Protections
Applies to
Grandfathered Plans
Yes
Yes
Yes
Yes
No
No
Applies to Non-
Grandfathered Plans
Yes
Yes
Yes
Yes
Yes
Yes
No
No
No
Yes
Yes
Yes
2011 Changes – All Plans
No Lifetime Limits
May no longer impose lifetime limits on the dollar value of essential health benefits
No prohibition on lifetime limits on non-essential health benefits
Out-of-network v. in-network
Reenrollment opportunity
– Must provide notice by first day of first plan year on or after September
23, 2010, i.e., January 1, 2011, that lifetime limit no longer applies
– At least 30-day enrollment period
Applies to grandfathered plans
2011 Changes – All Plans
Restricted Annual Limits
Before 2014 - plan may impose restricted annual limits only on dollar value of essential benefits
– At least $750,000 for 2011 calendar year plan
– At least $1.25 million for 2012 calendar year plan
– At least $2 million for 2013 calendar year plan
Starting in 2014 - no annual limits
However, plan may have annual limits on nonessential health benefits
Applies to grandfathered plans
2011 Changes – All Plans
Restricted Annual Limits
Before 2014 – plan or issuer may apply for waiver of new restrictions
September 3, 2010 – procedure established for waiver applications
Plan administrator or CEO of issuer must certify that if annual limits are imposed, there will be either a significant decrease in access to benefits or a significant increase in premiums paid by covered participants
Plan must have been in existence prior to 9/23/2010 and application must be filed 30 days in advance of 2011 plan year
2011 Changes – All Plans
No Rescission of Coverage
May not rescind coverage except for fraud or intentional misrepresentation of material fact
Must give 30 days prior notice
Rescission is retroactive cancellation of coverage
Applies to Grandfathered plans
2011 Changes – All Plans
Extension of Dependent Coverage
Overview – General Requirements
– Plans that provide dependent coverage must extend coverage for adult children until 26 years old
– Applies to health FSAs
– Terms cannot vary based on age
– No premium surcharge
– Does not include grandchildren
– Eligibility may be based only on relationship between the participant and the child
• For “child” as defined in Section 152(f)(1) of IRC, cannot base eligibility on tax dependency criteria
– Variation of rule applies to Grandfathered plans until 2014
2011 Changes – All Plans
Pre-existing Condition Exclusions – Under Age 19
May not impose preexisting condition exclusions on individuals under age 19
Starting in 2014, plans may not impose pre-existing exclusions on any person
Applies to Grandfathered plans
Non-Grandfathered Plans 2011 Changes
Preventive Services
Applies to nongrandfathered plans
No cost-sharing for in-network providers
Must Provide:
– Immunizations
– Screenings for children
– Breast cancer screenings
– Mammography
– Other recommended services
Non-Grandfathered Plans 2011 Changes
New Claims Review Procedures
Applies to non-grandfathered plans
Modifies/expands requirements under existing DOL claims procedure regulations
Requires independent external appeal process
Expands types of decisions to which the appeal procedures apply (coverage rescissions deemed to be claims denial)
Description of internal review process requirements and external review process must be set forth in SPDs, insurance policies, certificates of coverage, membership booklets, etc.
2011 Changes
Patient Protections
Applies to non-grandfathered plans
Emergency services without prior authorization or network restrictions
Choice of Providers
– Designation of primary care provider or pediatrician from available participating providers
– No authorization or referral required for OB/GYN
– Plan must provide notice of rights regarding choice of providers
Grandfathered Plans
Are They Worth It? Overview
Exempt from some, not all, insurance market reforms*
Collectively-bargained plans that are insured have special rules
Interim Final Regulations issued
June 14, 2010
* Insurance market reforms apply to self- insured plans as well as insured plans
Grandfathered Plans
What the Interim Final Regulations Say
Separate Benefit Packages
– Grandfathered rules apply separately to each benefit package
– For example, a high, mid and low plan may be treated as three separate plans for purposes of applying grandfathered status rules
Grandfathered Plans
What the Interim Final Regulations Say
Minimum Requirements
– Plan must be in existence on March 23, 2010
– Must retain documentation of terms of plan in existence on March 23, 2010
– Mandatory disclosure of grandfathered status to participants / beneficiaries
– Plan design and contributions generally may not be changed or, if changes are allowed, changes must fall within prescribed limits
Grandfathered Plans
What the Interim Final Regulations Say
Changes that will result in loss of grandfathered status
– New insurance policy, certificate, or contract of insurance (other than renewal)
– Elimination of benefits for diagnosis or treatment of particular conditions
– Add or decrease annual limits
Grandfathered Plans
What the Interim Final Regulations Say
Changes that will result in loss of grandfathered status (cont.)
– Increase in coinsurance percentage
– Increase deductible or out-of-pocket maximum by more than medical inflation + 15% (measured from March 23,
2010)
– Increase in fixed amount co-payment by more than the greater of (1) $5 increased by medical inflation or (2) medical inflation plus 15% (measured from March 23,
2010)
Grandfathered Plans
What the Interim Final Regulations Say
Changes that will result in loss of grandfathered status (Cont.)
Decrease in employer’s contribution rate by more than 5% from March 23, 2010
– Test applied for each tier of coverage
– Contribution rate is total cost of coverage (equal to
COBRA cost for self-insured plans) less amount paid by employee (whether pre-tax or post-tax) divided by total cost of coverage
– Consider impact of wellness program rewards on calculation of rate
Grandfathered Plans
Practical Considerations for Employers
Evaluate each benefits package separately
Weigh advantages of retaining grandfathered status against advantages of making plan changes that will cause loss of grandfathered status
Limited flexibility for permissible cost-saving changes will diminish over time, making it more difficult to retain grandfathered status
Review insurance policy to be sure early renewal
does not result in new policy, certificate, or coverage
Non-Discrimination Rules for Non-Grandfathered Plans
PPACA imposes new nondiscrimination rules on certain health plans
Effective for plan years beginning on or after September 23, 2010
Only applies to non-grandfathered plans
New rules reference Code § 105(h), which previously applied only to selfinsured health plans
Limited enforcement in past for selfinsured plans
What Types of Plans Are Not Subject to Nondiscrimination?
Dental
Health FSAs
Vision
HSAs
LTC
Med supplemental
Fixed/hospital indemnity
Disability
Specified disease
On-site medical
Retiree-only plans
The Nondiscrimination Tests
Two tests: Eligibility and
Benefits
– Both tests look to if the plan disproportionately benefits highly compensated employees (HCEs):
• 5 highest paid officers;
• More than10% shareholders; and
• Highest 25% paid (for purposes of the eligibility test disregarding certain excludable employees if not plan participants).
The Nondiscrimination Tests
Excludable employees include:
– Part-time employees working less than 25-35 hours per week
– Seasonal employees
– Employees with less than 3 years of service as of the beginning of the plan year
– Employees subject to collective bargaining agreement
– Employees under age 25 as of the beginning of the plan year
– Non-resident aliens earning no US source earned-income
Eligibility Test
A plan must satisfy one of the following
3 tests:
– 70% or more of all employees participate in the plan
(the 70% test)
– 70% of all employees are eligible to participate in the plan, at least 80% or more of those eligible do participate (the 70/80 test); or
– The plan benefits a nondiscriminatory class of employees (the “nondiscriminatory classification test”)
Eligibility Test
Nondiscriminatory Classification
The classification must be based on objective and reasonable criteria and satisfy certain numeric testing
– July 31, 1997 IRS Guidance permits use of prior (preTRA ‘86) or current law under Code 410(b) www.dol.gov
Benefits Test
Default test
– All benefits provided to an HCE under the plan are provided to all plan participants
• Coverage, rather than what is actually paid
• No lower deductibles or copayments
• No actuarial equivalence
• Makes testing two insured arrangements under one “plan” almost impossible
Benefits Test
Optional benefit test (assuming the plan meets the eligibility test discussed earlier)
– As long as each participant may elect any benefit under the plan at the same cost, a plan is not discriminatory
• Plan offers HMO and indemnity option and all can elect
• Helpful for testing plans with multiple insured arrangements
Concerns
Cannot shift HCEs to after-tax premiums
– Can avoid Code § 105(h) with self-insured plans by shifting premiums to after-tax dollars (this operates to convert employer-paid self-insured coverage to
Code § 104(a)(3) coverage which is not subject to nondiscrimination rules)
Concerns
Interaction with cafeteria plan nondiscrimination rules
– Compliance with new laws do not give a free pass on cafeteria plan rules
– Substantial overlap with Code § 105(h) rules (e.g., both impose eligibility tests and allow for use of nondiscriminatory classifications), but there are differences (e.g., different HCE definition, key employee concentration test)
FLEX Plan Limits
Effective for tax years beginning after
December 31, 2010
Health FSAs, HRAs, and
HSAs may no longer reimburse or pay for over-the-counter medicine or drugs without a prescription
Health Care Reform
What Employers Should Do Now
Apply for early retiree reinsurance program if eligible
Review plan documents, summaries and SPDs for compliance with near-term insurance market reforms
Evaluate whether any post March 23, 2010 or proposed plan changes would cause a loss of grandfathered status
Consider advantages of retaining grandfathered status versus advantages of plan changes
Ensure timely distribution of special notices and provide appropriate special enrollment opportunities
Revise health FSA, HSA and HRA open enrollment materials
IRS Circular 230 Notice: Any information regarding Federal taxation contained in this document is not intended to constitute individual legal advice and is not intended or written to be used, and cannot be used by the recipient or any other person, for the purpose of avoiding any Internal Revenue Code penalties that may be imposed on such person. Recipients of this document should seek advice based on their particular circumstances from an independent tax advisor
Littler Locations
Health Care Reform
Resources for Up-to-Date Info
Littler’s Healthcare Blog:
– www.healthcareemploymentcounsel.com
U.S. Department of Labor Employee Benefits
Security Administration:
– www.dol.gov/ebsa
The U.S. Government Website
– http://www.healthcare.gov/center
Melissa B.
Kurtzman, Esq.
Philadelphia, PA mkurtzman@littler.com
267.402.3036