Bacterial Diseases
advertisement

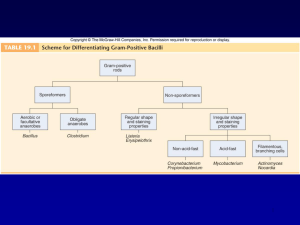
Bacterial Diseases Gram-positive Gram-negative Rickettsias, Chlamydias, Spirochetes and Vibrios Bacterial Diseases Classified by: Airborne Upper Lower Foodborne Waterborne Soilborne Arthropodborne Physical Contact STD Contact Animal Or by….. Physiological properties: Catalase Hydrogen peroxide water Oxidase Water hydrogen peroxide Peroxidase Breakdown peroxidase (by-products that cause tissue damage) Or, by…….. Gram-positive Gram-negative Rickettsias, Chlamydias, Spirochetes and Vibrios Gram-positive bacteria Staphylococcus aureus Capsule! grows in large, round, opaque colonies optimum temperature 37oC facultative anaerobe withstands high salt, extremes in pH, & high temperatures produces many virulence factors Coagulase coagulates plasma and blood produced by 97% of human isolates Hyaluronidase promotes invasion Staphylokinase digests blood clots Dnase digests DNA Lipases helps bacteria colonize oily skin Penicillinase inactivates penicillin Enzymes of S. aureus Toxins of S. aureus hemolysins lyse RBCs Leukocidin damages cell membranes Enterotoxins act in the gastrointestinal tract exfoliative toxin separates epidermal layers toxic shock syndrome toxin (TSST) Epidemiology and Pathogenesis Present in most environments frequented by humans Readily isolated from fomites Carriage rate for healthy adults is 20-60% mostly in anterior nares, skin, nasopharynx, intestine Predisposition to infection include: poor hygiene and nutrition, tissue injury, preexisting primary infection, diabetes, immunodeficiency Increase in community acquired methicillin resistance MRSA Staphylococcal Disease - 1 Localized cutaneous infections – invade skin through wounds, follicles, or glands folliculitis superficial inflammation of hair follicle usually resolved with no complications but can progress furuncle Boil inflammation of hair follicle or sebaceous gland progresses into abscess or pustule carbuncle larger and deeper lesion created by aggregation and interconnection of a cluster of furuncles impetigo bubble-like swellings that can break and peel away most common in newborns Staphylococcal Disease - 2 Systemic infections osteomyelitis infection is established in the metaphysis abscess forms bacteremia primary origin is bacteria from another infected site or medical devices endocarditis possible Staphylococcal Disease - 3 Toxigenic disease food intoxication ingestion of heat stable enterotoxins gastrointestinal distress staphylococcal scalded skin syndrome toxin induces bright red flush, blisters, then desquamation of the epidermis toxic shock syndrome toxemia leading to shock and organ failure Other Staphylococci S. epidermidis lives on skin & mucous membranes endocarditis, bacteremia, UTI S. hominis lives around apocrine sweat glands S. capitis live on scalp, face, external ear S. saprophyticus infrequently lives on skin, intestine, vagina; UTI Streptococci Gram-positive spherical/ovoid cocci arranged in long chains Non-spore-forming, nonmotile Can form capsules & slime layers Facultative anaerobes Sensitive to drying, heat & disinfectants 25 species Streptococci Lancefield classification system based on cell wall Ag 17 groups (A,B,C,….) Another classification system is based on hemolysis reactions b-hemolysis A,B,C,G & some D strains a –hemolysis S. pneumoniae & others collectively called viridans γ-hemolysis Enterococcus faecalis does not induce hemolysis Streptococci Skin infections Impetigo (pyoderma) superficial lesions that break and form highly contagious crust often occurs in epidemics in school children associated with insect bites, poor hygiene, and crowded living conditions Erysipelas pathogen enters through a break in the skin eventually spreads to the dermis and subcutaneous tissues can remain superficial or become systemic Throat infections Streptococcal pharyngitis strep throat b-hemolytic S. pyogenes Most serious streptococcal pathogen Inhabits throat, nasopharynx, occasionally skin Produces Ccarbohydrates, M-protein (fimbrae), streptokinase, hyaluronidase, DNase, hemolysins S. pyogenes GAS Produces toxins Humans only reservoir Transmission contact, droplets, food, fomites Skin infections pyoderma, impetigo, erysipelas Systemic infections strep throat, pharyngitis, scarlet fever S. pyogenes Causes streptococcal pharyngitis Strep throat enters the upper respiratory tract through respiratory droplets Some patients with strep throat may develop scarlet fever exhibiting a rash caused by erythrogenic exotoxins S. pyogenes Rheumatic fever serious complication affecting the joints and heart causes permanent heart damage called rheumatic heart disease Acute glomerulonephritus rare inflammatory response to M proteins may lead to renal damage Group B: S. agalactiae Regularly resides in human vagina, pharynx & large intestine wound and skin infections & endocarditis in debilitated people can be transferred to infant during delivery & cause severe infection Most prevalent cause of neonatal pneumonia, sepsis, & meningitis Targets infants without Ab, and mothers that do not provide passive immunity Pregnant women should be screened & treated “Typical” Pneumonia Can Be Caused by Several Bacteria: 80% of “typical” pneumonia cases are caused by Streptococcus pneumoniae Others: Haemophilus influenzae Staphylococcus aureus Klebsiella pneumoniae Streptococcus pneumoniae Small, lancet-shaped cells arranged in pairs and short chains Culture requires blood or chocolate agar Growth improved by 5-10% CO2 Lack catalase & peroxidases cultures die in O2 S. pneumoniae All pathogenic strains form large capsules major virulence factor Vaccine available for high risk people S. Pneumoniae Epidemiology 5-50% of all people carry it as normal flora in pharynx Does not survive long outside of its habitat Pneumonia occurs when cells are aspirated into the lungs of susceptible individuals Pneumococci multiply induce inflammatory response Traditionally treated with penicillin G or V Increased drug resistance Cultivation and Diagnosis Gram stain of specimen presumptive identification α hemolytic Quellung test or capsular swelling reaction Bacillus gram-positive endospore-forming motile rods mostly saprobic primary habitat is soil versatile in degrading complex macromolecules source of antibiotics 2 species of medical importance Bacillus anthracis Bacillus cereus Bacillus anthracis facultative large, block shaped rods central spores develop under all conditions except in the living body virulence factors capsule & exotoxins Bacillus anthracis 3 types of anthrax Cutaneous spores enter through skin, black sore least dangerous Pulmonary inhalation of spores Gastrointestinal ingested spores treated with penicillin or tetracycline http://www.youtube.com/watch?v=mi3sYzDsSGI Bacillus cereus common airborne & dustborne grows in foods, spores survive cooking & reheating ingestion of toxin-containing food causes nausea, vomiting, abdominal cramps & diarrhea 24 hour duration no treatment spores abundant in the environment Clostridium gram-positive spore-forming rods Anaerobic 120 species oval or spherical spores produced only under anaerobic conditions cause wound & tissue infections and food intoxications C. difficile C. botulinum C. perfringens C. tetanis Clostridium difficile-Associated Disease (CDAD) Normal resident of colon, in low numbers Causes antibiotic-associated colitis relatively non-invasive treatment with broad-spectrum antibiotics kills the other bacteria allowing C. difficile to overgrow Produces enterotoxins that damage intestines Major cause of diarrhea in hospitals Increasingly more common in community acquired diarrhea Clostridium botulinum Anaerobic, endospore-forming, Gram-positive bacillus Common in soil and water Botulism results when the endopsores germinate and produce botulism toxins Clostridium botulinum Causes 3 diseases 1. food poisoning o o spores are in soil, may contaminate vegetables improper canning does not kill spores & they germinate in the can producing botulinum toxin toxin causes paralysis by preventing release of acetylcholine 2. infant botulism o caused by ingested spores that germinate & release toxin 3. wound botulism o spores enter wound & cause food poisoning symptoms Clostridium botulinum Diagnosis Symptoms are diagnostic Treatment Administer neutralizing antibodies against botulism toxin Administer antimicrobial drugs in infant botulism cases Prevention Proper canning of food Infants under 1 year should not consume honey Clostridium perfringens Gangrene Mass of body tissue dies (necrosis) Usually occurs when blood flow ceases to a part of the body Types : Gas gangrene (myonecrosis) caused when spores enter the body through a severe open wound Dry gangrene Wet gangrene Clostridium perfringens Vegetative cells ferment muscle carbohydrates and decompose muscle proteins Large amounts of gas accumulate under the skin causing a crackling sound a-toxin damages and lyses blood cells Treatment involves: Antibiotics tissue debridement Amputation exposure in a hyperbaric oxygen chamber Clostridium tetani Tetanus Causes hyperactive muscle contractions Spores can enter the body through a wound produce toxins • Tetanospasmin inhibits compounds needed to inhibit muscle contraction Clostridium tetani Symptoms of tetanus include: Trismus (lockjaw) involves spasms of the jaw muscle and clenching of the teeth Opisthotonus involves muscle spasms that cause an arching of the back Spasmodic inhalation and seizures in the diaphragm and rib cage reduces ventilation Sedatives, muscle relaxants, and penicillin are used in treatment Tetanus toxoid is used in vaccination Listeria monocytogenes non-spore-forming gram-positive coccobacilli 1-4 flagella no capsules resistant to cold, heat, salt, pH extremes & bile primary reservoir is soil & water can contaminate foods & grow during refrigeration Listeria monocytogenes Listerosis immunocompromised patients, fetuses & neonates affects brain & meninges 20% death rate ampicillin & trimethoprimsulfamethoxazole Prevention pasteurization & cooking Mycoplasmas M. pneumoniae primary atypical pneumonia Walking pneumonia pathogen slowly spreads over interior respiratory surfaces causes fever, chest pain and sore throat Corynbacterium diptheriae gram-positive irregular bacilli 2 stages of disease: 1. Local infection –upper respiratory tract inflammation – sore throat, nausea, vomiting, swollen lymph nodes, pseudomembrane formation can cause asphyxiation 2. Diptherotoxin production and toxemia target organs primarily heart and nerves Epidemiology and Pathology Reservoir of healthy carriers potential for diphtheria is always present Most cases occur in nonimmunized children living in crowded, unsanitary conditions Acquired via respiratory droplets from carriers or actively infected individuals Corynbacterium diptheriae Diagnostic methods Pseudomembrane and swelling indicative Stains Conditions, history Serological assay Treatment: Antitoxin Penicillin or erythromycin Prevented by toxoid vaccine series and boosters Mycobacterium Genus gram-positive irregular bacilli acid-fast staining strict aerobes produce catalase possess mycolic acids & a unique type of peptidoglycan do not form capsules, flagella or spores grow slowly 2 medically important: Mycobacterium tuberculosis Mycobacterium leprae Mycobacterium tuberculosis contain complex waxes & cord factor prevent destruction by lysosomes of macrophages transmitted by airborne respiratory droplets only 5% infected people develop clinical disease Primary TB infectious dose 10 cells phagocytosed by alveolar macrophages multiply intracellularly after 3-4 weeks immune system attacks, forming tubercles granulomas consisting of a central core containing bacilli surrounded by WBCs Secondary TB reactivation of bacilli tubercles expand & drain into the bronchial tubes & upper respiratory tract gradually patient experiences more severe symptoms violent coughing, greenish or bloody sputum, fever, anorexia, weight loss, fatigue untreated 60% mortality rate Extrapulmonary TB during secondary TB, bacilli disseminate to regional lymph nodes, kidneys, long bones, genital tract, brain, meninges these complications are grave Diagnosis 1. in vivo or tuberculin testing 2. X rays 3. direct identification of acid-fast bacilli in specimen 4. cultural isolation and biochemical testing Treatment of TB 6-24 months of at least 2 drugs from a list of 11 one pill regimen called Rifater (isoniazid, rifampin, pyrazinamide) vaccine based on attenuated bacilli Calmet-Guerin strain of M. bovis used in other countries Mycobacterium leprae Hansen’s bacillus strict parasite slowest growing of all species multiplies within host cells in large packets called globi causes leprosy chronic disease that begins in the skin & mucous membranes & progresses into nerves Leprosy (Hansen’s Disease) spread through direct inoculation from leprotics 2 forms tuberculoid superficial infection without skin disfigurement damages nerves and causes loss of pain perception lepromatous deeply nodular infection causes severe disfigurement of the face & extremities Diagnosing Combination of symptomology, microscopic examination of lesions, and patient history Detection of acid-fast bacilli in skin lesions, nasal discharges, and tissue samples Treatment and Prevention Treatment by longterm combined therapy Prevention requires constant surveillance of high risk populations WHO sponsoring a trial vaccine Gram-negative Cocci and Bacilli Bacterial Meningitis meninges of brain and spinal cord cross the blood-brain barrier can be caused by several bacterial species Neisseria meningitides Streptococcus pneumoniae Haemophilus influenzae Neisseria Gram-negative diplococci none develop flagella or spores capsules on pathogens Strict parasites do not survive long outside of the host Residents of mucous membranes of warm-blooded animals Aerobic or microaerophilic Pathogenic species require enriched complex media and CO2 2 primary human pathogens Neisseria gonorrhoeae Neisseria meningitidis Neisseria meningitidis Virulence factors capsule, pili, IgA protease 12 strains serotypes A, B, C, cause most cases Disease begins when bacteria enter bloodstream, pass into cranial circulation, multiply in meninges very rapid onset endotoxin causes hemorrhage and shock can be fatal Treated with penicillin, chloramphenicol Vaccines exist for group A and C Neisseria gonorrhoeae Causes gonorrhea Virulence factors pili, other surface molecules, IgA protease Strictly a human infection In top 5 STDs Infectious dose 100-1,000 Does not survive more than 1-2 hours on fomites Infection is asymptomatic in 10% of males and 50% of females Gonorrhea Males urethritis, yellowish discharge, scarring & infertility Extragenital infections anal, pharygeal, conjunctivitis, septicemia, arthritis Gonorrhea Females vaginitis, urethritis, salpingitis (PID) mixed anaerobic abdominal infection common cause of sterility & ectopic tubal pregnancies Gonorrhea in Newborns Infected as they pass through birth canal Eye inflammation, blindness Prevented by prophylaxis after birth Diagnosis and Control Gram stain 20-30% of new cases are penicillinaseproducing PPNG or tetracycline resistant TRNG Recurrent infections can occur Reportable infectious disease Enterobacteriaceae Family Enterics gram-negative bacteria many members inhabit soil, water, & decaying matter cause diarrhea through enterotoxins divided into coliforms (lactose fermenters) and non-coliforms (non lactose fermenters) Antigens and virulence factors of typical enteric bacteria Testing of Enterics miniaturized, multichambered tube inoculating rod pulled through length of tube carries an inoculum to all chambers Coliform Organisms and Diseases: Escherichia coli most common aerobic & non-fastidious bacterium in gut @ 150 strains Most not infectious Escherichia coli enterotoxigenic E. coli causes severe diarrhea due to heat-labile heat-stable toxin stimulate secretion & fluid loss also has fimbrae toxin & enteroinvasive E. coli causes inflammatory disease of the large intestine enteropathogenic E. coli linked to wasting from infantile diarrhea Enterohemorrhagic E. coli Newest strain Can permanently damage kidney Escherichia coli pathogenic strains frequent agents of infantile diarrhea greatest cause of mortality among babies causes ~70% of traveler’s diarrhea causes 50-80% UTI indicator of fecal contamination in water Other Coliforms Serratia marcescens produces a red pigment causes pneumonia, burn & wound infections, septicemia & meningitis Klebsiella pneumoniae Citrobacter opportunistic UTIs & bacteremia Salmonella S. enteritidis 1,700 serotypes salmonellosis zoonotic gastroenteritis 2-5 days Typhoid Fever caused by Salmonella enterica serotype Typhi (S. typhi) typhoid fever ingested bacilli adhere to small intestine cause invasive diarrhea that leads to septicemia S. Typhi is transmitted by the five Fs: Flies Food Fingers Feces Fomites Shigella shigellosis incapacitating dysentery S. dysenteriae, S. sonnei, S. flexneri & S. boydii produce H2S or urease Nonmotile nonencapsulated Shigella invades villus of large intestine can perforate intestine or invade blood enters Peyer’s patches & instigates inflammatory response endotoxin & exotoxins treatment fluid replacement & ciprofloxacin & sulfa-trimethoprim Yersinia pestis tiny, gram-negative rod unusual bipolar staining & capsules virulence factors capsular & envelope proteins protect against phagocytosis & foster intracellular growth coagulase Yersinia pestis sylvatic plague humans develop plague through contact with wild animals urban plague domestic or semidomestic animals or infected humans found in 200 species of mammals rodents harbor the organism but do not develop the disease flea vectors bacteria replicates in gut, coagulase causes blood clotting that blocks the esophagus flea becomes ravenous Pathology of Plague bubonic bacillus multiplies in flea bite, enters lymph, causes necrosis & swelling in groin or axilla bubo septicemic progression to massive bacterial growth virulence factors cause intravascular coagulation subcutaneous hemorrhage & purpura black plague pneumonic infection localized to lungs, highly contagious fatal without treatment Plague Treatment streptomycin, tetracycline or chloramphenicol Killed or attenuated vaccine http://www.youtube.com/watch?v=9IjhQDnoCcY Bordetella pertussis aerobic coccobacillus causes pertussis or whooping cough communicable childhood affliction acute respiratory syndrome often severe, life-threatening complications in babies reservoir apparently healthy carriers transmission by direct contact or inhalation of aerosols Bordetella pertussis virulence factors receptors that recognize & bind to ciliated respiratory epithelial cells toxins that destroy & dislodge ciliated cells DTaP vaccine acellular vaccine contains toxoid & other Ags Pseudomonas small gram-negative bacilli single polar flagellum highly versatile metabolism Pseudomonas aeruginosa intestinal resident in 10% normal people resistant to soaps, dyes, quaternary ammonium disinfectants, drugs, drying Use aerobic respiration do not ferment carbohydrates Opportunistic Pseudomonas aeruginosa common cause of nosocomial infections in hosts with burns, neoplastic disease, cystic fibrosis complications include pneumonia, UTI, abscesses, otitis, & corneal disease grapelike odor greenish-blue pigment (pyocyanin) multidrug resistant Francisella tularensis causes tularemia zoonotic disease of mammals (particularly rabbits) endemic to the northern hemisphere Aerobic bacilli transmitted by contact with infected animals, water & dust or bites by vectors headache, backache, fever, chills, malaise & weakness intracellular persistence can lead to relapse 30% death rate in systemic & pulmonic forms gentamicin or tetracycline “Atypical” Pneumonia Can Be Caused by a Diverse Group of Bacterial Species Mycoplasma pneumoniae Legionella pneumophila Coxiella burnetii Chlamydia pneumoniae Chlamydia psittaci Legionella pneumophila “Legionellosis”, Legionaires disease Motile aerobic bacilli widely distributed in water live in close association with amebas prevalent in males over 50 nosocomial disease in elderly patients fever, cough, diarrhea, abdominal pain, pneumonia fatality rate of 3-30% azithromycin Rickettsias, Chlamydias, Spirochetes and Vibrios Rickettsia obligate intracellular parasites gram-negative cell wall among the smallest bacteria nonmotile pleomorphic rods or coccobacilli ticks, fleas & louse are involved in their life cycle bacteria enter endothelial cells & cause necrosis of the vascular lining treat with tetracycline & chloramphenicol 4 Types of Rickettsioses Rocky Mountain spotted fever R. rickettsii zoonosis carried by dog ticks & wood ticks most cases on eastern seaboard distinct spotted rash Chlamydias obligate intracellular parasites small gram-negative cell wall alternate between 2 stages elementary body small metabolically inactive, extracellular, infectious form reticulate body grows within host cell vacuoles Chlamydia trachomatis 1. trachoma attacks the mucous membranes of the eyes, genitourinary tract & lungs ocular trachoma • severe infection, deforms eyelid & cornea, may cause blindness inclusion conjunctivitis • occurs as babies pass through birth canal • prevented by prophylaxis 2. STD urethritis, cervicitis, scarring lymphogranuloma venereum disfiguring disease of the external genitalia & pelvic lymphatics Spreading to the fallopian tubes can cause salpingitis Left untreated can cause pelvic inflammatory disease (PID) Increases the danger of infertility or ectopic pregnancies Chlamydia can also occur in the pharynx or anus Males complain of painful urination and watery discharge cause infertility in males Spirochettes Treponema Borrelia Treponema Gram-negative spirochetes live in the oral cavity, intestinal tract, & perigenital regions of humans & animals pathogens are strict parasites Treponema pallidum human is the natural host extremely fastidious & sensitive cannot survive long outside of the host causes syphilis ID = 50 cells Pathogenesis and Host Response Spirochete binds to epithelium, multiplies, and penetrates capillaries. Moves into circulation and multiplies Untreated marked by stages Primary Secondary Tertiary Spirochete appears in lesions and blood during first 2 stages communicable Stages of Syphilis Primary syphilis appearance of hard chancre at site of inoculation chancre heals spontaneously Secondary syphilis fever, headache, sore throat, red or brown rash on skin, palms and soles rash disappears spontaneously Stages of Syphilis Tertiary syphilis about 30% of infections enter in tertiary stage can last for 20 years or longer neural, cardiovascular symptoms, gummas develop Congenital syphilis nasal discharge, skin eruptions, bone deformation, nervous system abnormalities Borrelia Borrelioses Gram-negative spirochetes transmitted by arthropod vector B. hermsii relapsing fever B. burgdorferi Lyme disease B. hermsii - Relapsing Fever mammalian reservoirs squirrels, chipmunks, wild rodents tick-borne after 2-15-day incubation, patients have high fever, shaking, chills, headache, & fatigue Nausea, vomiting, muscle aches, abdominal pain extensive damage to liver, spleen, heart, kidneys, & cranial nerves parasite changes & immune system tries to control it recurrent relapses tetracycline B. burgdorferi - Lyme Disease transmitted by ticks complex 2-year cycle involving mice & deer nonfatal, slowly progressive syndrome that mimics neuromuscular & rheumatoid conditions B. burgdorferi - Lyme Disease Symptoms: 70% get bull’s eye rash fever, headache, stiff neck, & dizziness if untreated can progress to cardiac & neurological symptoms, polyarthritis tetracycline, amoxicillin vaccine for dogs, human vaccine discontinued insect repellant containing DEET Vibrio cholera Cholera Curviform gramnegative top 7 causes of morbidity & mortality ingested with food or water infectious dose 108 Vibrio cholera infects surface of small intestine, noninvasive cholera toxin causes electrolyte & water loss through: secretory diarrhea, resulting dehydration leads to muscle, circulatory, & neurological symptoms Treatment oral rehydration, tetracycline vaccine Campylobacter jejuni important cause of bacterial gastroenteritis transmitted by beverages & food Curviform gram-negative reach mucosa at the last segment of small intestine near colon adhere, burrow through mucus and multiply symptoms of headache, fever, abdominal pain, bloody or watery diarrhea Helicobacter pylori Curviform gram-negative discovered in 1979 in stomach biopsied specimens causes 90% of stomach & duodenal ulcers people with type O blood have a 1.5-2X higher rate of ulcers Same receptor in common produces large amounts of urease © P. Hawtin/Photo Researchers, Inc. The bacteria produce urease, which in turn produces ammonia neutralizes acid in that area of the stomach allows the bacteria to survive The ammonia, and an H. pylori cytotoxin destroy mucoussecreting cells creates a sore