Class #12 AO N405 MUSCULOSKELETAL DISORDERS

UNIT 4
Nursing Care of Clients With
Musculoskeletal Disorders
This Class:
Fractures: Types
Management & complications
Traction (Skin and Skeletal)
Casts (Compartment Syndrome, Infection,
Cast Syndrome)
Class Objectives:
Describe the anatomy and physiology of the musculoskeletal system including the significance of health history.
Discuss the significance of assessment and diagnosis of musculoskeletal problems including diagnostic tests.
Explain the pathophysiology, manifestations, complications & collaborative care of clients with fractures.
Describe the preventative health teaching needs of the client with a cast.
Describe the various types of traction and appropriate nursing care.
Class Objectives Cont’d:
Compare the nursing needs of the client undergoing a
THR with those undergoing a TKR
Discuss the etiology, pathophysiology, prevention and management of clients with osteoporosis.
Identfy the causes and related nursing management of osteomalacia and Pagets’s disease.
Discuss the pathophysiology, manifestations, complications & collaborative care of clients with arthritis, gout, spinal cord deformities, septic arthritis .
Readings:
– Read in your text Chapters 66, 67, 68, &
69
– Recommended readings
– Bibliography list
– Fractures
Fractures
•Read text content dealing with fractures
•Know what a closed, open,displaced comminuted, impacted, & greestick fractures are.
•Note the risk factors & levels of prevention r/t #
•Review the stages of healing
•Know neuromuscular assessment
•What causes muscle spasm following #s and what are the consequences?
A fracture is “any disruption in the continuity of the bone, when more stress is placed on it than it can absorb”.
(Black, Hawkes & Keene, 2001, p587).
When # occurs, muscles are also disrupted & pull fracture fragments out of position.
Adjacent structures are affected – soft tissue edema, hemorrhage, joint dislocations, ruptured tendons, severed nerves, damaged blood vessels
Large muscle groups create massive spasms, the proximal portion remains intact while the distal portion can be displaced in response to force and spasm.
FRACTURES
Classification of Fractures:
(See Chart 69-1)
Open: (compound or complex) break in tissue over site of the bone injury
Complete: break across entire cross-section of bone & often displaced
Incomplete: (greenstick) though only part of the cross-section
Closed: (simple) intact skin over site of injury
Comminuted: produces several bone fragments
Physical Assessment may reveal :
– Deformity (hemorrhage or spasm)
– Shortening
– Swelling
– Ecchymosis
– Muscle spasm
– Pain, tenderness
– Loss of function, altered mobility & crepitus
– Neurovascular changes
– shock
Signs and Symptoms
Complications
Fat Embolism Syndrome
Fat globules (emboli) occlude small vessels of lungs, brain, kidneys, & other organs
Characterized by neurologic dysfunction, pulmonary insufficiency, and petechial rash on chest, axilla & upper arms
Long bone # & other major trauma ( such as
THR) are the principle risk factors
Most frequently in young adults (20-30 years of age)
Fat Embolism Syndrome What to
Look for:
Manifestations of fat emboli occur within 24-72 hours but may be up to a week after injury:
– Hypoxia PaO2 < 60 mm Hg
– Tachypnea, tachycardia, pyrexia
– Deterioration in LOC
– Confusion , agitation
– Respiratory distress response – tachypnea, dyspnea, crackles, wheezes, precordial chest pain, copious thick white sputum, tachycardia
– petechiae: chest, shoulders, axilla, mouth, conjunctival sac
Fat Embolism:
Prevention:
– Immobilize fractures: early & gentle stabilization
– Gentle care
– Adequate hydration
– O2
– Aware of those at high risk
Management:
– O2
– Fluid replacement
– Mechanical ventilation
– Corticosteroids
– Vasoactive medications
– Maintain Hgb
– Calm, supportive environment
Monitor Respiratory Status Every
Shift .
Immobility increases risk for Atelectasis,
DVT and Pulmonary Emboli.
Never ignore client's complaints.
Follow-through and check it out.
Fifty percent (50%) of persons with fat emboli die.
Complications
Infection
Musty, unpleasant odor over cast and/or at the ends of cast
– Drainage through cast or cast opening
– Sudden unexplained body temperature elevation
– “Hot Spot” felt over cast lesion
– May result in osteomyelitis
Interventions: Infection
Wash hands
Use aseptic technique when caring for wound and emptying drains
Culture drainage
Foley catheter care
Monitor temp
Report excessive drainage or inflammation to physician
Complications
Watch out for Deep Vein Thrombosis after skeletal or muscular injury/surgery!
Muscle Spasm :
Powerful involuntary muscle contractions shorten the flexor muscles & cause extreme pain. This may be triggered by hypoxia of muscle tissue.
What Helps?
Bed cradle
Heat
Avoid heavy sedation
Avoid pressure in popiteal space
Minimize compression
Active & passive exercises as ordered
Frequent change in position
Fracture: Early Complications
Critical monitoring & assessment is imperative. Know assessment findings that may indicate one of the following early complications of fractures. Question waiting for a place to happen
!!!!
Shock
Nerve damage, arterial damage
Infection
Cast syndrome
Compartmental Syndrome
Volkmann’s Contracture
Fat Embolism Syndrome
Deep Vein thrombosis & Pulmonary Embolism
Long-term Complications
Joint stiffness or post-traumatic arthritis
Avascular necrosis
Nonfunctional union after a fracture
Complex regional pain syndrome
Reaction to internal fixation device
Avascular Necrosis
Complications of Fractures:
Shock
Bones are very vascular. In combination with collateral damage to adjacent structures/vessels, the patient is at risk for hemorrhage.
Shock fully develops if a healthy client loses 1/3 of normal blood volume.
Blood loss :
15-30% (up to 1500 ml) -subtle signs
30-40% (1500-2000 ml) –obvious shock
Over 40% (over 2000 ml)
1 unit of packed cells raises Hgb about 1 gram. Check with physician about expected normal loss.
Potential Blood Loss Following
Fractures (Liters)
Humerus
Elbow
Forearm
Pelvis
Hip
Femur
Knee
Tibia
Ankle
Spine/ribs
1-2
.5-1.5
.5-1
1.5-4.5
1.5-2.5
1-2
1-1.5
. 5-1.5
.5-1.5
1-3
This is not what is expected but what is possible!
See Text
1) Compartment Syndrome
2) Cast Syndrome
3) Infection
What?
How to recognize?
What should be done?
Fracture Reduction
Closed reduction : usually done under anesthesia
– Carried out through manual traction to move fracture fragments & restore bone alignment
Followed by immobilization device (cast)
Open Reduction: incision and realignment
– Usually performed with internal fixation devices
(screws, pins, plates, wires)
Closed vs. Open Reduction
Open
Reduction
Fracture Reduction Cont’d
External Fixation: maintain position for unstable fractures & for weakened muscles, allow for use of contiguous joints while affected part remains immobilized. Common sites include face & jaw, pelvis, fingers.
Traction: application of a pulling force to an injured body part or extremity while a counter-traction pulls in the opposite direction.
External fixation
Figure 27-3: Types of Internal
Fixation Devices
Open reduction and internal fixation of Comminuted mandibular fracture
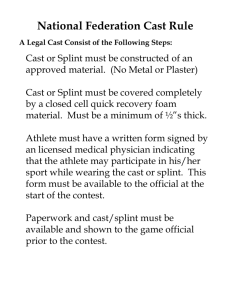
CASTS
•Review information learned in 2nd & 3rd year. At this point you should know
•Types of casts
•
•
• Why a cast may need to be Bi-valved
Drying & caring for a cast
Complications caused by casts …
•Management of Casts & Braces
•Importance of knowing weight bearing status
Windowing and Bivalving a Cast
Windows maybe cut in dried casts:
1. relieve pressure from abd. distension (body cast)
2.
To prevent “Cast Syndrome”
3. To assess radial pulse (check circulation in a casted arm)
4. To inspect areas of discomfort or areas of suspected tissue damage
5. To remove drains or care for wounds.
Bivalving a Cast Window Cast
Cast Drying:
Synthetic casts – dry approx. 20-30 mins (clients feel the sensation of heat thus may feel hot).
Plaster casts set rapidly but take several hrs-days to completely dry (lg. cast).
Promote the circulation of warm, dry air around a damp cast to enhance moisture evaporation and speed drying process.
Heat occurs with early cast drying stages
Do not cover cast while drying, can place layers of towels underneath pillow to elevate cast to absorb dampness.
Green cast (damp cast)
Lg. cast avoid covering and to allow air to circulate
Never use heated hairdryer to dry cast.
Nerve Damage during casts/traction:
Traction applied to an extremity puts pressure on the peroneal nerve where it passes around the neck of the fibula to just below the knee.
Pressure at this point may cause footdrop, leading to inability to dorsiflex the foot.
Inability to plantarflex indicates damage to the tibial nerve.
The calf muscle is not affected & the temp of extremity doesn’t change.
Assess for complications following cast :
Compartment syndrome
Fat emboli
Infection
DVT
Cast syndrome
Complications of Fractures/Casts
Compartmental Syndrome :
Edema from a fracture causes an increase in compartmental pressure that decreases capillary blood perfusion.
When the local blood supply unable to meet tissue metabolic demands ischemia begins = compromised circulation.
Increase pressure in a confined space due to tight cast, edema or bleeding.
Complications of Fractures/Casts
Compartmental Syndrome:
– Pulselessness: slow nail bed capillary refill
(>3sec)
– Skin pallor, blanching, cyanosis or coolness
– Increasing pain, swelling,pain on passive motion, painful edema peripheral to cast.
– Paresthesias (tingling, pricking), heightened sensation to touch, diminished sensitivity to touch (hypesthesia), anesthesia (numbness)
– Motor paralysis to previous functioning muscles
Compartmental Syndrome
Swelling out of control
Compartment Syndrome Treatment
Fasciotomy
CUT OPEN
RELEASE PRESSURE RELIEF
Complications Cont’d
Figure 27-6: Cast Syndrome
Cast syndrome results from the compression of the duodenum between the aorta and the superior mesenteric artery. The external compression is usually caused by a tight body cast.
Complications Cont’d
Cast Syndrome:
Bloating feeling
– Prolonged nausea: repeated vomiting
– Abdominal distension: vague abdominal pain
– Shortness of breath
– Untreated may lead to death!
Cast Syndrome
An abdominal flat-plate is ordered. If you diagnosed the cast syndrome, you correctly identified the clinical signs consistent with this syndrome. This is due to an extrinsic compression of the third portion of the duodenum by the superior mesenteric artery
Other Complications Cont’d
Infection:
Musty, unpleasant odor over cast and/or at the ends of cast
– Drainage through cast or cast opening
– Sudden unexplained body temperature elevation
– “Hot Spot” felt over cast lesion
– May result in osteomylitis
Complications Cont’d
Volkmann’s Contracture:
A common complication of elbow fractures
Can result in unresolved compartment syndrome. Arterial blood flow decreases, leading to ischemia, degeneration & contracture of muscle
May lead to permanently stiff, claw-like deformity of arm & hand
Volkmann’s Contracture
Complications Cont’d
FAT EMBOLISM:
Fat emboli occur when fat globules lodge in the pulmonary vascular bed or peripheral circulation. Fat embolism syndrome (FES) is characterized by neurologic dysfunction, pulmonary insufficiency, and petechial rash on chest, axilla & upper arms. Long bone #
& other major trauma ( such as THR) are the principle risk factors
Fat Embolism: Beware!!
When a bone is fractured, pressure within the bone marrow rises & exceeds capillary pressure; fat globules leave the marrow & enter bloodstream, it may also be caused by the stress induced release of catecholamine, which causes the rapid immobilization of fatty acids.
Once fat globules are released they travel to the brain, kidney, lung & other organs, occluding small blood vessels - - causing ischemia.
Fat Emboli:
Fat globules within the pulmonary arterioles. The globules stain reddish-orange.
The cumulative effect of these globules is similar to a large pulmonary embolus, but the onset is usually 2 to 3 days following the initiating event, such as the trauma associated with bone fractures.
Monitor respiratory status every shift
.
Nurse Alert:
Immobility increases risk for fat embolism, atelectasis, and pulmonary emboli. Never ignore client's complaints. Follow-through and check it out.
Fifty percent 50% of persons with fat emboli die.
WHAT TO LOOK FOR:
Manifestations of fat emboli occur within a few hours to weeks after injury:
– deterioration in LOC
– confusion , agitation
– SOB
– petechiae: Chest, axilla, mouth, conjunctival sac
– atelectasis may result
– signs of shocktachycardia, tachypnea
– Hypoxia Po2 < 60 mm Hg
Fat Embolism:
Fat globulins released from long bone pelvis or multiple fractures
Prevention:
– Immobilize fractures: early & gentle stabilization
– Gentle care
– Adequate hydration
– O2
Management:
O2
Fluid replacement
Mechanical ventilation
Corticosteroids
Maintain Hgb
Corticosteroids
Complications Cont’d
Neuro-vascular problems
Early detection may mean no or slight disability in the future. Assess carefully & knowingly!
Who is at Risk for Neurovascular Problems?
Those with/who:
External fixators
Interstitial edema/bleeding
Excessive exercise
Trauma to joint/limb
Casts, Splints, Constrictive Dressings
Medical Procedures (heart cath)
Traction
Spinal Surgery/injury
Tissue compression
KNOW the SIX Ps: Cast
Assessment
P ain
P allor
P aresthesia
P ulselessness
P aralysis
P olar
Compartment
Syndrome??
Infection??
Cast Syndrome??
Assess
Monitor neurovascular status of distal aspects of involved extremities in comparison with corresponding body part after the initial post op period & every 2 hours for the following 24 hours and every 4 to 12 hours thereafter
(according to agency policy).
Nurse Alert: Irreversible tissue death occurs in 4 to 12 hours.
Inspect color and temperature.
Monitor for edema caused by tissue trauma or venous stasis.
Assess capillary refill by pressing on toe or fingernail, releasing, and noting "pinking" on nail within 3 seconds
Complications Cont’d
Watch out for Deep Vein
Thrombosis after skeletal or muscular injury/surgery!
Hemorrhage: Know what it means!
Stage I up to 15% (up to 750 ml)
Stage II 15-30% (up to 1500 ml) -subtle signs
Stage III 30-40% (1500-2000 ml) –obvious shock
Stage IV over 40% (over 2000 ml)
Complications Cont’d
Blood Loss in Fractures
• Bones are very vascular. In combination with collateral damage to adjacent structures/vessels, the patient is at risk for hemorrhage.
• Shock fully develops if a healthy client looses 1/3 of normal blood volume.
• 7 - 8% of body wt is blood. An adult has about 5.5 L of blood.
• 10% volume loss = tachycardia
• 30% loss affects B.P
• 1 unit of packed cells raises Hgb about 1 gram. Check with physician about expected normal loss.
Potential Blood Loss Following
Fractures (Liters)
Humerus
Elbow .5-1.5
Forearm .5-1
1-2
Pelvis 1.5-4.5
Hip 1.5-2.5
Femur 1-2
Knee 1-1.5
Tibia .5-1.5
Ankle .5-1.5
Spine/ ribs 1-3
This is not what is expected but what is
Check with surgeon to determine extent of possible!
expected blood loss
Watch for Blood loss post op
For Example
In the client with a total hip replacement
(THR) the total amount of drainage is usually less than 50 ml every 8 hours, it may be a bit more if the client received a plasma expander such as dextran.
Drains are usually removed within 48-72 hours post surgery.
Muscle Spasms Interventions:
Powerful involuntary muscle contractions shorten the flexor muscles & cause extreme pain. This may be triggered by hypoxia of muscle tissue.
• What helps?
• Bed cradle
• Heat
• Avoid heavy sedation
• Avoid pressure in popliteal space
• Minimize compression
• Active & passive exercises as ordered
• Frequent change in position
Interventions: Infection
Wash Hands.
Use aseptic technique when caring for wound and emptying drains.
Culture drainage.
Foley catheter care
Monitor temp.
Report excessive drainage or inflammation to physician.
Intervention: DVT/PE/FES
Client wears elastic stockings.
Teach leg exercises.
Observe for changes in mental status, chest pain and SOB.
Observe for swelling, redness and pain in legs (DO NOT MESSAGE).
Fat embolism is the most lethal complication of THR.
Interventions: Bleeding
Vitals q4h.
Assess for bleeding.
Report excessively low BP.
Intervention: Pain Management
Encourage client to report hip pain immediately.
Promote adequate rest through out the day.
Administer oral analgesics PRN.
Traction
•What is used traction for?
•What is the difference between Skeletal & Skin traction?
•What would the nurse assess for that is particular to each type?
•Differentiate between the following types of traction & give an example of each:
•Continuous & Intermittent
•Running & Suspension
•Skeletal/ Skin/ Cervical
•Russell’s & Buck’s
Traction serves several purposes:
It aligns the ends of a fracture by pulling the limb into a straight position.
It ends muscle spasm.
It relieves pain .
It takes the pressure off the bone ends by relaxing the muscle.
Skin Traction:
http://www.youtube.com/watch?v=2ZEWz_Ps7vo
Apply traction to underlying bones and other structures (muscles).
Used :
1. with commercially prepared foam slings
2. by encircling a body part with a halter, corset or sling.
Counteraction is provided by a persons wt. when the bed is tilted away from the pull.
Buck’s SKIN TRACTION
Skin traction uses 5 to 7 pound weights attached to the skin to indirectly apply the necessary pulling force on the bone. If traction is temporary, or if only a light or discontinuous force is needed, then skin traction is the preferred treatment. Because the procedure is not invasive, it is usually performed in a hospital bed.
Skeletal Traction:
Is accomplished by surgically inserting metal wires or pins thru distal bones to the # site or by anchoring metal tongs in the skull.
A traction bow is attached to wire or pin and traction force is applied .
Used to reduce unstable fractures of long bones
Skeletal traction is performed when more pulling force is needed, or when the part of the body needing traction is positioned so that skin traction is impossible. Skeletal traction uses weights of 25-40 pounds. It requires the placement of tongs, pins, or screws into the bone so that the weight is applied directly to the bone. This is an invasive procedure that is done in an operating room under general, regional, or local anesthesia.
Thomas Splint Picture
http://www.scribd.com/doc/12356898/Balance
-Skeletal-Traction
Skin Traction
Advantage:
Relative ease of use and ability to maintain comfort
Disadvantage:
Wt required to maintain Normal body alignment or fracture alignment can not exceed 6 lbs per extremity.
– Skeletal Traction
– Advantage:
– Increases mobility without threatening joint continuity.
Easier to change linen, backcare
Disadvantage:
Need to use multiple wts makes client slide in bed more.
Bucks
The main risks associated with skin traction are that the traction will be applied incorrectly, or that the skin will become irritated.
More risks associated with skeletal traction.
– Bone inflammation.
– Infection can occur at the pin sites.
Both types of traction have complications associated with long periods of immobility:
– bed sores
– reduced respiratory function
– urinary & and circulatory problems
– occasionally, fractures fail to heal
– emotional toll of prolonged bedrest
– Kidney/gallstones
More about traction
Positioning the extremity so that the angle of pull brings the ends of the fracture together is essential. Weights must hang freely
Elaborate methods of weights, counterweights, and pulleys have been developed to provide the appropriate force, while keeping the bones aligned and preventing muscle spasm.
The patient's age, weight, and medical condition are all taken into account when deciding on the type and degree of traction.
Check the four P's of traction maintenance:
Pounds: Inspect traction setup. Is the correct weight in place?
Pull: Is the direction of pull aligned with the long axis of affected bone?
Pulleys: Is the rope gliding smoothly over pulley?
Pressure: Are clamps and connections tight?
Assess, Assess, Assess
Assess client's knowledge of the reason for traction, including nonverbal behavior and responses.
Assess integrity and condition of skin over bony prominences and under devices in use.
Assess client's overall health condition, including degree of mobility, ability to perform ADLs, and current medical conditions.
Assess client's level of pain and need for analgesics before procedure begins.
Assess for respiratory dysfunction
USUAL PIN SITE CARE
With gloves remove gauze dressings from around pins
Inspect sites for drainage or inflammation.
Prepare supplies and apply new gloves.
Clean each pin site with NaCl by placing sterile applicator close to the pin and cleaning away from the insertion site. Dispose of applicator.
Continue process for each pin site.
Using a sterile applicator, apply a small amount of topical antibiotic ointment as ordered
Provide pin site care according to hospital policy/
Dr. orders.
Cover with a sterile 2 X 2 split gauze dressing or leave site open to air (OTA) as prescribed
More care for traction client
Assess level of discomfort and provide nonpharmacological and pharmacological relief as indicated.
Encourage active and passive exercises and use of unaffected extremities for ADLs.
Encourage us of trapeze bar for repositioning in bed.
Provide a fracture pan for elimination prn
Evaluate effectiveness of care & need for intervention
Care of the Client in Traction
•When caring for a client in continuous, balanced, skeletal traction with a Thomas Splint what should the nurse know? Wow, what a question!
•Consider skin, infection, personal care,
ROM/exercises
•Care of ropes, pulleys
•What to do when transporting client/bed elsewhere
Nerve damage during traction
•Traction applied to an extremity puts pressure on the peroneal nerve where it passes around the neck of the fibula to just below the knee.
•Pressure at this point may cause footdrop, leading to inability to dorsiflex the foot.
•Inability to plantarflex indicates damage to the tibial nerve.
•The calf muscle is not affected & the temp of extremity doesn’t change.
Specific Fractures
Hip Fractures
Condylar fractures
Pelvic fractures
Patellar fractures
Tibial & fibular fractures
Foot fractures
Upper extremities
Please review Pages 607-619 for care of specific fractures
Sports Injuries
Common Overuse injuries:
– Lower Extremities:
Stress fractures (common in tarsal bones)
Plantar fasciitis (damage of long ligament that attaches to the sole of the heal bone)
Shin splints (medial tibial area)
Patellar tendinitis (jumper’s knee)
– Upper Extremities
Tennis elbow
Tendinitis (hand & wrist)
– Strains & sprains
Sports Injuries Cont’d
Rotator cuff tears
– Shoulder muscle injury
Anterior cruciate ligament injuries
– Tear of ACL
Meniscal injuries
Arthroscopy
Same day surgery.
Mostly preformed on knee and shoulder by use of a fibroptic arthoscope
Candidates for surgery are people who can flex their joint greater than fourty degrees and the joint is infection free.
Used for obtaining a Biopsy, assessing cartilage, removing loose bodies & trimming cartilage.
Infection is the major complication to arthroscopy.
Complications of Arthroscopy:
Infection
Blood in joint (hemarthrosis
Swelling
Synovial rupture
Joint injury
Thrombophlebitis.
By the time a person presents with complaints of numbness, paresthesias, pain, or motor deficit, nerve damage has progressed to the stage of larger fiber sensory and/or motor loss.
The median nerve shares confined space with nine flexor tendons as it travels through the carpal tunnel. Any condition which reduces that space is likely to cause CTS due to compression of the vulnerable median nerve.
Any solution which relieves pressure on the nerve and promotes circulation in the microvascular neural blood supply is likely to "cure" CTS and relieve its attendant symptoms of pain, etc.
DUPUYTREN'S CONTRACTURE
A painless thickening of the connective tissue in the palmar hand that can lead to difficulty extending the digits. Causes include hand trauma and genetic predisposition.
Painless nodule on the palm,
Cord-like bands across the palm & thickening of the lines of the palm, and curling (contracture) of the 4th and 5th digits.
Surgery is performed in some cases unresponsive to conservative measures such as (splinting, warm soaks, exercises).
Neurovascular Assessment:
Questions to Consider:
1. Discuss why neurovascular assessment is so important. Your answer should include consideration of the three components of neurovascular assessment:
Circulation, Motor Function, & Sensation , as well as discussion of the 6Ps of neurovascular assessment.
2.Who is most at risk for problems of the peripheral nervous system/blood flow?
Explanation
A loss of the bone’s blood supply causes avascular necrosis (AN) - the bone dies & bone structure collapses . Femoral neck fractures which damage local blood vessels, increase the risk of avascular necrosis. Long term high dose steroids also increase risk. Symptoms of AN include pain & reduced ROM in affected joint. Heparin, Lasix &NSAIDs aren’t associated with AN.