5.20.13 Daily Operations

DAILY OPERATIONS FOR
ACUTE, INPT REHAB, AND
SNF
Med Surg II – PT Eval and POC
Acute Care
Beginning of the Day
•
•
Collect the new consults (orders) for PT
• Some mechanism for getting PT orders to the PT Dept.
•
•
•
•
• Written at all hours of the day and night
Written as
• PT Evaluate
•
•
•
PT Evaluate and Treat
PT for Gait Training
PT for ROM 2x per day
• Continue with ambulation 3x/day in hallway
Organize the day’s list – how do you split the pts up between PT and
PTAs?
Teams
Specialty/Pt Population
Number of staff to pt population
•
•
•
•
Ex. Flint Area Hospitals – orders, philosophy of mobility
McLaren – 6 PTs to 45 pts
Genesys – 5 PTs to 90 pts
Hurley – 4 PTs to 45 pts
• How will you prioritize the patient list?
Priority
• Evaluations
• Jt Commission: must evaluate within 24 hrs of when the order was written
• Patient Population
• Type of surgery such as orthopedics
• Specialty Centers such as Stroke Center
• Short LOS
• Acuity but shows progression to home
• Shows progression to rehab
• Limited time (ex ER Observation)
Pt List
• 15 New evals
• 30 Treatments
• 10 may go home today
• 7 are in the Jt Program (TKA/THA)
• 3 are general surgery
• 7 are potential rehab candidates
• 3 are in ICU on hold
• 5 are day 2-3
• 5 are to be seen every other day with 3 of them to be seen today
PT Lists
8 Evals
3 Rehab
Candidates
5 day 2-3
1 Seen Today
Check on 1 ICU
Hold
18 pts
5 Evals
3 General Surgery
Home Today
5 Rehab Candidates
2 Seen Today
Check on 1 ICU Hold
2 Evals
7 Jt Program
(TKA/THA) seen BID
Check on 1 ICU
Hold
16 pts 10 pts with 7
BID but have assistance
PT 1
• 8 Evals
• In am 7 evals, two hold
• In pm 1 evals
•
•
•
Treatments
• ICU off hold with trt
See Today
•
One rehab candidate, one rehab candidate d/c to rehab
One Day 2-3
Two evals hold, 4 Day 2-3 not seen
•
•
•
•
•
•
•
•
•
7:00-7:30 Get list ready and prep
7:30-8:15 Eval
8:30 – 9:15 Eval
9:20-9:25 Eval but test pending
9:30-9:35 Eval but test pending
9:35-9:10:10 Eval
10:10-11:00 Eval
11:00-12:00 Eval
12:00-12:20 ICU off hold
Lunch
1:00-1:40 Eval
1:40-2:10 See Today
1:40-2:15 Rehab Candidate
2:15-3:00 Day 2-3
3:00-3:15 Billing for day, prep for tomorrow
PT 2
•
•
•
•
•
5 Evals
•
•
In am 4 evals
In pm 1 eval
3 General Surgery
•
Home Today
In am 3 Gen Surg
5 Rehab Candidates
• In pm Rehab
2 Seen Today
• In pm See Today
Check on 1 ICU Hold
• In pm Check
•
•
•
•
•
•
•
•
•
•
•
•
•
• 7:00-7:30 Prep/list
7:30-8:15 Eval
8:20-9:00 Eval
9:10 – 9:40 Eval
9:45-10:30 Eval
10:45 – 11:15 Gen Surg
11:15-11:35 Gen Surg
11:45-12:15 Gen Surg
Lunch
1:00 – 1:45 Eval
1:50-2:10 Rehab Candidate
2:15-2:45 Rehab Candidate
2:50-3:05 See Today
3:05-3:15 Billing, Prep for next day
• Did not see 2 rehab candidate, 1
See Today, Did not check on ICU
Hold
PT 3
•
•
• 2 Evals
• In am
7 Jt Program
(TKA/THA) seen BID
Check on 1 ICU
Hold
•
•
•
•
•
• 7:00 – 7:30 List/prep
7:30-8:15 Eval
8:20-9:00 Eval
9:00-11:30 Jt Program
11:30-11:50 Notes
11:55 – 12:10 Check on
ICU
•
•
•
•
Lunch
1:00-2:45 Jt Program
2:45-3:00 Notes
3:00-3:15 Billing
Productivity
•
Direct Pt Care
• Acute: 9-11 pts per day
• Daily vs BID
•
Indirect Pt Care
•
• Documentation
Walking to next area
• Ordering equipment
• Communication with other disciplines
• Obtaining other equipment
• Waiting on other disciplines
•
• For chart
For speaking with pt
• For care
Inpatient Rehab/SNF
Beginning of the Day
• Collect the new consults (orders) for PT
• Some mechanism for getting PT orders to the PT Dept.
• Usually know of admission the previous day so know when you leave that night that there is an evaluation
• Written as
• PT Evaluate
• PT Evaluate and Treat
• PT for Gait Training and General Mobility
• All Pts get 3 hours of therapy so which pt gets PT/OT or
PT/OT/SLP?
Priority
• Evaluations
• Jt Commission: must evaluate within 24 hrs of when the order was written
• All pts receive 3 hours of therapy
Pt List
• 20 Bed Unit
• 2 New Evals
• One PT/OT/SLP so PT = 1 hour
•
One PT/OT so PT = 1.5 hours
• 12 Treatments
• 2 PT/OT/SLP so PT = 1 hour
•
8 PT/OT so PT = 1.5 hour
• 6 Empty Beds
PT Lists
1 Evals for 1 hour 1 Eval for 1.5 hrs
4 – 1.5 hrs 2 – 1 hrs
Conferences
4 - 1.5 hrs
PT 1
• 1 Evals for 1 hour
• 4 – 1.5 hrs
•
•
•
•
•
•
•
•
•
•
•
•
•
•
7:00-8:00 Eval
8:00-8:20 Document Eval
8:30-8:50 Prep schedule/conferences next day
9:00-10:00 A
9:30-10:00 D
10:00-11:00 B
10:30 – 12:00 C
12:00-12:20 Document A, D, B
Lunch
1:00-2:00 D
1:30-2:00 A
2:00-2:30 B
2:30-3:15 Document C, D, A, B and order equipment, bill, update conference form for tomorrow
PT 2
•
1 Eval for 1.5 hrs
•
2 – 1 hrs
• 7:00-7:30 Eval hx and
ROM/Strength
• 7:30-8:30 1 hr
• 8:30-9:00 Prep for conferences
• 9:00-11:00 Conferences
• 11:00-12:00 1 hour
• 12:00-12:20 Document
• Lunch
• 1:00-1:30 Eval
• 1:30-2:30 Document
• 2:30-3:00 Eval
• 3:00-3:15 Document, bill
PT 3
• 4 - 1.5 hrs
•
•
•
•
•
•
•
•
•
•
•
•
8:00 – 8:30 Pt A
8:30-9:00 Document and Prep schedule and conference forms
9:00-10:00 Pt B
10:00 – 11:00 Pt C
11:00-12:00 Pt D
12:00-12:20 Document
Lunch
1:00-2:00 Pt A
1:00-1:30 Pt B
1:30-2:00 Pt C
2:00-2:30 Pt D
2:30-3:15 Document, update conference sheet, billing
Productivity
•
• Rehab: 4-6 pts per day
SNF: 6-10 pts per day
• Indirect Pt Care
• Documentation with FIM
• Walking to next area
•
• Cleaning Up
Communication Forms
•
•
•
3 hr Rule
Mobility
Conference/Weekly
• Ordering equipment
• Communication with other disciplines
• Obtaining other equipment
• Waiting on other disciplines
•
•
•
For chart
For speaking with pt
For care
Variables That Impact Productivity
• Type of clinical practice or program
• Physical space covered
• Case mix or payer mix attributes
• Receipts of skilled referrals (acute)
• ACO Accountable Care Organizations
• Relationship of entire continuum
• Cost reimbursement increase with good outcomes
Holding Therapy
• Why Hold?
• Medical Status
• Tests to R/O
• Pt refusal or pt deferment
• Use PT Decision Making
• Document what is happening
•
• If acute – why was pt not evaluated or treated
If rehab – counts why pt did not receive 3 hrs
• Place on hold and check on pt daily (or every other day pending status)
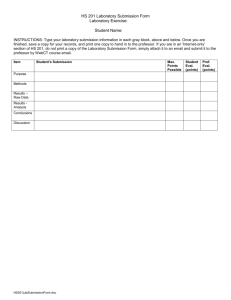
Billing
• Even though DRG, PPS or RUGS
• Use the 8 minute rule
•
•
•
•
•
Must see pt 8 minutes to bill
8-22 min = 1 unit
22-37 = 2 units
38-52 = 3 units
53-67 = 4 units
• Submit via computer or billing sheet
• Eval 15, Eval Med (30 min)
• Gt 15, Ther Ex 15, Neuromus Re-ed 30
•
•
•
•
Communication with Other Disciplines
Nursing
• Let RN know how pt did
• May demonstrate mobility with RN present
Physician
• Who wrote the order, who is the primary
• Rehab : pt is admitted by the physiatrist (PM&R)
•
•
See during the day
Blue Communication Form
• Page
• Office
Case Manager
• Discharge Planning
Social Worker
• Discharge to SNF or ECF
•
•
•
•
OT, SLP
Resp Ther
Dietician
Pharmacist
Rounds/Conferences
With Pt/Family Present
• Rounds in Acute
• Physician specialty
• Discuss pt case medical and physical
• Plans for current day
• Plans for discharge
• Conferences in Rehab/SNF
•
•
•
Physician, Therapies, Nursing, SW, Case Manager
Discuss pt progress and plans for goals
Discuss discharge
Working Side By Side With Nursing
• Flow Sheets
• Info not found in the chart
• Ask if Nsg has initiated mobility and how pt did with Nsg
• Notify when you see signs/symptoms or pt not responding as you planned
Co-Treatments with OT
• Acute
•
•
• Similar history, specific questions about mobility versus ADLs
OT screens UE, PT screens LE and trunk
•
Two people assist pt
PT performs bed mobility and transfer to chair, OT performs bathing/grooming, PT performs gait training, OT performs dressing while sitting
• Rehab/SNF
• Time must now be divided between disciplines
• Both must be performing skilled interventions
• Ex: Modified plantigrade position where PT is facilitating trunk and knee management while OT is facilitating UE stabilization and elbow management
Committees
• Rounds
• QI for specialty
• Total joint programs
• CVA programs
• Lifting
• Cost containment
• Team building
• Education
• Lifting
• Mobility
Students
• Clinical Instructor
• One year experience
• Teaching and Learning Principles
• Use of clinical environment
• Center Coordinator for Clinical Education
• CI for one year experience
• Organize the clinical experiences between schools and staff
• May be a CI along with CCCE
Equipment
• PT Dept Equipment/Area
• Parallel bars, NuStep, Wts, Theraband
• Assistive Devices
•
•
PT Dept versus Floor Equipment
Walker, w/c, canes, crutches, slide boards
• Hoyer Lifts
• CPM Machines
• Hospital Beds
• Medical Equipment
• Laundry
• Gowns, linen, wash cloths
• Patient care needs
• Basins, ADL items, footies
Signage
• Dry Erase Boards
• In room
• General mobility and assistance
• Signs outside of rooms
• Warning
• Signs inside room
• SLP Swallow Instructions
• Nursing No BP in L arm, pt blind
Family – Acute Care
• Ask pt if family may stay
• Need for training
• PT to determine if family interfering with PT session
• May ask family to wait in waiting area or go to cafeteria ~ 30 minutes
• Children should be asked to leave for session
• Ask pt how much info given to family
Family - Rehab
• Family is encouraged to join PT session
• Family training
• Family education
Transitional Apartment
Used to show pt/family can go home
Used to show pt/family cannot go home
Pt Refusal/Deferment
• Refusal
• States no therapy
• Right to refuse/Responsibility to follow physician recommendations
• Techniques
• Ask why and get to the root of the problem
• See if pt will try a small task to give pt confidence in self and in PT
• Team meeting
• Leave the door open
• Deferment
• States would like therapy to come at another time
• Techniques
• Ask what is the best time the pt would like therapy
• Sign a contract with PT
Eval
• Outcome Measurements
• FIM
• 3 or 6 min walk
• Gt speed
• 5 Rep sit to stand
• Dionne Egress Test
The Dionne Egress Test
•
•
•
Purpose: To facilitate the safe progression of a patient's debut transfer through repetitions.
Test 1:
• Three reps of sit-to-stand.
• The first rep in this progression is actually a clearing test, in which the patient elevates from and clears the support surface by only one to two inches. The purpose of the clearing rep is to verify weightbearing ability and that the patient is able to perform the task without physical assistance. The clearing test also allows the guarding caregivers to pause and request feedback verifying that all participants are safe during the initial rep.
• The patient then completes two subsequent full sit-to-stand reps to demonstrate consistency of physical antigravity performance. The total sit-to-stand progression demonstrates leg press ability and is critical to evaluate the ability to rise from the target surface, such as a bedside commode, during the return effort.
Test 2:
• Three steps of marching in place. There are situations in which a patient may have sufficient strength to raise a leg from the floor and advance it toward the target surface, but that same leg may lack the strength to support the patient's entire bodyweight.
• It is critical to test both the strength required to elevate each leg, and the ability of each leg to support the patient's total bodyweight during a single leg stance.
• Marching in place at the starting surface allows caregivers to test consistency and to redirect the patient back to a sitting position through the safe use of guarding techniques
Test 3:
• Advance step and return each foot. Before the patient is allowed to step away from the starting surface to the target surface, a last test of endurance and function must be performed. There are both orthopedic and neurological causes that may render a patient unable to step backward.
• While guarding positions are maintained at the bed's edge or starting surface, the patient is requested to advance one leg forward and then return it to the starting position. The task is repeated in the other leg.
• Should a patient be unable to retreat a leg, the caregivers cue the patient to shift backwards onto the trailing leg and sit. Note that the patient always has a trailing leg touching the starting surface for possible retreat in this last endurance test.
Assessment Evaluation
• LTG/STG – Patient Goals with PT input
• LTG(s) focus on broad functional tasks. They include an activity that the patient should be able to perform in a safe setting at home.
• Need to balance pt’s function, pt’s wishes activities of home
• STG(s) break the LTG down into pieces or numerous tasks that the therapist can work on individually. When the STG is met, it brings the patient closer to the LTG task.
• In acute settings, the LTG and STG may be the same goals for a patient with a relatively short stay which averages 4-7 days.
• In long term settings, there is usually a LTG set with a month time span and STG(s) are set for weekly time periods.
Assessment Daily/Progress
• Pt tolerated treatment – well, fair, poor
• Present signs and symptoms
• Absent signs and symptoms
• What changed or remained the same from the eval or the previous day?
• What goals progressed? Why?
• What did not progress? Why?
• Any change in equipment so ordering can take place?
• Any change in D/C destination?
38
Interventions: Communicate, Coordinate,
Documentation
•
Communicate
• With nursing pre/post PT services
• Obtain clarifying information
•
Coordinate
• Around daily routine (bath, bathroom, tests)
• With other disciplines (enhance specific instructions, observe pt compliance, co-eval or co-treat)
•
Document
• Immediately after 1-2 patients
Interventions: Patient Education
• Precautions
• Contraindications
• Signs and symptoms of infection
• Protection of incision/wound
• Use of equipment
•
•
When to contact physician or emergency
HEP – verbal or written
39
PT Examination/Interventions
Low Function
•
•
•
•
•
•
•
•
ROM
• PROM, AAROM, AROM (strength with gravity as assistance)
Manual
•
•
• Resisted isometrics or isotonics
Peripheral Joints – foot/ankle, Chest
Soft tissue
Sensory Stim
•
• Performed with movement
Joint compression
Splinting/Positioning
Pain Management
Breathing/Coughing
Mobility
•
• Bed mobility: rolling, bridging
Sitting: balance
Education
Interventions: Procedural Interventions
•
•
•
•
•
•
•
•
•
•
•
Mid to High Function
Ther Ex
•
•
ROM
Strength: use of manual resistance, theraband, cuff wts, sitting and standing targeted muscle groups
•
•
•
Aerobic
Locomotion: transfers and gait, wheelchair propel
Relaxation
Self Care
Work/Play
Assistive Devices/Adaptive Equipment
• Advanced Balance
Airway Clearance
Integument
Manual
Physical Agents
Electrophysical Agents
Functional Mobility – Gait, stairs
Outcome Measures
• Need to learn how to modify techniques or pt positions to achieve the goals of the exercise
41
![Please go to the following website [eval.franklin.uga.edu] and fill out](http://s3.studylib.net/store/data/008442817_1-afd5046c9c27af7ab7918658ed8da10d-300x300.png)