Hepatitis - Austin Community College
advertisement

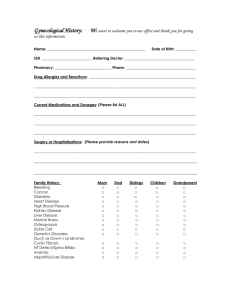
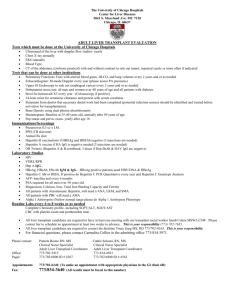
Liver Disorders John Nation, RN, MSN Fall 2011 From the notes of Charlene Morris, RN, MSN Austin Community College Overview of Today’s Lecture A & P Review Hepatitis A Hepatitis B Hepatitis C Cirrhosis Portal Hypertension Esophageal Varices Hepatic Encephalopathy Hepatorenal Syndrome Liver Transplant A and P Review A and P Review Largest internal organweighs around 3 lbs! A B C D E Liver Hepatic vein Hepatic artery Portal vein Common bile duct F Stomach G Cystic duct H Gallbladder Blood Supply – 2 sources Hepatic artery: – 500ml/min of oxygenated blood. – 30% of Cardiac output goes to the liver Portal vein – 1000ml/min – partly oxygenated blood supplies 50 - 60% O2 plus rich supply of nutrients, toxins, drugs – from stomach, small and large intestines, pancreas and spleen Hepatic Blood Supply (Cont’d) Both empty into capillaries/sinusoids Liver filters the blood Hepatic vein to inferior vena cava Lobule – Functional unit of the liver Capillaries Metabolic Functions of the liver “Body’s Refinery” Over 400 functions Primary role in anabolism and catabolism Metabolic Functions of the Liver 1. Metabolism of Glucose 2. Protein Storage 3. Fatty acids 4. Cholesterol Other functions Immunologic Blood storage Plasma protein synthesis Clotting Waste products of hemoglobin Formation and secretion of bile Steroids and hormones Ammonia Drugs, alcohol and toxins metabolism To Summarize…. The liver: – changes food into energy – removes alcohol and poisons from the blood – makes bile, a yellowish-green liquid that helps with digestion Hepatitis Simply means inflammation of the liver – “itis” means inflammation, “hepa” means liver. Viral hepatitis – Most common cause – Viral types include A, B, C, D, E, and G Hepatitis Other possible causes – Drugs (alcohol) – Chemicals – Autoimmune liver disease – Bacteria (rarely) Hepatitis Etiology Causes – A, B, C, D, E, and G virus – Cytomegalovirus – Epstein-Barr virus – Herpes virus – Coxsackie virus – Rubella virus Hepatitis A Hepatitis A virus (HAV) – RNA virus – Transmitted fecal–oral route, parenteral (rarely) – Frequently occurs in small outbreaks Hepatitis A 61,000 cases of hepatitis A occur annually in the United States 10 million cases of hepatitis A occur worldwide – Nearly universal during childhood in developing countries Hepatitis A Hepatitis A virus (HAV) – Found in feces 2 or more weeks before the onset of symptoms and up to 1 week after the onset of jaundice – Present in blood briefly – No chronic carrier state Hepatitis A: Incubation Period 2-6 weeks Acute onset Mild flu-like manifestations Symptoms last up to 2 months Liver usually repairs itself, so no permanent effects Hepatitis A Hepatitis A virus (HAV) – Anti-HAV immunoglobulin M (IgM) Appears in the serum as the stool becomes negative for the virus Detection of IgM anti-HAV indicates acute hepatitis Hepatitis A Hepatitis A virus (HAV) – Anti-HAV immunoglobulin G (IgG) IgG anti-HAV: Indicator of past infection Presence of IgG antibody provides lifelong immunity Hepatitis A: Mode of Transmission Mainly by ingestion of food or liquid infected with the virus –Poor hygiene, improper handling of food, crowding housing, poor sanitation conditions are all factors related to Hepatitis A Hepatitis A: Mode of Transmission (Cont’d) Occurs more frequently in underdeveloped countries Contaminated waters –Drinking water, contaminated seafood Food-borne Hepatitis A outbreaks usually due to infected food handler –Contamination of food during preparation Hepatitis A: Vaccine 2 doses IM –Initial dose –Booster in 6 to 12 months Post-exposure Prophylaxis Standard IG-immune globulin – Given IM within 2 weeks of exposure Hepatitis A Vaccine IG is recommended for persons who do not have anti-HAV antibodies and have had food borne exposure or close contact with HAV-infected person Remember 2/2/2/2 Rule 2 doses IM for vaccination Signs & symptoms last 2 months Contagious 2 weeks before signs & symptoms Post-exposure dose given IM within 2 weeks of exposure Must report within one day Hepatitis B Nearly 400 million people infected with Hepatitis B – 50% to 75% active viral replication 73,000 new cases of Hepatitis B annually in United States – Incidence decreased due to HBV vaccine Hepatitis B Hepatitis B virus (HBV) – DNA virus – Transmission of HBV Perinatally by mothers infected Percutaneously (IV drug use) Mucosal exposure to infectious blood, blood products, or other body fluids Hepatitis B Hepatitis B virus (HBV) –Transmission occurs when infected blood or other body fluids enter the body of a person who is not immune to the virus Hepatitis B Hepatitis B virus (HBV) – Sexually transmitted disease – Can live on a dry surface for 7 days – More infectious than HIV Hepatitis B- Precautions Source: Uptodate PREVENT INFECTION OF FAMILY — Acute and chronic hepatitis B are contagious. Thus, people with hepatitis B should discuss measures to reduce the risk of infecting close contacts. This includes the following: Discuss the infection with any sexual partners and use a latex condom with every sexual encounter. Do not share razors, toothbrushes, or anything that has blood on it. Cover open sores and cuts with a bandage. Do not donate blood, body organs, other tissues, or sperm. Hepatitis B- Precautions Source: Uptodate Immediate family and household members should have testing for hepatitis B. Anyone who is at risk of hepatitis B infection should be vaccinated, if not done previously. (See "Patient information: Adult immunizations".) Do not share any injection drug equipment (needles, syringes). Clean blood spills with a mixture of 1 part household bleach to 9 parts water. Hepatitis B- Prevention Hepatitis B cannot be spread by: Hugging or kissing* (some disagreement) Sharing eating utensils or cups Sneezing or coughing Breastfeeding Source: Uptodate Hep B Incubation Period 6-24 weeks Prevention –Vaccine-3 doses Initial dose Dose at 4 weeks Dose 5 months later Post-exposure Hep B Hepatitis B Immune globulin IM in 2 doses – First dose within 24 hours to 7 days of exposure – Second dose 20 to 30 days post-exposure Provides short-term immunity Give HBV vaccine concurrently- vaccine can be beneficial post- exposure Hepatitis B Hepatitis B virus (HBV) – Complex structure with three antigens Surface antigen (HBsAg) Core antigen (HBcAg) E antigen (HBeAg) – Each antigen—a corresponding antibody may develop in response to acute viral Hepatitis B Hepatitis B Virus Presence of Hepatitis B Surface Antibodies – Indicates immunity from HBV vaccine – Past HBV infection – With chronic infection, liver enzyme values may be normal or ↑ – 15% to 25% of chronically infected persons die from chronic liver disease Hepatitis C Approximately 170 million people are infected with the hepatitis C virus (HCV) Estimated 30,000 new cases diagnosed annually Hepatitis C 8000 to 10,000 people in the United States die each year from complications of end-stage liver disease secondary to HCV Approximately 30% to 40% of HIV-infected patients also have HCV Hepatitis C Hepatitis C virus (HCV) – Transmitted primarily percutaneously – Risk factors IV drug use –Most common mode of transmission in United States and Canada Blood transfusions Hepatitis C Hepatitis C virus (HCV) –Risk factors (cont’d) – High-risk sexual behavior Hemodialysis Occupational exposure Perinatal transmission Hepatitis C: Transmission Hepatitis C virus (HCV) – Up to 10% of patients with HCV cannot identify a source – Risk of body piercings, tattooing, and intranasal drug use in transmission of HCV Hepatitis C Diagnostic Studies Anti-HCV HCV RNA antibody Hepatitis C Interventions Harm Reduction - Austin Harm Reduction Coalition Hepatitis D Hepatitis D virus (HDV) – Also called delta virus – Defective single-stranded RNA virus – Cannot survive on its own – Requires the helper function of HBV to replicate Hepatitis D Hepatitis D virus (HDV) (cont’d) –HBV-HDV co-infection ↑ Risk of fulminant hepatitis More severe acute disease Hepatitis E Hepatitis E virus (HEV) – RNA virus – Transmitted fecal–oral route – Most common mode of transmission is drinking contaminated water – Occurs primarily in developing countries Hepatitis G Hepatitis G virus (HGV) –RNA virus –Poorly characterized parenterally and sexually transmitted virus –Found in some blood donors –Can be transmitted by blood transfusion Hepatitis G Hepatitis (cont’d) G virus (HGV) –Coexists with other hepatitis viruses and HIV –Does not appear to cause liver damage Pathophysiology of Hepatitis Acute infection- widespread inflammation of liver tissue – Liver damage mediated by Cytotoxic cytokines Natural killer cells – Liver cell damage results in hepatic cell necrosis Common Manifestations of Acute Hepatitis Predictable course among all the viruses Incubation Phase: after exposure to virus, no symptoms Preicteric Phase of Hepatitis Flu-like symptoms –General malaise –Fatigue –Body aches, headache –GI symptoms- nausea/vomiting, diarrhea, abdominal discomfort –Chills, low grade fever Icteric or Jaundice Phase Usually 5-10 days after pre-icteric symptoms Jaundice results when bilirubin diffuses into tissues Sclera jaundiced Urine darkens due to excess bilirubin being excreted If bilirubin cannot flow out of liver, stool will be light or clay-colored Severe Jaundice Hepatitis Clinical Manifestations Pruritus can accompany jaundice – Accumulation of bile salts beneath the skin When jaundice occurs, fever subsides Liver usually enlarged and tender Convalescent Phase Healing generally within 3-16 weeks Begins as jaundice is disappearing GI symptoms minimal Hepatitis Liver cells can regenerate with time and if no complications occur, resume their normal appearance and function Hepatitis Complications Fulminant Hepatic Failure Chronic Hepatitis Cirrhosis Hepatocellular Carcinoma Fulminant Hepatitis Results in severe impairment or necrosis of liver cells and potential liver failure Develops in small percentage of patients Occurs because of Complications of Hepatitis B Toxic reactions to drugs and congenital metabolic disorders Diagnostic tests Liver function studies – ALT (Alanine aminotransferase) – elevates: enzyme in liver cells released into bloodstream with injury or disease (0 – 50) normal – AST (Aspartate aminotransferase) – elevates: enzyme in liver & heart cells released into bloodstream (0 -41) – GGT – gamma glutamyltransferase: present in all cell membranes, inj or disease = elevates in cell lysis, (8 – 55). increases when bile ducts are blocked & hepatitis. Elevated until function returns. Diagnostic tests – Alkaline phosphatase – present in liver & bone cells. Elevated in hepatitis.(44-147 IU/L) – CBC – low RBC, Hct, Hgb related to anemia, RBC destruction, bleeding, folic acid and vitamin deficiencies. – Low WBC and Platelets Increased blood flow to spleen – cells destroyed faster than needed – AFP- alpha fetoprotein– liver cancer marker – Lactic dehydrogenase LDH5 specific for liver damage Diagnostic tests Coagulation – prolonged prothrombin time due to poor production of prothombin by liver and decreased Vitamin K absorption (Normal PT 12-15 seconds, INR 0.8 to 1.2) Hyponatremia –hemodilution Hypokalemia, hypophosphatemia, hypomagnesemia –malnutrition & renal loss Bilirubin – Total (2-14 umol/L) Bilurubin – direct/conjugated (0-4 umol/L) Diagnostic tests Serum albumin – low due to impaired liver production (3.3 – 5) Serum ammonia – high (0 – 150)(10 to 80 ug/l) Glucose and cholesterol –abnormal due to impaired liver function Abd. Ultrasound – liver size, ascites, or nodules Esophagascopy – look for varices Liver biopsy CT, MRI Rx Impacting Liver A host of medications can cause abnormal liver enzymes levels. Examples include: Pain relief medications such as aspirin, acetaminophen (Tylenol), ibuprofen (Advil, Motrin), naproxen (Narosyn), diclofenac (Voltaren), and phenylbutazone (Butazolidine) Anti-seizure medications such as phenytoin (Dilantin), valproic acid, carbamazepine (Tegretol), and phenobarbital Antibiotics such as the tetracyclines, sulfonamides, isoniazid (INH), sulfamethoxazole, trimethoprim, nitrofurantoin, etc. Rx Impacting Liver Cholesterol lowering drugs such as the "statins" (Mevacor, Pravachol, Lipitor, etc.) and niacin Cardiovascular drugs such as amiodarone (Cordarone), hydralazine, quinidine, etc. Anti-depressant drugs of the tricyclic type (ie elavil) With drug-induced liver enzyme abnormalities, the enzymes usually normalize weeks to months after stopping the medications. Liver Biopsy Needle biopsy Most common in past Laparoscopic biopsy: Used to remove tissue from specific parts of the liver. Liver Biopsy (Cont’d) Transvenous biopsy Catheter into a vein in the neck and guiding it to the liver. A biopsy needle is placed into the catheter and advanced into the liver. Used for patients with blood-clotting problems or excess fluid Liver Biopsy Adequacy of clotting- PT/ INR, Platelets (Vit. K?) Type and cross match for blood Usually hold aspirin, ibuprofen, and anticoagulants Chest x-ray Consent form & NPO 4 to 8 hr. Liver Biopsy (Cont’d) Consent form & NPO 4 to 8 hr. Vital signs & Empty bladder Supine position, R arm above head Hold breath after expiration when needle inserted Be very still during procedure – 20 minutes Liver Biopsy Video Complications are: Puncture of lung or gallbladder, infection, bleeding, and pain. After Needle Liver Biopsy Pressure to site, place pt on Rt side to maintain site pressure minimum of 2 hrs. & flat 12-14 hrs. Vital signs & check for bleeding NPO X 2H after Assess for peritonitis, shock, & pneumothorax Rt. shoulder pain common – caused by irritation of the diaphragm muscle – usually radiates to the shoulder for a few hours or days. After Needle Biopsy (Cont’d) Soreness at the incision site Avoid aspirin or ibuprofen for pain control for the first week because they decrease blood clotting, which is crucial for healing. CONSULT HEALTHCARE PROVIDER! Avoid coughing, straining, lifting x 1-2 weeks Hepatitis Care Rest is a priority! Diet –High calorie & protein, Low fat – Vitamin supplement – B complex & K – Avoid alcohol & drugs detoxed in liver Life style changes Meds for Chronic Hepatitis Chronic HBV Pegylated a-interferon (Pegasys, PEG-Intron) Lamivudine (Epivir) Adefovir (Hepsera) Entecavir (Baraclude) Telbivudine (Tyzeka) Chronic HCV Pegylated a-interferon (Pegasys, PEG-Intron) Ribavirin (Rebetol, Copegus) Hepatitis Nursing Management Nursing assessment Past health history – Hemophilia – Exposure to infected persons – Ingestion of contaminated food or water – Past blood transfusion (before 1992) Hepatitis Nursing Management Nursing assessment Medications (use and misuse) – Acetaminophen – Phenytoin – Halothane – Methyldopa Hepatitis Nursing Management Nursing assessment IV drug and alcohol abuse Weight loss Dark urine Fatigue Right upper quadrant pain Pruritus Hepatitis Nursing Management Nursing assessment Low-grade fever Jaundice Abnormal laboratory values Hepatitis Nursing Management Nursing diagnoses Imbalanced nutrition: Less than body requirements Activity intolerance Ineffective therapeutic regimen management Hepatitis Nursing Management Overall goals: Planning –Relief of discomfort –Resumption of normal activities –Return to normal liver function without complications Hepatitis Nursing Management Nursing implementation Health promotion –Hepatitis A Education Vaccination Good hygiene practices Hepatitis Nursing Management Nursing implementation Health Promotion –Hepatitis B Vaccination Education Workplace safety Hepatitis Nursing Management Nursing implementation Health promotion –Hepatitis C Education Infection control precautions Modification of high-risk behavior Hepatitis Nursing Management Nursing implementation Acute intervention –Rest –Jaundice Assess degree of jaundice Small, frequent meals Hepatitis Nursing Management Nursing implementation Ambulatory and home care –Dietary teaching –Assessment for complications –Regular follow-up for at least 1 year after diagnosis Hepatitis Nursing Management Nursing implementation Ambulatory and home care –Avoid alcohol Hepatitis Nursing Management Evaluation Expected outcomes –Adequate nutritional intake –Increased tolerance for activity –Verbalization of understanding of follow-up care Hepatitis Nursing Management Evaluation Expected outcomes –Able to explain methods of transmission and methods of preventing transmission to others Hepatitis Reporting Break! Cirrhosis Cirrhosis Pathophysiology Cirrhosis is the end stage of chronic liver disease Progressive, leads to liver failure Insidious, prolonged course Ninth leading cause of death in United States Twice as common in men Cirrhosis Pathophysiology Hepatocytes are destroyed and portal hypertension develops Liver cells attempt to regenerate Regenerative process is disorganized Functional liver tissue is destroyed and scarring of liver occurs New fibrous connective tissue distorts liver’s normal structure, with impeded blood flow Four Types of Cirrhosis Alcoholic Cirrhosis – formerly called Laennec’s Post necrotic Cirrhosis Biliary/obstructive - bile flow obstructed causing damage to liver Cardiac- from right side heart failure Alcoholic or Nutritional Cirrhosis (formerly called Laennec’s) Usually associated with alcohol abuse Most common cause of cirrhosis Causes metabolic changes in liver; fat accumulates in liver (fatty liver) Fatty liver potentially reversible if alcohol consumption ceases Post Necrotic Cirrhosis Results from complication of viral infections, Hepatitis, or exposure to toxins Liver shrinks because lobules destroyed, broad bands of scar tissue form within the liver Biliary Cirrhosis Associated with chronic biliary obstruction and infection Retained bile damages and destroys liver cells, causing fibrosis of liver Cardiac Cirrhosis Results from long-standing severe right sided heart failure Elevated central venous pressures cause stasis of blood in veins of liver, which leads to fibrosis Early Signs of Cirrhosis Complications and Common Manifestations 1. Hepatomegaly and RUQ pain 2. Weight loss 3. Weakness 4. Anorexia 5. Diarrhea and constipation Cirrhosis Interventions- Drugs Diuretics– Aldactone (spironolactone): decreases aldosterone levels, K+ sparing – Lasix (furosemide) Salt-poor albumin Neomycin – decrease ammonia forming organisms. Typically only recommended when unable to tolerate lactulose Lactulose – decreases ammonia forming organisms and inc. acidity of bowel. Goal is 2-3 loose stools per day. Ferrous sulfate and folic acid – to treat anemia/ vitamin deficiency Cirrhosis InterventionsDrugs (Cont’d) Beta blocker: propranolol (Inderal), nadolol- to prevent bleeding of E varices in conjunction with isosorbide mononitrate (Imdur) lowers hepatic venous pressure Proton Pump Inhibitors, H2 Receptor Blockers– decrease irritation of varices Serax (oxazepam) – benzodiazepine for alcohol withdrawal, sedation, sleep. Is metabolized in the liver – use cautiously. Nursing Diagnoses Cirrhosis Fluid Volume deficit Ineffective protection: bleeding Disturbed thought process Ineffective breathing pattern Impaired skin integrity Imbalanced nutrition: less than body requirements Cirrhosis Interventions- Diet and fluids Low protein (sometimes), high carbohydrate, high calorie-if signs of acute hepatic encephalopathy With cirrhosis and no hepatic encephalopathy, high carbohydrate, high protein, low salt Low sodium-500 mg-2gms At first sign of encephalopathy or ammonia level increasing- decrease protein intake (sometimes) Early stage for liver regeneration- need high protein-(75-100gms) Later Manifestations of Cirrhosis Jaundice Jaundice occurs as a result of the decreased ability to conjugate and excrete bilirubin In the late stages of cirrhosis, patient is usually jaundiced JAUNDICE Hepatocellular Obstructive Hemolytic CirrhosisHepatocellular or intrahepatic jaundice Diseased liver cells can’t clear normal amounts of bilirubin from the blood. Obstructive or Extrahepatic Jaundice Due to the interference with the flow of bile in the hepatic duct. Liver is conjugating bilirubin but it cannot reach small intestines so is released into blood stream Hemolytic Jaundice Due to excessive destruction of RBC’s. – transfusion reaction – Faulty hemoglobin – sickle cell – Autoimmune destruction of RBC’s Major Complications of Cirrhosis Portal hypertension Variceal bleeding Ascites Spontaneous bacterial peritonitis Hepatorenal syndrome Hepatic encephalopathy Break! Portal Hypertension • The portal vein carries about 1500 ml/min of blood from the small and large bowel, spleen, and stomach to the liver. • Any obstruction or increased resistance to flow or, rarely, pathological increases in portal blood flow may lead to portal hypertension with portal pressures over 12 mm Hg. • alcoholic and viral cirrhosis are the leading causes of portal hypertension in Western countries. Portal Hypertention (Cont’d) – Increases in portal pressure cause development of a portosystemic collateral circulation with resultant compensatory portosystemic shunting and disturbed intrahepatic circulation. – These factors are partly responsible for the important complications of chronic liver disease, including variceal bleeding, hepatic encephalopathy, ascites, hepatorenal syndrome, recurrent infection, and abnormalities in coagulation. – Variceal bleeding is the most serious complication and is an important cause of death in patients with cirrhotic liver disease. PORTAL HYPERTENSION normal 3 mmHg 12 mmHg = esophageal rupture Resistance to blood flow = Increase in pressure in portal venous system. – Swelling, inflammation, fibrosis, scarring of liver – Thrombus – Resistance in Inferior vena cava: Rt.CHF, myopathy Blood takes collateral channels - esophagus, stomach, spleen etc, veins, hemorrhoids May need shunts or TIPS Transjugular Intrahepatic Portosystemic Shunt to decrease pressure, beta blockers also help Portal Hypertension Esophageal Varices Arteriovenous shunting Hypersplenism Caput medusae Moderate anemia (dilated abd. veins) Thrombocytopenia Hemorrhoids Neutropenia Marked ascites Ascites &Caput medusae Spider angiomas Treatment of esophageal varices Active bleeding Central line & pulmonary artery pressures Blood transfusions & fresh frozen plasma for clotting factors Somatostatin or Vasopressin – constrict gut vessels Nitroglycerin- to counter negative affects of vasopressin Airway/trach Later prevention of re-bleeding Beta-blockers Long-acting nitrates Soft food, chew well, avoid intra-abdominal pressure Protonix (pantoprazole) Rapid Endoscopy! Sclerotherapy: • A sclerosant solution (ethanolamine oleate or sodium tetradecyl sulphate) is injected into the bleeding varix or the overlying submucosa • Complications can include fever, dysphagia and chest pain, ulceration, stricture, and (rarely) perforation. Band ligation: • Band ligation is achieved by a banding device attached to the tip of the endoscope Band Ligation Balloon Tube Tamponade: • The balloon tube tamponade may be life saving in patients with active variceal bleeding if emergency sclerotherapy or banding is unavailable • The main complications are gastric and esophageal ulceration, aspiration pneumonia, and esophageal perforation. Minnesota TubeFour lumens: • one for gastric aspiration • two to inflate the gastric and esophageal balloons • one above the esophageal balloon for suction of secretions to prevent aspiration Sengstaken-Blakemore Tube Three Lumens: Esophageal balloon inflation Gastric balloon inflation Gastric aspiration Long term Management of Esophageal Varices Repeated endoscopic treatment Repeated endoscopic treatment eradicates esophageal varices in most patients, recurrent variceal bleeding is uncommon. Because portal hypertension persists, patients at risk for recurrent varices Long term drug treatment The use of beta-blockers after variceal bleeding has been shown to reduce portal blood pressures and lower the risk of further variceal bleeding. Prophylactic management Most patients with portal hypertension never bleed, and it is difficult to predict who will. Beta blockers have been shown to reduce the risk of bleeding. Transjugular Intrahepatic Portosystemic Shunt Special procedures – fistula created with portal vein and hepatic vein and then stents placed to keep it open. Bypasses the liver by returning blood to hepatic vein to inferior vena cava TIPS Transjugular intrahepatic portosystemic shunt TIPS POST TIPS: • Shunted blood contains high ammonia • Can lead to: hepatic encephalopathy Splenomegaly due to Portal hypertension The spleen enlarges as blood is shunted to splenic vein This increases rate of destruction of RBCs, WBCs, and platelets Decreases storage capacity of spleen Causes anemia, leukopenia and thrombocytopenia Ascites – Complication of Cirrhosis Blood flow diverted to mesenteric vessels – Increased capillary pressure leads to fluid leaving vessels out into peritoneal cavity High pressure in liver causes fluid to leave liver into peritoneal cavity This fluid is plasma filtrate with high concentration of albumin Minerals- Ca++ is attached to albumin decreases so phosphorus increases. K+ is low due to aldosterone Four Factors Lead to Ascites Hypoproteinemia Increased Na+ & Increased capillary permeability H2O retention Portal Hypertension Responses to third spacing Loss of albumin to ascites leads to hypoproteinemia, depletion of plasma proteins Loss of blood volume = lowered BP Reflexes aimed at returning blood pressure to normal include release of aldosterone – Increases reabsorption of NA+ back into blood and H2O follows, thus increasing blood volume ASCITES accumulation of high protein fluid in the abdomen - 3rd spacing Nursing Management ASCITES Assess for Respiratory Distress- Fowler’s position helps ease work of breathing in ascites Measure Abdominal Girth Accurate I&O MEDICAL TREATMENT Na+ restriction500 mg –2 gms Fluids-1500 ml/day Diuretics-Aldactone Albumin - NaCl poor Paracentesis To treat respiratory distress Pt will loose 10-30 grams of protein Pt in sitting position Empty bladder first Post--watch for hypotension, bleeding, shock & infection Additional Complications Liver Failure Liver Failure Complex syndrome characterized by impairment of many organs and body functions Two conditions: Hepatic Encephalopathy Hepatorenal Syndrome Hepatic encephalopathy: Alteration in neuro status due to accumulation of ammonia Build-up of other substances such as hormones, GI toxins, drugs also contribute Where does ammonia come from? A by-product of protein metabolism Protein and amino acids are broken down by bacteria in GI tract, producing ammonia. Liver converts this to urea which is eliminated in the urine Precipitating Factors – all place demands on liver Bleeding esophageal varices Ingestion of narcotics or barbiturates, anesthetics Excessive protein intake Electrolyte imbalance Hemodynamic alterations Diuretics Severe infection Blood transfusions Stages of Hepatic Encephalopathy Hepatic Encephalopathy - Onset Phase Personality changes, disturbances of awareness, forgetfulness, irritability, & confusion Hepatic Encephalopathy - Second Phase Hyperreflexia Asterixis or flapping – Altered hand writing Violent, abusive behavior Hepatic Encephalopathy + Babinski hyperactive reflexes obtained with reflex hammer - Coma Babinski Video Medical Management Hepatic Encephalopathy Neomycin Lactulose Protein reduction Hepatorenal syndrome Complication of Hepatic Failure Hepatorenal syndrome Complication of Hepatic Failure kidneys may appear normal physically but functioning impaired. Usually sudden decrease Urine production, increase BUN & Creatinine, jaundice and signs of liver failure Poor prognosis- most die within 3 wks without transplant Think due to decreased perfusion &/or toxins from failure of liver Liver Dialysis Bridge to transplant Dialyze 6 hours at a time Donors: Live donor liver transplants are an excellent option. Liver regenerates to appropriate size for their individual bodies. Survival rates increase / shorter wait time The donor - a blood relative, spouse, or friend, will have extensive medical and psychological evaluations to ensure the lowest possible risk. Blood type and body size are critical factors in determining who is an appropriate donor. Potential donors evaluated for: – – – – liver disease, alcohol or drug abuse, cancer, or infection. hepatitis, AIDS, and other infections. matched according to blood type and body size. Age, race, and sex are not considered. Cadaver donor have to wait Liver Transplant Video Liver transplant complications Rejection. About 70% of all liver-transplant patients have some degree of organ rejection prior to discharge. Anti-rejection medications are given to ward off the immune attack. Infection Most infections can be treated successfully as they occur. Cancer Review 1. Pathophysiology 1. Cirrhosis 2. Portal hypertension 3. Liver failure 1. Encephalopathy 2. Hepato-renal syndrome 2. Signs & Symptoms 3. Treatment 4. Nsg. Care 5. Complications The End