CNS Research - Wisconsin Association of Clinical Nurse Specialists

Descriptive Research
The Work of
Clinical Nurse Specialists in the Acute Care Setting
Julie Darmody MSN, RN, ACNS-BC
Doctoral Candidate, UW-Madison School of Nursing
Clinical Assistant Professor, UW-Milwaukee College of Nursing
Acknowledgements
This research was partially supported by:
• Nurses Foundation of Wisconsin Grant
• Helene Denne Schulte Research
Assistantship, UW-Madison School of
Nursing
Acknowledgements
• Mary Ellen Murray PhD RN (Advisor)
• Murray Research Team
– Mary Hook PhD, RN
– Roberta Pawlak MS, RN
– Yulia Semeniuk MS, RN
– Judy Westphal MSN, RN
– Nicole Bennett MS, RN
– Karin Kunz BS, RN
Purpose
Conduct a broad exploratory study that will describe the work of the CNS in acute care from multiple perspectives.
Objectives
Collect data on the following:
• organization characteristics
• job descriptions
• CNS activities and time
• perceptions of CNSs & Administrators about most important CNS activities and outcomes
Background
• Safety & quality are critical issues in health care
• CNSs have great potential to influence safety & quality in acute care
Significance
• Current increase in employment opportunities for the CNS in acute care
(Gerard & Walker, 2003; Sole, 2004)
• Challenges include a lack of understanding about the effect of CNS practice on patients, nurses, and systems
(Walker, et al, 2003)
Advanced Practice Nurses
National Sample Survey of RNs, 2004 http://bhpr.hrsa.gov/healthworkforce/reports/rnpopulation/preliminaryfindings.htm
CNS Practice
• The Clinical Nurse Specialist (CNS) is a masters-prepared advanced practice nurse who is a clinical expert in evidence-based nursing practice within a specialty area
(ANA, 2004)
• The Clinical Nurse Specialist (CNS) influences patients, nurses, and the organization to achieve quality, cost-effective outcomes (NACNS, 2004)
Framework for CNS Practice
• NACNS, 2004
Direct Patient / Client Care
Nurses
And
Nursing Practice
Organizations
And
Systems
Review of Literature:
Foundations of CNS Practice
• Foundation or core of CNS practice is clinical expertise with patients in a specialty area
(Sechrist & Berlin, 1998; Wilson-Barnett & Beech, 1994)
• Common features of developing practice models are that the CNS is a clinical expert who utilizes influence to improve patient outcomes
(Ball, 1999; Ball & Cox, 2003; Ball & Cox, 2004; NACNS, 1998;
NACNS, 2004)
Observing the work of the Clinical Nurse
Specialist: A Pilot Study
(Darmody, 2005)
• Purpose: develop a tool for recording the activities of CNSs using the NACNS Model
• Sample: n=5 CNSs in one acute care setting
• Method: Direct observation (4 hours/CNS =20 hrs)
• Results: CNS activity/time with
– Patients=30%
– Nursing personnel=44%
– Organization=10%
– Other Activities=16%
Design and Methods
• Descriptive Mixed Method Study
• Data Sources
– Multidimensional Work Sampling
(MDWS)
– CNS Questionnaire
– Administrator Questionnaire
– CNS Job Descriptions
Setting and Sample
• Four Health Care Organizations in the Midwest
• CNS Participants (n=30)
Masters prepared and employed in an acute care setting in a position titled CNS
• Administrator Participants (n=7)
Responsible for supervision and evaluation of CNSs in the organization
• Job descriptions (n=12)
Organization Characteristics
• Who do CNSs report to?
System-wide (n=1), hospital-wide (n=1), or multiple (n=2)
• Job Descriptions
Single (n=2) or Multiple (n=2)
• Structure of CNS Responsibility
– Majority are unit-based (n=1)
– Majority are population-based (n=2)
– Combination of unit and population-based (n=1)
CNS Characteristics (n=30)
• Age Range
30-39: 7 (23.3%)
40-49: 12 (40%)
> 50 : 11 (36.7%)
• Work Status (FTE)
Full-time: 22 (73.3%)
Part-time (0.5 to 0.9): 8 (26.6%)
• Average years of experience as CNS: 9.63 years
• Average years in current
CNS position: 6.08 years
• Responsibility
– Unit-based: 16 (53%)
– Population-based: 14 (47%)
CNS Characteristics (n=30)
• Specialty Patient Population
•
– Critical Care/Emergency: 4 (13.3%)
– Diabetes: 4 (13.3%)
– Geriatric: 3 (10%)
– Medical-Surgical: 13 (43.3%)
– Obstetric/Neonatal/Pediatric: 4 (13.3%)
– Pain & Palliative Care: 2 (6.7%)
Certification as Advanced Practice Nurse:
Yes: 19 (63.3%) No: 11 (36.7%)
Administrator Characteristics
(n=7)
• Position Titles: Varied including Director,
Assistant Vice-President, Vice President
• Education: All Masters prepared in Nursing or Business Administration
• Representation: At least 1 Administrator participant from each of the 4 organizations with several organizations having more than
1 participant
Recruitment & Data Collection
(Sept 2006 thru Jan 2008)
– E-mail recruitment messages to eligible CNS and Administrator Participants
– Group or individual meeting with researcher
– Return questionnaires and consents by mail
• Enrolled CNSs = 30 (33%)
• Enrolled Administrators = 7 (41%)
– CNS participants
• Training appointment
• Quiz #1 after training and Quiz #2 two weeks later
• Work sampling data collection until 240 data points
Job Descriptions (n=12)
• Framework
– NACNS model (17%)
– Sub-role or other framework (83%)
• Literature-based themes present
– Quality & Evidence-based practice consistently present
– Clinical & fiscal outcomes usually described in general terms
– Safety not included in majority of job descriptions
Random Work Sampling
• CNSs carried Random Reminder
Instrument (Divilbiss Electronics)
• Recorded work activity on checklist each time a random signal was received
• CNS Activity Checklist was developed in a pilot study (Darmody, 2005)
Random Work Sampling Results
• CNSs self reported 7,564 data points or observations during 518 work days and
4,216 hours
• CNS work days averaged 8.14 hours in length
• Each CNS subject recorded an average of
252 data points during 17.3 days and 140.6 hours of work
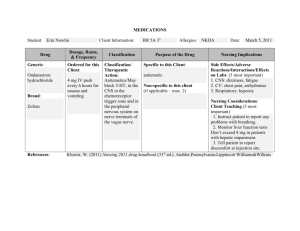
CNS Work Activity
CNS Work
Activity
Frequency Percent
2,172
95% Confidence
Interval
28.7% ± 1.02% (27.7-29.7%) Patients
Nursing 1,715
Organization 2,517
22.7%
33.3%
± 0.94% (21.7-23.6%)
± 1.06% (32.2-34.3%)
Other
Total
1,160
7,564
15.3%
100%
± 0.81% (14.5-16.1%)
Patient Activity
CNS Activity with Patients
Frequency Percent
Interdisciplinary Rounds
Patient Consultation
Coordination of Care
Direct Patient Care
Chart Review
Patient Teaching
Care Communication
Documentation
Brief Interaction
Nursing Rounds
417
305
287
285
256
180
129
123
86
56
5.51%
4.03%
3.79%
3.77%
3.38%
2.38%
1.71%
1.63%
1.14%
0.74%
Discharge Planning
Total Patient Activity
48
2,172
0.63%
28.71%
CNS Activity with Nurses
Nursing Activity
Nursing Education
Nursing Orientation
Nursing Question
Nursing Communication
Performance Evaluation
Total Nursing Activity
Frequency Percent
853
309
11.28%
4.09%
286
186
81
1,715
3.78%
2.46%
1.07%
22.67%
CNS Activity with the Organization/System
Organization Activity Frequency Percent
Committee Meeting
Quality Improvement
Problem solving
Protocol/Guideline Development
CNS Group Meeting
Organization Question
Safety
Education: Interdisciplinary
Product/Equipment Review
Program Development
Total Organization Activity
208
161
123
13
725
593
370
315
6
3
2,517
9.58%
7.84%
4.89%
4.16%
2.75%
2.13%
1.63%
0.17%
0.08%
0.04%
33.28%
Other CNS Activity
Other CNS Activity
Personal Time
Schedule/Calendar
Continuing Education (Self)
E-Mail Management
Scholarship: Write/Present
Research
Professional Organization
Total Other Activity
Frequency Percent
613 8.1%
399
64
5.27%
0.85%
40
20
14
10
1,160
0.53%
0.26%
0.19%
0.13%
15.34%
CNS Contacts
CNS Contact
Self (working alone)
Group Meeting
Nurse
Frequency Percent
2,843 37.59%
1,704
1,263
22.53%
16.7%
Patient
Manager
376
372
Provider (any non-nursing provider) 239
All other contacts 767
Total CNS Contacts 7,564
4.97%
4.92%
3.16%
10.13%
100%
CNS Work by Organization
Site Sample Patients Nursing Organization Other
Org
A
Org
B
Org
C
Org
D n=9 n=6 n=9 n=6
23.4%
47.8%
17.7%
35.4%
28.2%
11.7%
29.8%
14.2%
32.5%
27.9%
38.8%
31.0%
15.8%
12.5%
13.7%
19.4%
Most Important CNS Activities
(Likert Scale: 1=not at all important; 5=highly important
• CNS Perception (n=30)
• Develop clinical protocols & guidelines (4.467)
• Quality improvement projects (4.433)
• Nursing education (4.433)**
• Coordination of care (4.067)
• Nursing orientation (4.000)
• Administrator Perception
(n=7)
• Develop clinical protocols & guidelines (4.571)
• Rounds: Interdisciplinary
(4.429)
• Quality improvement projects
(4.286)
• Rounds: Nursing (4.143)
• Coordination of care (3.857)
** statistical significance
Most Important CNS Outcomes
(Likert Scale: 1=not at all important; 5=highly important)
• CNS Perception (n=30)
• Evidence-based nursing care (4.967)
• Skilled & competent nursing staff (4.800)**
• Patient satisfaction
(4.533)
**statistical significance
• Administrator
Perception (n=7)
• Skilled & competent nursing staff (5.000)**
• Evidence-based nursing care (4.857)
• Patient satisfaction
(4.429)
Summary & Conclusions
Random work sampling
• The NACNS model provides a useful framework
• Average proportions of CNS time spent in major work categories in the NACNS Framework:
• patients 28.7%
• nursing personnel 22.7%
• organization/system 33.3%
• other activities 15.3%
• Population-based CNSs spent a greater percent of time in activities with patients while unit-based CNSs spent a greater percent of time with nursing personnel.
Summary & Conclusions (cont)
Organization Characteristics
• This study revealed variations between organizations on
CNS job descriptions, reporting relationships, and how CNS responsibility is structured within the organization.
Perceived Importance of Activities and Outcomes
• Overall the most important activities and outcomes as perceived by CNSs and administrators were similar.
– CNSs placed significantly greater importance on the activity of nursing education and the outcome of patient knowledge
– Administrators placed significantly more importance on the outcome of skilled and competent nursing staff
Implications
• Link work activity to clinical and fiscal outcomes
“Explicit descriptions of the work of APNs are essential to understanding the process of care and empirically linking this to outcomes.”
Cunningham, R. (2004). Advanced practice nursing outcomes: A review of selected empirical literature.
Oncology Nursing Forum, 31(2), 219-230.
• Articulate the value of CNS practice
“Articulating how, why, and for whom they add value is critical to the future viability of the APN role and the delivery of quality healthcare services to the public.”
Cunningham, R. (2004). Advanced practice nursing outcomes: A review of selected empirical literature.
Oncology Nursing Forum, 31(2), 219-230.
Questions?
Comments?
Thank you!
Julie Darmody MSN, RN, ACNS-BC darmodyj@uwm.edu
Doctoral Candidate, UW-Madison School of Nursing
Clinical Assistant Professor, UW-Milwaukee College of Nursing