General Anesthesia: Components, Induction, and Monitoring
advertisement

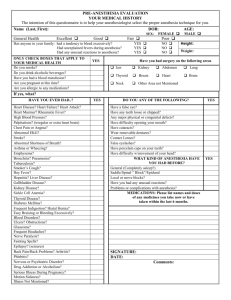
General anesthesia Outline of lecture Components and phases of general anesthesia Indications for GA Induction of GA Standard Rapid sequence induction Inhalation Monitors employed Basic components of general anesthesia Definition of Anesthesia: state of being unaware and unresponsive to painful stimuli Several aspects are involved a) lack of conscious awareness = unconsciousness b) lack of perception of pain = analgesia c) lack of movement = muscle relaxation d) modification of autonomic responses (HR,BP) to painful stimuli. Components of general anesthesia 2 Definition of Anesthesia: state of being unaware and unresponsive to painful stimuli a) lack of conscious awareness = unconsciousness Regional anesthesia (spinal, epidural, plexus block) is perhaps more correctly termed regional analgesia. Analgesia is an altered sensation of painful stimuli. The stimulus is felt as movement, pressure. Patient is usually partly aware of surroundings pregnant woman having C. Section under spinal analgesia Components of general anesthesia 3 Two aspects of conscious awareness: being awake and the formation of a memory of being awake. Goal of providing a level of sedation adequate to prevent patient being awake. Amount of required sedation depends on intensity of stimulation. If also give analgesia, one can prevent a patient being awake and in pain. If give relaxants and no analgesia, a patient can be awake and paralyzed and in pain. Awareness during GA Sedation with midazolam also causes amnesia (failure to form a memory of event even when awake) Volatile anesthesia at a depth greater than 0.7 MAC is thought to prevent awareness. Titration of level of anesthesia to a BIS level less than 60 is claimed to prevent awareness. Components of general anesthesia 4 Definition of Anesthesia: state of being unaware and unresponsive to painful stimuli b) lack of perception of pain = analgesia c) lack of movement in response to painful stimuli This will occur at MAC level of anesthesia or sub MAC levels and use of muscle relaxants d) modification of autonomic responses (HR,BP) to painful stimuli. This usually requires a dose of more than 1.0 MAC and is easier to achieve with specific drugs (beta blockers, potent narcotics) Components of general anesthesia 5 Practically impossible to create state of general anesthesia with a single drug A combination of various drugs of specific types is commonly used. Result of the combination satisfies all the desired categories and often has a synergistic effect. A sedative + narcotic is more potent than bigger dose of either alone Components of general anesthesia 6 Volatile agent e.g. sevoflurane has large amount of sedation, some muscle relaxation, but no analgesia. (Nitrous oxide has above features and analgesia) Propofol has sedation, some relaxation, some amnesia and no analgesia. Fentanyl has mild sedation, no relaxation, no amnesia and large amount of analgesia Muscle relaxants have no sedation, amnesia or analgesia 5 phases of general anesthesia (Preparation) Induction Maintenance Emergence Recovery Preparation for GA Patient assessment NPO status Airway Functional reserve of major organ systems CVS, respiratory, renal, hepatic Medications used regularly Allergies and previous experience with GA Type of planned procedure Urgency Position of patient during surgery Area of body involved Phases of general anesthesia Induction phase: transition from awake state to full affect of anesthesia on CNS, CVS, respiratory and muscle system Changes in CNS function are always accompanied by those of other systems Magnitude of changes in various systems reflect physiological state of patient age, stress level, physiological reserve, fluid balance, drug therapy Induction of anesthesia Drug effect on CNS is primarily depression of usual response There may be contrary effects related to loss of inhibitory actions of CNS (excitement) Examples: movements of limbs, hiccough, cough Induction of anesthesia Addition of supports is required to ensure adequate function of respiratory and CVS systems Airway control with oral airway, LMA, or ETT Ventilatory support Protection of the airway Blood pressure support with medication or IV fluids Further adjustment of anesthesia levels based on Patient response Stage of surgery Trends of monitored variables Maintenance of anesthesia Further adjustment of anesthesia levels based on Patient response Stage of surgery Trends of monitored variables Maintenance phase usually a stable period unless Changing level of surgical stress Impaired state of patient fitness Anesthesia gases form the major component with some IV narcotics or relaxants as background Emergence from anesthesia Slower version of induction phase in a reverse order CNS wakes up in stages or by regions Brainstem or lower functions first (breathing, cough, shivering) Cerebral cortex later (purposeful movements, response to commands) Removal of supports at appropriate time intervals Excitement aspects are common: limb movement, restlessness, coughing. Potential for vomiting, laryngospasm, upper airway obstruction Indications for general anesthesia Defined by surgical procedure Requires profound muscle relaxation Incision location above umbilicus Inability to provide comfort with local/regional anesthesia Duration of surgery more than 3 hours Defined by patient Airway protection Respiratory failure Unstable clinical state Inability to cooperate/ understand regional Complications of general anesthesia Respiratory failure Atelectasis Aspiration Hypotension Injury to peripheral nerves, cornea Injury to respiratory tract Intravenous induction Indications: Usual or default method of starting general anesthesia Risk of aspiration (see rapid sequence) Standard method involves drug combination: Sedative in large dose (propofol) usually with narcotic and/or anxiolytic (midazolam) Muscle relaxant if doing intubation Mask 100% O2 during process (before, during, after) Drug doses are initially based on weight and age of patient. Extra doses as directed by response of patient Intravenous induction Contraindications: Lack of proper equipment for resuscitation (IPPV, oxygen, airway devices, suction) Uncertainty about ability to ventilate or intubate patient if they become apneic Patient with partial airway obstruction (avoid apnea) Intravenous induction Precautions: Patient with limited or uncertain CVS reserve (hypovolemia, CHF, valvular stenosis, sepsis) Patients with poorly controlled CVS disease (high BP, angina, disturbed heart rhythm) Patients with risk of aspiration Patients with respiratory failure Intravenous induction Standard form vs slow form Standard form indicates use of standard doses given on basis of body weight. Slow form indicates careful titration of strong sedative drugs (propofol) or narcotics. Possible substitution with or addition of other medications (ketamine) Goal is the use of minimal but sufficient doses of anesthesia to reduce intensity of CVS and respiratory effects and allow time for compensation Rapid Sequence Induction Rapid sequence induction Indications: Patient at risk for regurgitation and aspiration who require GA History of recent vomiting or recent meal Pregnancy Increased intra-abdominal pressure Abdominal distension Poorly controlled GE reflux Decreased level of consciousness Rapid sequence induction Contraindications: Potential difficult intubation Potential airway obstruction Laryngeal injury Cervical spine injury Poorly controlled BP Rapid sequence induction Precautions: Potential for loss of airway control Potential for severe BP change (high or low) Potential for cardiac dysrhythmias, including arrest, in predisposed patient. Potential for marked increase in ICP Rapid sequence induction Method: Preoxygenation is critical; best method unclear. Suction and airway alternatives available Use adjuvant drugs to control BP, HR response: midazolam, narcotics, lidocaine, ketamine, etc Explain and rehearse use of cricoid pressure with the patient. Optimize position of upper airway. Dose of potent sedative (propofol) as per body weight or titrate depending on reserve of CVS Rapid sequence induction After patient is asleep, apply cricoid pressure and give relaxant in large dose. Two choices: no active ventilation, proceed with laryngoscopy as relaxant has peak effect Gentle IPPV (Paw 10-15 cm H2O) with 100% O2 until relaxant has peak effect. Place ETT, and inflate cuff and confirm correct position of ETT before removing cricoid pressure Inhalation induction Inhalation induction Indications: Difficult IV access Potential airway obstruction e.g. epiglottitis Thoracic diseases which preclude use of IPPV Mediastinal mass, foreign body in airway, broncho-pleural fistula Patients unable to cooperate with awake airway endoscopy Inhalation induction 2 Contraindications: Aspiration risk (unless overruled by airway concerns) Active bleeding in airway (risk of cough, laryngospasm) Note profound changes in BP are unusual with this as compared to rapid sequence with IV drugs No controlled studies in this area of “right way to do induction in this type of patient” Inhalation induction 3 Precautions: Lack of patient cooperation or comprehension Preexisting respiratory failure Patients may become restless before falling deeply asleep. This is a temporary phenomenon “excitement phase”. Use gentle assisted ventilation and wait. After several minutes of anesthesia, expect improved conditions for starting an IV, if not already done. Inhalation induction 4 Describe steps briefly to patient. Emphasis on deep breaths with maximal breath holding interval. Best agents are sevoflurane, enflurane, halothane. Desflurane and isoflurane are irritating to airway. Avoid narcotics; give sedation with midazolam. Coach patient with calm, reassuring voice Choices of technique: Several deep breaths from a primed circuit Slow incremental doses with normal ventilation Inhalation induction 5 Single / several deep breath technique: Prime circuit with anesthesia agent from vapourizer at maximum setting, FGF at 8L/min, pop off valve open and patient end of circuit occluded. Have patient exhale maximally, then apply face mask to patient and inhale maximally from primed circuit. Expect prompt onset of sleep (60 seconds) followed by transient apnea, then pattern of rapid shallow respirations. Inhalation induction 6 Slow incremental doses with normal ventilation Prime circuit with N2O 70%, FGF at 8L/min, pop off valve open and patient end of circuit occluded. When patient is comfortable with situation, begin volatile agent increasing vapourizer setting by 0.5% every 3 or 4 breaths. Reassure patient with calm voice encouraging a regular smooth breathing pattern. Use of a deep breathing pattern here may lead to premature onset of apnea with prolonged phase. Expect several minutes to fall asleep. Assist ventilation Inhalation induction 7 Time to safe airway insertion: Use eye signs and elapsed time, not ET concentration as guide. Consider response to oral airway as trial With single deep breath technique, authors suggest possible insertion of LMA after at least 2 minutes, ETT at least 5 minutes following onset of sleep. Laryngospasm, coughing, inadequate view of larynx is possible. Do not rush. Place patient on 50-100% O2 shortly before attempted insertion of LMA / ETT Monitors used during Induction of Anesthesia Monitors during induction of anesthesia Pulse oximetry and end tidal CO2 are critical Eyes and ears of the anesthesia person Experienced assistant is very important Stethescope, BP, EKG Prepare with plan B