Precancerous lesion
advertisement

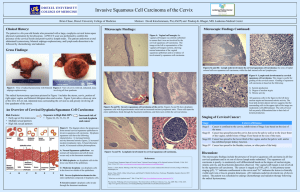
Precancerous lesion of FGT • Premalignant or precancerous lesions are epithelial changes of the FGT, which if left without treatment could progress (over an interval; may extend into several years) into carcinoma. The general features of precancerous cells Loss of stratification: loss of the normal arrangement of epithelial cells into layers. Distorted cells with enlarged irregular hyperchromatic nuclei. Increased Nuclear / Cytoplasm (N/C) ratio Nuclear mitosis are present at high level at the top layer more than the basal layers. Types of precancerous lesions Epithelial endometrial and cervical hyperplasia Leukoplakia: patches of keratosis. It is visible as adherent white patches on the mucous membranes. Atypical squamous metaplasia of the cervix Parakeratosis: mode of keratinization characterized by the retention of nuclei in the stratum corneum. Cervical dysplasia: abnormality of development show expansion of immature cells, with decrease in the number and location of mature cells. Endocervical polyp (Adenoma of the cervix) Cervical intraepithelial neoplasm (CIN) Epithelial hyperplasia Cervical hyperplasia Squamous cell hyperplasia: Thickness of the whole epithelium due to chronic irritation. Basal cell hyperplasia: Hyperactive proliferation of the basal cell layer to form several layers instead one or two layers. Reserve cell hyperplasia: Presence of patchy layer of small cells immediately beneath basal cell layer. Endometrial hyperplasia Endometrial hyperplasia is overgrowth of both glandular and stromal endometrial layers due to over- stimulation by estrogen . Types: Mild (cystic) hyperplasia (G I) Moderate (adenomatous) hyperplasia (GII) Sever (atypical) hyperplasia (GIII) Cervical smear: Thick clusters of reactive endometrial cells with or without atypia. N.B. Sever atypical endometrial hyperplasia is considered as GI (well differentiated) endometrial adenocarcinoma. Cervical atypical squamous metaplasia Definition: It is a transformation of the fragile cervical cells at the squamo-columnar junction of endocervical canal into more resistant stratified squamous epithelial cells with cellular atypia. Cervical smear: Squamous cells with a nuclear enlargement irregular (increased nuclear hyperchromasia. N/C ratio), membrane binucleated, and slightly Endocervical polyp (cervical adinoma) Definition: It is a pedunculated vascular connective tissue core containing inflammatory cells (acute & chronic), with dilated endocervical glands, and covered by ulcerated epithilium or squamous metaplasia cervical Cervical dysplasia Cervical intraepithelial neoplasia (CIN) Definition: It is an abnormal growth or disordered development of primitive immature basal cell layer and abnormal cell maturation; i.e. begin in the lower portion of cervical epithelium. Site: Usually at squamo-columnar junction ; it may be multifocal and involve the endocervical cleft. Features of cytological smears of dysplastic cells • Enlarged hyperchromatic nucleus ( N/C ratio). • Increased number of abnormal mitotic figures according to the severity of dysplasia • Nuclear chromatin clumping. Classification (types) of Dysplasia (CIN) Dysplasias are subclassified according to the degree by which the epithelium is replaced by immature dysplastic cells; Mild (GI) CIN dysplasia: involve the lower 1/3 of the cervical epithelium. Moderate (GII) CIN dysplasia: involve the lower 2/3of the cervical epithelium. Severe (GIII) CIN dysplasia or carcinoma in situ: involve the whole thickness of the covrring epithelium Cervical Disease Progression in Cells of the Basement Membrane LSIL HSIL Koilocytosis CIN1 Basement membrane Normal squamous epithelium Mild Koilocytosis - Cell changes showing perinuclear vacuolization LSIL - Low-grade Squamous Intraepithelial Lesion HGSIL or HSIL - High-grade Squamous Intraepithelial Lesion CIN2 CIN3 Moderate Severe Carcinoma in situ Dysplasia CIN - Cervical Intraepithelial Neoplasia CIN1 - Mild dysplasia CIN2 - Moderate dysplasia CIN3 - Severe dysplasia to carcinoma in situ (CIS) Precursor Lesions of Cervical Carcinoma LSIL CIN 1 Normal Mild Dysplasia HSIL CIN 2 CIN 3 Moderate Severe Carcinoma Dysplasia Dysplasia in situ Precancerous Lesions of the Cervix. LSIL = Low Grade Squamous Intraepithelial Lesion CIN = Cervical Intraepithelial Neoplasia HSIL = High Grade Squamous Intraepithelial Lesion • Above, left. Squamous carcinoma in situ (CIS), cervix. To the right is normal squamous epithelium with its basal cell layer & orderly maturation upwards. • The left side shows CIS characterized by lack of maturation, altered cell polarity, nuclear pleomorphism & increased nuclear / cytoplasmic ratio. • As is characteristic of CIS, neoplastic cells are confined to the epithelial layer & have not invaded through the epithelial basement membrane, under which, the submucosal stroma contains chronic inflammatory cells. A C B D Carcinoma of the cervix 1- Carcinoma in situ: • It is a lesion in which all thickness of cervical epithelium is replaced by malignant cells without invasion of the underlying stroma; i.e. with intact basement membrane. 2- Micro-invasive carcinoma • These are buds of malignant epithelial cells invading the cervical stroma beneath the carcinoma in situ to a depth of 2-3 mm from the site of the origin, without lymphatic or vascular invasion. 3- Invasive carcinoma • Malignant epithelial cells that invade the underlying stroma of the cervical epithelium by infiltration or destruction of the basement membrane, with or without lymphatic or vascular invasion. Types of invasive carcinoma Primary type • • • • Squamous cell carcinoma Adenocarcinoma Adeno-squamous carcinoma Adeno-acanthoma (squamous cell mataplasia + adenocarcinoma). • Choriocarcinoma (Malignant tumor of the placenta). Secondary type Metastatic Cytology of malignant cells Cytological features of normal and benign tumors The cells are uniform in size and shape. The cells are uniform in nuclear and cytoplasmic ratio. The normal C/N = ½ Normal polarity (normal arrangement of cells to neighbouring cells). In benign tumors, the appearance of cells are usually give normal appearance of origin cells; E.g. fibroma: show the increased number of normal appearance of fibroblasts. Cytological features of malignant tumors • A and B: mature squamous metaplasia. • C: immature squamous metaplasia. • D: immature squamous metaplasia with pattern of transitional metaplasia. Cervical dyskaryosis • Changes in nuclear-cytoplasmic ratio • Changes in nucleoli • Changes in mitotic index Severe dyskaryosis Atypical immature metaplastic squamous cells with increased nuclear/cytoplasmic ratio and hyperchromasia. Mild-moderate dyskaryosis Squamous carcinoma 1- Nuclear criteria Nuclear enlargement Nuclear shape and size variation Disturbed chromatin (abnormal chromatin distribution in the nucleus) Changes of nuclear membrane Irregular enlarged prominent nucleoli. Multinucleated malignant giant cells Abnormal mitosis Hyperchromasia: deep blue hyperchromatic nuclei due to increase DNA content of the nucleus. Enlarged nuclei with increased N/C ratio Enlarged nuclei with irregular nuclear membrane 2- Cytoplasmic criteria • Scanty cytoplasm • Increased N/C ratio • Tight holding of membrane around nucleus • Secretory or inclusion of cytoplasm 3- Malignant cells intrcellular relationship • Variation of the size and shape of malignant cells • Decreased cohesiveness between cells • Abnormal stratification and polarity General consideration about malignant criteria 1- No single morphologic malignant criteria alone is pathogenic for malignancy; a combination of criteria is necessary. 2- Nucleus is the most important part of the ell to show malignant changes; but the cytoplasmic changes could help in cell differentiation and cell typing. 3- The presence of acini or papillae in an abnormal location (such as in pleural cavity) -------- increase suspicion of malignancy even in absence of the prominent features of malignancy because of their high degree of differentiation. So, the question should always to be answered in this form: - It is a cancer? - What type of cancer is it? Factors affecting the distribution of malignant cells Collection and processing technique: Direct smearing or scraping ------ exfoliate malignant cells in clusters or sheets rather than isolated cells in spontaneous exfoliation (aspiration). Nature of the lesion: Adenocarcinoma -------- exfoliate malignant cells in clusters as acini or papillary structures. Dysplastic cells and carcinoma in situ of squamous cell carcinoma ----- single scattered exfoliated squamous cancer cells throughout the smear. Sarcomatous cells are usually arranged as single malignant cells and are separated by thin fibrous tissue.