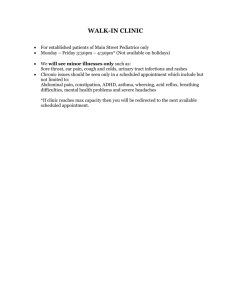
Figure 2: Adult Pulmonary new patient appointment lead time by
advertisement

University of Michigan Taubman Center Taubman Center Hours Expansion: Feasibility Analysis for Adult Pulmonary, Adult Nephrology, Adult General Otolaryngology Clinics Final Report To: Mrs. Katie Konson, Senior Project Manager, Ambulatory Care Services Dr. Connie Standiford, MD, Executive Medical Director Ambulatory Care Services Mr. Matt Bazzani, Chief Department Administrator of Family Medicine Mrs. Tammy Ellies, Project Senior Manager and Lean Coach Ms. Katie Schwalm, Engineering Fellow Dr. Mark Van Oyen, University of Michigan Professor From: IOE 481 Project Team 1 Mr. Nicholas Curry Ms. Sarah Gombert Mr. Daniel Varsanik Date: December 10, 2013 TABLE OF CONTENTS EXECUTIVE SUMMARY ...............................................................................................I INTRODUCTION ..........................................................................................................1 Background ..........................................................................................................1 Project Goal and Objectives ..................................................................................2 Project Scope ..........................................................................................................2 METHODS ......................................................................................................................2 Conducted Interviews .............................................................................................2 Performed Benchmarking .......................................................................................3 Analyzed MiChart Scheduling Data .......................................................................3 FINDINGS FROM DATA ...............................................................................................4 Interviews ................................................................................................................4 Benchmarking .........................................................................................................4 MiChart Scheduling Data .......................................................................................6 FEASIBILITY CHECKLIST ........................................................................................13 Checklist Methods ................................................................................................13 Checklist Findings ................................................................................................13 Checklist Conclusions ...........................................................................................13 CONCLUSIONS ........................................................................................................13 RECOMMENDATIONS ................................................................................................14 Feasibility Checklist ..............................................................................................14 Satellite Locations .................................................................................................14 In Clinic Expansion ...............................................................................................14 OPORTUNITES FURTHER ANALYSIS ....................................................................14 EXPECTED IMPACT ...................................................................................................15 REFERENCES ................................................................................................................16 Appendix A: Interview Questionnaire for Clinic Managers .........................................A-1 Appendix B: Interview Questionnaire for Urology Clinic Managers ............................B-1 Appendix C: Figures for Pulmonary Clinics .................................................................C-1 Appendix D: Patient Type and Provider Data Figures ..................................................D-1 Appendix E: Feasibility Checklist .................................................................................E-1 Appendix F: Partially Completed Checklist for Clinics ................................................F-1 LIST OF FIGURES Figure 1: Adult Pulmonary new patient appointment lead time........................................6 Figure 2: Adult Pulmonary new patient appointment lead time by month........................7 Figure 3: Adult Nephrology new patient appointment lead time.......................................7 Figure 4: Adult Nephrology new patient appointment lead time by month.......................8 Figure 5: Adult General Otolaryngology new patient appointment lead time...................8 Figure 6: Adult General Otolaryngology new patient appointment lead time by month.......................................................................................................................9 Figure 7: Adult Pulmonary correlation between lead time and cancellations ...................9 Figure 8: Adult Nephrology correlation between lead time and cancellations ................10 Figure 9: Adult General Otolaryngology number of new patient cancelations by lead time............................................................................................................10 Figure 10: Adult Pulmonary new patient monthly appointment volumes .......................11 Figure 11: Adult Nephrology new patient monthly appointment volumes......................12 Figure 12: Adult General Otolaryngology new patient monthly appointment volumes..................................................................................................................12 Figure C-1: TC Adult Pulmonary new patient appointment lead time...........................C-1 Figure C-2: TC Adult Pulmonary new patient appointment lead time by month .........C-1 Figure C-3: Briarwood Health Clinic Adult Pulmonary new patient appointment lead time...............................................................................................................C-2 Figure C-4: Briarwood Health Clinic Adult Pulmonary new patient appointment lead time by month...............................................................................................C-2 Figure C-5: Brighton Health Clinic Adult Pulmonary new patient appointment lead time...............................................................................................................C-3 Figure C-6: Brighton Health Clinic Adult Pulmonary new patient appointment lead time by month...............................................................................................C-3 Figure D-1: Adult Pulmonary percentage of new patients seen within 4-weeks by appointment type.................................................................................................D-1 Figure D-2: Adult Nephrology percentage of new patients seen within 4-weeks by appointment type.................................................................................................D-1 Figure D-3: Adult General Otolaryngology percentage of new patients seen within 4-weeks by provider............................................................................................D-2 Figure D-4: Adult Pulmonary percentage of new patients seen within 4-weeks by provider................................................................................................................D-3 Figure D-5: Adult Nephrology percentage of new patients seen within 4-weeks by provider................................................................................................................D-4 LIST OF TABLES Table 1: Hours of Operation Comparison ..........................................................................5 Table 2: Number of new patients that need to be seen to increase access to 80% ..........11 Table 3: Average number of new patients by appointment status ...................................12 ATTACHMENTS Adult Pulmonary Supplemental Information Adult Nephrology Supplemental Information Adult General Otolaryngology Supplemental Information EXECUTIVE SUMMARY The University of Michigan Hospital’s ambulatory care (outpatient) clinics want to explore the feasibility of extending business hours because new patients are not seen within the desired timeframe. To study the feasibility of extending hours, a student team from IOE 481 at the University of Michigan has investigated the relationship between extending hours and new patient access in three specific clinics: Adult Pulmonary, Adult Nephrology, and the Adult General Otolaryngology clinics within the Taubman Health Center (TC). The team was asked to provide a general feasibility checklist and partially completed checklists for the Adult Pulmonary, Adult Nephrology, and the Adult General Otolaryngology clinics. The team was also asked to provide analysis data pertaining to patient access for the Adult Nephrology, and the Adult General Otolaryngology clinics. One way the TC measures its performance is by patient access, which is determined by calculating the percentage of new patients have a completed appointment with a provider within 4 weeks of scheduling an appointment. The faculty group practice goal for the TC is for all areas to be operating at or greater than 80% new patient access. During a meeting, the Senior Project Manager stated that the clinics of Adult Pulmonary, Adult Nephrology and Adult General Otolaryngology have patient access rates below the faculty group practice goal of 80%. Data Methodology The following five sections describe the data collection and analysis. Conducted Interviews. The team interviewed three clinic managers from the Adult Pulmonary, Adult Nephrology, and Adult General Otolaryngology clinics. The team developed a questionnaire to gain understanding of how the clinics run and the requirements for a clinic to run. The team interviewed the three clinic managers a second time with a feasibility checklist draft to gain feedback on the current content. Performed Benchmarking with Urology. The Adult Urology clinic at TC launched extended hours in September 2013. The team used a questionnaire to interview the Adult Urology Operations Manager to gain information about the department’s extended hours program and research the development of the extended hours program. Performed Benchmarking with Competitors. The team benchmarked select University of Michigan Health System’s competitors through phone calls and Internet research to find the hours of operation at clinics similar to those at the TC. The main competitors benchmarked are: the Mayo Clinic, Cleveland Clinic, Beaumont Health System, St. Joseph Mercy Hospital, Johns Hopkins, and the Henry Ford Health System. Analyzed MiChart Scheduling Data. The team analyzed MiChart scheduling data from October 2012 to October 2013 for the Adult Pulmonary, Adult Nephrology, and Adult General Otolaryngology clinics in the TC. This data was used to calculate and analyze: New patient access New patient access by appointment types I New patient appointment status New patient cancellation reasons New patient appointment status by month New patient appointment slots per month Access of each new patient provider Correlations between cancellations and lead-time The number of new patients that need to be seen to increase patient access to 80% Data Findings The following sections describe the findings from the data collection and analysis. Interviews. The interviews with the 3 clinic managers of the Adult Pulmonary, Adult Nephrology, and Adult General Otolaryngology allowed the team discover that there are three main limitations in expanding hours: (1) specific ancillary services and testing, (2) provider type, and (3) patient preference for providers. The second set of interviews allowed the team to fill out the feasibility checklist for each of the three clinics. Benchmarking with Urology. The interview with the Adult Urology department allowed the team to understand the possible use of satellite locations for extended hours. Benchmarking Competitors. From benchmarking it was discovered that two of the University of Michigan Health System’s local competitors have extended hours via satellite locations. MiChart Scheduling Data. From the MiChart Scheduling data the team found that for the Adult Pulmonary, Adult Nephrology, and Adult General Otolaryngology clinics the access rates are 72%, 50%, and 23%, respectively. To reach an access of 80% based on the data, the Adult Pulmonary, Adult Nephrology, and Adult General Otolaryngology clinics need to see 6, 10, and 11 new patients, respectively, per week. Feasibility Checklist The team developed a feasibility checklist that will be used by future clinics when considering extending hours. The feasibility checklist has been developed through interviews conducted with the Adult Pulmonary, Adult Nephrology, and Adult General Otolaryngology clinic managers, as well as the benchmarking with the Adult Urology Operations manager. The team developed a categorization of five main topics to be considered: (1) Market – Business Need, (2) Needs Assessment, (3) Operational Planning, (4) Financial Evaluation, and (5) Implementation Planning. Conclusions Each clinic’s needs differ according to in-clinic procedures. Clinics also use different ancillary services according to patient and provider need. It was discovered that some satellite locations currently offer Saturday hours for patient appointments and urgent care clinics. These satellite clinics offer the possibility to increase patient access via Saturday hours as a feasible option. Through benchmarking, the team discovered that four out of six of the University of Michigan Health System’s competitors do not offer extended II hour services. The two competitors that do offer extended hours use satellite locations and are local competitors. The MiChart data showed that there is an access issue in the Adult Pulmonary, Adult Nephrology, and Adult Otolaryngology clinics operating at new patient access rates of 72%, 50%, and 29%, respectively. To reach an access of 80% based on the data, the Adult Pulmonary, Adult Nephrology, and Adult General Otolaryngology clinics need to see 6, 10, and 11 new patients, respectively, per week. Recommendations The following sections describe the recommendations for the feasibility checklist, satellite locations, and in clinic expansion. Feasibility Checklist. The team recommends that before considering expanded hours a clinic should complete the feasibility checklist based on specific clinic information. After filling out the checklist, the clinic should perform MiChart data analysis to find access rates and correlations. Next, a patient survey should be created in order to find when patients would want extended hours, if they would go to them, and where. The clinic should then do a clinic staff survey to find out if staff willingness to flex their schedules or change hours. Lastly, the clinic should research direct competitors to see if they have extended hours and if they hold the hours at satellite locations or at their main campus. Satellite Locations. A satellite location should only be used for extending hours on Saturdays. Some of the satellite locations within the University of Michigan Health System already offer Saturdays hours. In-Clinic Expansion. Before considering expanding hours the following should be optimized to capacity: Rooms Providers Scheduling Template Equipment If the clinic is currently operating at full capacity and is still considering expanding hours, the clinic should explore early or late expanded hours within the TC during the weekdays. Opportunities for Further Analysis To accurately compare the University of Michigan’s Health System’s competitors, the following subjects must be examined: Lead-time for competitors Access rates for competitors Number of patients seen daily Use of overbooking concepts Use of satellite locations III INTRODUCTION The University of Michigan Hospital’s ambulatory care (outpatient) clinics are exploring the feasibility of extending business hours because new patients are not seen within a desired timeframe. The goal of the University of Michigan Hospital is to have its outpatient clinics have 80% of new patients seen within 4 weeks of making an appointment; currently that goal is not being met. An IOE 481 student team from the University of Michigan evaluated the feasibility of extending hours and/or implementing weekend hours. To study the feasibility of extending hours, the team has investigated the relationship between extending hours and new patient access in three specific clinics: Adult Pulmonary, Adult Nephrology, and the Adult General Otolaryngology clinics within the Taubman Health Center (TC). The team was asked to create a feasibility checklist presenting ideas to consider before launching extended hours for further use of other TC clinics, as well as data pertaining to patient access for the Adult Nephrology, and the Adult General Otolaryngology clinics. This project is a groundbreaking investigation for higher patient access rates within all the TC clinics. This report discusses the data the team analyzed along with the conclusions and recommendations the team is providing. Background IOE 481 team investigated the Adult Pulmonary, Adult Nephrology, and Adult General Otolaryngology clinics. The Adult Pulmonary clinic provides care for patients with acute or chronic respiratory disease. The Adult Nephrology clinic provides care for patients with a wide range of kidney diseases. The Adult General Otolaryngology clinic provides care for patients with disorders of the ear, nose, and throat, which also include the head and neck. The Adult Pulmonary, Adult Nephrology, and Adult General Otolaryngology clinics operate from 8 am to 5 pm Monday through Friday and offer no weekend service in TC [1]. The clinics may need ancillary services such as radiology, phlebotomy, and possible other services during appointments. These services have their own separate hours that often differ from clinic hours [1]. Adult Pulmonary and Adult Nephrology share a total of 68 rooms with the following four other clinics in the TC: Gastroenterology, Infectious Diseases, General Medicine, and Rheumatology. These clinics require a certain number of providers and support staff, such as medical assistant, social workers, and nutritionists, to run the clinic. One way the TC measures its performance is by patient access, which is determined by calculating the percentage of new patients that meet with a provider within 4 weeks of making an appointment. The goal for the TC is for all units to be operating at or greater than 80% patient access. The clinics of Adult Pulmonary, Adult Nephrology and Adult General Otolaryngology have patient access rates below the faculty group practice goal of 80% [2]. Some patients who are not seen in a desired timeframe may cancel and/or possibly find care elsewhere. 1 Project Goal and Objectives The goal of this project was to explore the feasibility of extending clinic hours in the Adult Pulmonary, Adult Nephrology, and Adult General Otolaryngology clinics of the University of Michigan Hospital. To reach the goal, the following aspects have been analyzed and considered: Patient Access Clinic scheduling Competitor hours Ancillary services Provider availability Support staff Financial costs Project Scope This project included three clinics within the TC at the University of Michigan Health System: Adult Pulmonary, Adult Nephrology, and Adult General Otolaryngology clinics. Within these clinics, the team examined the operational factors that needed to be considered for these clinics to offer extended hours. The team examined potential benefits that extending hours could provide to the three clinics and the University of Michigan Health System. The team also examined satellite clinics that offer the same services as TC, but are still part of the University of Michigan Health Systems. The team examined operational factors and current services at the satellite locations. Any task not connected to these clinics was not included in this project. Specifically, the team did not examine any other clinic’s scheduling data, patient population, provider, or appointment schedules. METHODS The following three sections describe the data collection and analysis. Conducted Interviews The team interviewed 3 clinic managers from the Adult Pulmonary, Adult Nephrology, and Adult General Otolaryngology clinics. The team developed a questionnaire, with the help of the Senior Project Manager, Lean Coach, and Engineering Fellow, which can be seen in Appendix A. The team used the questionnaire during the interviews to gain understanding of how the clinics run and the requirements for a clinic to run. The team then interviewed all 3 clinic managers a second time with a draft of the feasibility checklist. These interviews were conducted to gain feedback on the current content and discover any aspects missing from the checklist. The first set of interviews with the 3 clinic managers allowed the team to: Understand what is needed for each of the three individual clinics to function during extended hours (e.g. People, equipment) 2 Gain a greater understanding of the types of patients each clinic sees Understand constraints in formulating a plan for extending hours Understand which areas in each department that have the greatest need for expansion Gain input about when and where the extended hours should take place Gain input on the degree of feasibility for earlier morning and later evening hours and for offsite clinic hours The second set of interviews with the 3 clinic managers allowed the team to: Gain a managers perspective of the feasibility checklist Discover which questions were useful Combine similar ideas Find missing aspects in checklist Fill out the checklist for each clinic Performed Benchmarking The team performed benchmarking both internally and externally. The team benchmarked the Urology department at TC to gain information on their extended hours program. The team also benchmarked the University of Michigan Health System’s main competitors to find the hours of operation at clinics similar to those at the TC. Internal Benchmarking The Urology department at TC launched extended hours in September 2013; therefore, the team benchmarked the Adult Urology clinic in the TC through one interview. Attached in Appendix B is the questionnaire the team used to gain information from the Adult Urology clinic manager about the department’s extended hours program and what research went into developing an extended hours program. External Benchmarking The team benchmarked local competitors: Beaumont Health System, St. Joseph Mercy Hospital (IHA), and the Henry Ford Health System. The team also benchmarked Mayo Clinic, Cleveland Clinic, and Johns Hopkins. The benchmarking was done through phone calls and Internet research. The benchmarked data was analyzed to compare current hours and the implementation of extending hours. The team benchmarked these clinics because they are the University of Michigan’s Health System’s competitors at both local and national levels. Analyzed MiChart Scheduling Data The team received MiChart data from October 2012 to October 2013 for the Adult Pulmonary, Adult Nephrology, and Adult General Otolaryngology clinics in the TC. This data included information on: Visit types Name of providers seeing patients The date the information was created The appointment status Cancellation reason, if applicable 3 Date and time appointment is scheduled The lead-time in weeks for new patients to be seen The team analyzed current access and identified opportunities for improvement from the data. First, the team used the data to calculate: Overall new patient access New patient access by appointment types Number of new patient appointments that need to be seen to increase patient access to 80% Second, the team used the data to analyze: New patient appointment status by month New patient appointment volume per month Access of each new patient by provider Correlations between cancellations and lead-time The above analysis was done for each of the three clinics. The data provided insight into problems within each of the three clinics, and the severity of these problems will determine the feasibility of extending hours. FINDINGS FROM DATA Below are the findings from our data collection and analysis. Interviews From the first interviews, the team discovered that there are three main limitations when expanding hours within a clinic: (1) specific ancillary services and testing, (2) provider type, and (3) patient preference for providers. From the second interviews, the team gained a greater understanding of the three clinics and was able to fill out more of the feasibility checklist for each of the three clinics. For the Adult Pulmonary clinic, the team found that they are currently operation at approximately 85% capacity and there is room to improve. For the Adult Nephrology clinic, the team found that most of the providers that work in Adult Nephrology at the TC are not specialized, meaning they see all types of patients. For the Adult General Otolaryngology clinic, the team found that providers do not currently make up missed clinic hours. Each of these three clinics has differing needs. More findings from the interview can be found in the partially completed clinic feasibility checklists located in Appendix F. Benchmarking The following are the findings from the benchmarking with the TC Adult Urology clinic and the competitors of the University of Michigan Health Systems. Satellite Locations are a Viable Option for Extending Hours 4 From the interview that the Adult Urology department it was discovered that the Urology department has extended evening hours two Wednesdays every month at TC and two Saturdays every month at a satellite location. Benchmarking with the Adult Urology clinic allowed the team to understand that satellite locations are a possible option for use in extended hours. Some satellite locations in the University of Michigan Health System already have extended hours and have the ability to provide resources for extended hours. These satellite locations may also: Expand the market Maximize already available resources Provide care closer to where patients live Few Competitors Have Extended Hours Four out of six competitors do not have extended hours. The two competitors that do have extended hours hold the hours at satellite locations. Table 1 below shows TC’s main local and national competitors and their competitor’s hours. Table 1: Hours of Operation Comparison Pulmonary M-F UMHS TC [1]* 8am-5pm M-F 8am-8pm; Beaumont [3]* Sat 9am-1pm** Local M-Th Competitors 7am-7pm; Henry Ford [4]* F 7am-5pm** M-F IHA [5]* 8am-5pm M-F Cleveland Clinic [6]* 8am-5pm National M-F Johns Hopkins [7]* Competitors 8:30am-5pm M-F Mayo Clinic [8]* 8am-5pm Nephrology M-F 8am-5pm Otolaryngology M-F 8am-5pm M-F 8am-4:30pm M-F 8am-4:30pm M-Th 7am-7pm; F 7am-5pm** M-F 8am-5pm M-F 8am-5pm M-F 8am-5pm M-F 8am-5pm M-F 8am-5pm M-F 8am-5pm M-F 8am-5pm M-F 8am-5pm M-F 8am-5pm *Numbers refer to reference section **Bolded represents hours that differ from the TC Table 1 shows that the Henry Ford Health System has extended hours. The extended hours take place at their Novi satellite location for Pulmonary and Nephrology. Table 1 also shows that the Beaumont Health Systems has extended hours. The extended hours take place at their Sterling Heights satellite location for Pulmonary only. All other hours are Monday through Friday during normal workday hours (8 am to 5 pm). 5 MiChart Scheduling Data Presented below are the findings the team has gathered from analyzing the MiChart Scheduling data, based on the outline in the methods section above. The data was collected from October 2012 to October 2013. Access Rates Patient access is the percentage of new patients that are seen by a provider within 4 weeks of scheduling an appointment for the specified clinic. The faculty group practice has a goal of 80% of new patients seen within 4 weeks. The MiChart Scheduling data indicated that for the Adult Pulmonary, Adult Nephrology, and Adult General Otolaryngology clinics the access rates are 72%, 50%, and 23%, respectively. Percentage of Patients Seen Figure 1 below shows the lead-time versus the percentage of patients seen for the Adult Pulmonary clinics through the University of Michigan Health Systems. Figure 1 shows that 72% of patients are seen within 4 weeks. Figure 2 below shows a yearly breakdown by month of how long patients waited to be seen from when they created their appointment. 45% 40% 35% 30% 25% 20% 15% 10% 5% 0% 41% 31% 21% 7% 0 to 2 Weeks 2 to 4 Weeks 4 to 8 Weeks Greater than 8 Weeks Lead-Time Figure 1: Adult Pulmonary new patient appointment lead time (Source: MiChart Data. Data Collection Period: October 2012 to October 2013. Sample size: 3701) 6 Figure 2: Adult Pulmonary new patient appointment lead time by month (Source: MiChart Data. Data Collection Period: October 2012 to October 2013. Sample size: 3701) Pulmonary currently offers services at three locations: TC, Briarwood Health Clinic, and Brighton Health Clinic. Figures 1 and 2 above show data from all three clinics combined. The breakdown of each clinic can be seen in Appendix C. Percentage of Patients Seen Figure 3 below shows the lead-time versus the percentage of patients seen for the Adult Nephrology clinic at TC. Figure 3 shows that 50% of patients are seen within 4 weeks. Figure 4 below shows a yearly breakdown by month of how long patients waited to be seen from when they created their appointment. 45% 40% 35% 30% 25% 20% 15% 10% 5% 0% 39% 31% 19% 11% 0 to 2 Weeks 2 to 4 Weeks 4 to 8 Weeks Greater than 8 Weeks Lead-time Figure 3: Adult Nephrology new patient new patient appointment lead time (Source: MiChart Data. Data Collection Period: October 2012 to October 2013. Sample size: 1589) 7 Figure 4: Adult Nephrology new patient appointment lead time by month (Source: MiChart Data. Data Collection Period: October 2012 to October 2013. Sample size: 1589) Percentage of Patients Seen Figure 5 below shows the lead-time versus the percentage of patients seen for the Adult General Otolaryngology clinic at TC. Figure 5 shows that 29% of patients are seen within 4 weeks. Figure 6 below shows a yearly breakdown by month of how long patients waited to be seen from when they created their appointment. 70% 60% 50% 40% 30% 20% 10% 0% 60% 23% 11% 6% 0 to 2 Weeks 2 to 4 Weeks 4 to 8 Weeks Greater than 8 Weeks Lead-time Figure 5: Adult General Otolaryngology new patient appointment lead time (Source: MiChart Data. Data Collection Period: October 2012 to October 2013. Sample size: 1072) 8 Figure 6: Adult General Otolaryngology new patient appointment lead time by month (Source: MiChart Data. Data Collection Period: October 2012 to October 2013. Sample size: 1072) Percentage of Cancellations Correlation Between Cancellations and Lead-Time Figures 7, 8 and 9 below show correlations between the lead-time of the appointment and appointment cancellations for new patients for the Adult Pulmonary, Adult Nephrology and Adult General Otolaryngology clinics, respectively. These figures indicate that the greater the lead-time, the more likely the patient will cancel his/her appointment. Appointment cancellations indicate losses in potential revenue. 45% 40% 35% 30% 25% 20% 15% 10% 5% 0% Less than 2 weeks 2-4 weeks 4-8 weeks greater than 8 weeks Lead Time Figure 7: Adult Pulmonary correlation between lead time and cancellations Source: MiChart Data. Data Collection Period: October 2012 to October 2013. Sample size: 5627) 9 Percentage of Cancellations 60% 50% 40% 30% 20% 10% 0% Less than 2 weeks 2-4 weeks 4-8 weeks Greater than 8 weeks Lead Time Figure 8: Adult Nephrology correlation between lead time and cancellations Percentage of Cancellations Source: MiChart Data. Data Collection Period: October 2012 to October 2013. Sample size: 2768) 60% 50% 40% 30% 20% 10% 0% Less than 2 weeks 2-4 weeks 4-8 weeks Greater than 8 weeks Lead Time Figure 9: Adult General Otolaryngology correlation between lead time and cancellations Source: MiChart Data. Data Collection Period: October 2012 to October 2013. Sample size: 2006) From Figures 7, 8, and 9 it can be seen that there a positive correlation between the length of the lead time and the percentage of new patient cancellations. Projected Needs From the MiChart data the team projected how many more new patients each of the three clinics would need to see in order to bring access rates at the goal of 80%. Table 2 below shows the current access of each clinic studied along with the number of new patients that need to be seen yearly, monthly, and weekly. 10 Table 2: Number of New Patients that need to be seen to increase access to 80% Clinic Current Number Number Needed Number Access Needed Yearly Monthly Needed Weekly Adult Pulmonary 72% 307 26 6 Adult Nephrology 50% 473 40 10 Adult General 29% 547 46 11 Otolaryngology (Source: MiChart Data. Data Collection Period: October 2012 to October 2013. Sample size: 6382) The numbers in Table 2 were calculated based on the total number of patients seen in the past year, and then multiplied by 80% to get a target number of new patients that need to be seen in less than 4 weeks of creating an appointment. Then by taking the new total, the team calculated approximately how many more new patients needed to be seen in a yearly span. The monthly and weekly numbers were found by dividing the yearly amount by 12 and 50, respectively. Appointment Status The following charts, Figure 10, 11, and 12, show a monthly breakdown of the total new patient expected clinic volume each month. For each month, the bars indicate how many new patients completed their appointment, did not show up to their appointment, or left the clinic without being seen by a provider. For example, in October 2012 in the Adult Pulmonary clinic had 283 new patients complete their appointments, 24 new patients that did not show up to their appointment, and no new patients that left the clinic without being seen. Figure 10: Adult Pulmonary new patient monthly appointment volumes (Source: MiChart Data. Data Collection Period: October 2012 to October 2013. Sample size: 3963) 11 Figure 11: Adult Nephrology new patient monthly appointment volumes (Source: MiChart Data. Data Collection Period: October 2012 to October 2013. Sample size: 1802) Figure 12: Adult General Otolaryngology new patient monthly appointment volumes (Source: MiChart Data. Data Collection Period: October 2012 to October 2013. Sample size: 1236) From the figures above, the team determined the average monthly volume of new patient appointments. These numbers can be seen in Table 3. Table 3: Average number of new patients by appointment status Clinic Completed No Show Left without Being Seen Adult Pulmonary 285 20 0 Adult Nephrology 123 15 0 Adult General Otolaryngology 82 13 0 (Source: MiChart Data. Data Collection Period: October 2012 to October 2013. Sample size: 7001) Other Calculations The team analyzed new patient access by appointment type as well as by provider. These figures and analysis can be seen in Appendix D. 12 FEASBILITY CHECKLIST The main deliverable from this project is a feasibility checklist. The following sections discuss the checklist methods, findings, and conclusions. Checklist Methods The team provided a feasibility checklist that will be used by future clinic departments when considering extending hours. These questions have been developed through the interviews conducted with the Adult Pulmonary, Adult Nephrology, and Adult General Otolaryngology clinics, the benchmarking with the Adult Urology clinic manager, and client and coordinator input. The final checklist can be seen in Appendix E. Checklist Findings From the interviews, the team concluded that there are several topics to consider when examining the feasibility of expanding hours of any hospital clinic, including that of the University of Michigan’s TC. The five main topics to be considered are: (1) Market – Business Need, (2) Needs Assessment, (3) Operational Planning, (4) Financial Evaluation, and (5) Implementation Planning. Checklist Conclusions The team has partially completed the feasibility checklist of the Adult Pulmonary, Adult Nephrology, and Adult General Otolaryngology clinics. These partially completed checklists can be seen in Appendix F. The team recommends that each clinic continue to fill out the checklist. CONCLUSIONS Each clinic’s needs differ according to in-clinic procedures. Clinics also use different ancillary services according to patient and provider need. Ancillary services do not offer the same hours as outpatient clinics. While examining the possibility of expanding hours it was discovered that some satellite locations currently offer Saturday hours for patient appointments and emergency clinics. Currently, some offsite clinics offer similar services to that at TC, specifically for the Adult Pulmonary, Adult Nephrology, and Adult General Otolaryngology clinics. These satellite clinics offer the possibility to increase patient access and are a feasible option. Through benchmarking, the team discovered that four out of six of the University of Michigan Health System’s competitors do not offer extended hour services. While the two competitors that do offer extended hours use satellite locations and are local competitors. TC offering extended hours could increase not only patient access, but also the population base as a whole. The MiChart data showed that there is an access issue in the Adult Pulmonary, Adult Nephrology, and Adult Otolaryngology clinics operating at access rates of 72%, 50%, and 29%, respectively. To reach an access of 80% based on the data, the Adult Pulmonary, Adult Nephrology, and Adult General Otolaryngology clinics need to see 6, 13 10, and 11 new patients, respectively, per week. Lastly, there is a possible positive correlation between cancellations and long lead times. RECOMMENDATIONS The following sections describe the recommendations in regards to the checklist, satellite locations, and in clinic expansion. Feasibility Checklist The team recommends that before considering expanded hours a clinic should fill out the feasibility checklist based on specific clinic information. After filling out the checklist, the clinic should perform MiChart data analysis to find access rates and correlations. Next, a patient survey should be created in order to find when patients would want extended hours, if they would go to them, and where. The clinic should then do a clinic staff survey to find out if staff is willing to flex their schedules, change the hours of schedules, or work overtime. Lastly, the clinic should research direct competitors to see if they have extended hours and if they hold the hours at satellite locations or at their main campus. Satellite Locations Satellite locations are a viable option for expanding hours. A satellite location should only be used for extending hours on Saturdays. Some of the satellite locations within the University of Michigan Health System are already open on Saturdays. If the locations are already open, there is a possibility for clinics to take advantage of possible unused capacity. Satellite locations already open on Saturdays could also give a clinic infrastructure support. Lastly, satellite locations could increase convenience for patients in regards to hours, parking, and location. In Clinic Expansion Before considering expanding hours the following should be optimized to capacity: Rooms Providers Scheduling Template Equipment If the clinic is currently operating at full capacity and is still considering expanding hours, the clinic should explore early or late expanded hours within the TC. OPORTUNITIES FOR FUTURE ANALYSIS To accurately compare the University of Michigan’s Health System’s competitors, the following subjects must be examined: Lead-time for competitors Access rates for competitors Number of patients seen daily Use of overbooking concepts Use of satellite locations 14 EXPECTED IMPACT Clinics offering extended hours could increase the following: Access for new patient appointments Patient satisfaction Room utilization Patient population Financial margin 15 REFERENCES [1] UofMHealth.org, 1995. [Online]. Available: UofMHealth.org, http://www.uofmhealth.org/our-locations [Accessed: October 2013]. [2] Senior Project Manager, private communication. September 2013. [3] Beaumont Health System Call Center, private communication. October 2013. [4] Henry Ford Health System Call Center, private communication. October 2013. [5] IHA Health System Call Center, private communication. October 2013. [6] Cleveland Clinic System Call Center, private communication. October 2013. [7] Johns Hopkins Call Center, private communication. October 2013. [8] Mayo Clinic Call Center, private communication. October 2013. 16 Appendix A. Interview Questionnaire for Clinic Managers The following questionnaire was verbally read in meetings with the Adult Pulmonary, Adult Nephrology, and Adult General Otolaryngology clinic managers. What are the people requirements to run your clinic? i.e. number of clerks, providers, nurses, etc. o How many different types of providers? Are all types of providers there on a daily basis? Or what are the times and days of the week they are available? Number of providers there on a daily basis? (Or average number if it changes) What ancillary services do your patients require? Do they vary per provider? Per appointment reason? Per clinic? Are there any specialists needed? Nutritionists, social workers, residents, etc. Is your current staff being utilized to capacity? Do certain patients have priority in scheduling? Return patients, new patients, etc. What is the average return visit time for returning patients? What is the average length of an appointment for new patients? Return patients? How long is the designated spot for each appointment? Does it differ for new and return patients? What staff would be affected the most by extending hours? Doctors, nurses, clerks, etc. What is the best way to contact you with further questions? A-1 Appendix B. Interview Questionnaire for Urology Clinic Manager What factors did you consider when you started to look at extending hours? Did you consider weekday and weekend extension? Did you look into what other facilities (benchmarking) have done? If so, who? What is working/what is not, as in provider issues, nurses, MA’s, clerks? o Did you have to hire any new employees or expand the amount of hours people worked? What was the expected improvement or target improvement? Are there things you wish you had considered before beginning? What specific ancillary services did you look into also having to expand? Was financial cost an objective? Did you consider it, and how much weighting did you put on it? When are your expanded hours and how many were added? B-1 Appendix C. Figures for Pulmonary Clinics Percentage of Patients Seen Figure C-1 below shows the lead-time versus the percentage of patients seen for the Adult Pulmonary clinic at TC. From the following, it can be seen that 74% of patients are seen within for weeks. Figure C-2 below shows a yearly breakdown by month of how long patients waited to be seen from when they created their appointment at TC. 45% 40% 35% 30% 25% 20% 15% 10% 5% 0% 42% 32% 18% 8% 0 to 2 Weeks 2 to 4 Weeks 4 to 8 Weeks Greater than 8 Weeks Lead-Time Figure C-1: TC Adult Pulmonary new patient appointment lead time (Source: MiChart Data. Data Collection Period: October 2012 to October 2013. Sample size: 2867) Figure C-2: TC Adult Pulmonary new patient appointment lead time by month (Source: MiChart Data. Data Collection Period: October 2012 to October 2013. Sample size: 2867) Figure C-3 below shows the lead-time versus the percentage of patients seen for the Adult Pulmonary clinic at Briarwood Health Clinic. From the following, it can be seen that 78% of patients are seen within for weeks. Figure C-4 below shows a yearly breakdown by month of how long patients waited to be seen from when they created their appointment at Briarwood Health Clinic. C-1 Percentage of Patients Seen 60% 50% 48% 40% 30% 30% 18% 20% 10% 3% 0% 0 to 2 Weeks 2 to 4 Weeks 4 to 8 Weeks Greater than 8 Weeks Lead-Time Figure C-3: Briarwood Health Clinic Adult Pulmonary new patient appointment lead time (Source: MiChart Data. Data Collection Period: October 2012 to October 2013. Sample size: 532) Figure C-4: Briarwood Health Clinic Adult Pulmonary new patient appointment lead time by month (Source: MiChart Data. Data Collection Period: October 2012 to October 2013. Sample size: 532) Figure C-5 below shows the lead-time versus the percentage of patients seen for the Adult Pulmonary clinic at Brighton Health Clinic. From the following, it can be seen that 78% of patients are seen within for weeks. Figure C-6 below shows a yearly breakdown by month of how long patients waited to be seen from when they created their appointment at Brighton Health Clinic. C-2 Percentage of Patients Seen 60% 53% 50% 40% 30% 20% 22% 17% 9% 10% 0% 0 to 2 Weeks 2 to 4 Weeks 4 to 8 Weeks Greater than 8 Weeks Lead-Time Figure C-5: Brighton Health Clinic Adult Pulmonary new patient appointment lead time (Source: MiChart Data. Data Collection Period: October 2012 to October 2013. Sample size: 302) Figure C-6: Brighton Health Clinic Adult Pulmonary new patient appointment lead time by month (Source: MiChart Data. Data Collection Period: October 2012 to October 2013. Sample size: 302) C-3 Appendix D. Patient Type and Provider Access Data Figures Percentage of Patients Figure D-1 below shows the percentage of patients seen within 4 weeks by appointment type at the Adult Pulmonary clinics through the University of Michigan Health Systems. 100% 90% 80% 70% 60% 50% 40% 30% 20% 10% 0% 100% 73% 67% 63% 51% 50% 44% Patient Type Figure D-1: Adult Pulmonary percentage of new patients seen within 4 weeks by appointment type (Source: MiChart Data. Data Collection Period: October 2012 to October 2013. Sample size: 3701) Percentage of Patients Figure D-2 below shows the percentage of patients seen within 4 weeks by appointment type at the Adult Nephrology clinics at TC. 100% 90% 80% 70% 60% 50% 40% 30% 20% 10% 0% 100% 82% 73% 70% 37% 26% 15% 0% Patient Type Figure D-2: Adult Nephrology percentage of new patients seen within 4 weeks by appointment type (Source: MiChart Data. Data Collection Period: October 2012 to October 2013. Sample size: 1589) Figure D-3 below shows the percentage of patients seen within 4 weeks by provider at the Adult General Otolaryngology clinics at TC. D-1 100% Percentage of Patients 90% 80% 70% 60% 50% 40% 30% 20% 10% 0% A B Provider Code C Figure D-3: Adult General Otolaryngology percentage of new patients seen within 4 weeks by provider (Source: MiChart Data. Data Collection Period: October 2012 to October 2013. Sample size: 1037) Figure D-4 below shows the percentage of patients seen within 4 weeks by provider at the Adult Pulmonary clinics through the University of Michigan Health Systems. Figure D-5 below shows the percentage of patients seen within 4 weeks by provider at the Adult Nephrology clinics at TC. D-2 100% 90% Percentage of Patients 80% 70% 60% 50% 40% 30% 20% 10% A B C D E F G H I J K L M N O P Q R S T U V W X Y Z AA BB CC DD EE FF GG HH II JJ KK LL MM NN OO PP QQ RR SS TT UU VV WW XX YY ZZ AAA BBB 0% Provider Code Figure D-4: Adult Pulmonary percentage of new patients seen within 4 weeks by provider (Source: MiChart Data. Data Collection Period: October 2012 to October 2013. Sample size: 3701) D-3 100% 90% Percentage of Patients 80% 70% 60% 50% 40% 30% 20% 10% 0% Provider Code Figure D-5: Adult Nephrology percentage of new patients seen within 4 weeks by provider (Source: MiChart Data. Data Collection Period: October 2012 to October 2013. Sample size: 1589) D-4 Appendix E. Feasibility Checklist Market—Business Need: Define your patient population by program area. Identify where there is growth. Identify where there is a deficit. Define your goals for your patient populations. Define your market projection. Define your health care needs. Identify any changes in the market. Identify your current service offerings. Identify where you currently have services. Identify if these services are under utilized. Identify if you are considering a satellite location. Identify the hours of operation at the satellite location. Needs Assessment: Define your current access. Identify specific appointment types where your access is lower. Identify if your provider template is at capacity. Identify client demand. Identify if your rooms are being utilized to capacity. Identify if your current staff is being utilized to capacity. Identity if you are providing make up clinics when providers cancel. Identify if your currents days and hours are at capacity. Define your cancel appointment back-up procedure. Wait list? Overbooking? Other? Identify who your direct competitors are. Define who provides services similar to you. Define how your patients rate your overall services. Identify your customer satisfaction with lead-time. Identify how your patients rate provider performance. Operational Planning: Identify your clinical resources by service. Identify equipment needed for: New patient appointments. Return patient appointments. Procedures that take place during appointments. Identify if you need MA’s, PA’s, clerks, etc. during an appointment. E-3 Identify ancillary services needed. Identify the current hours of operation for your ancillary services. Identify if you have satellite location/s that have the same services. Identify hours of operation for ancillary services at satellite location/s. Identify if there are any process improvements in the already instated hours. Define your current recruiting plan. Identify provider/s willing to work at the different times. Identify if you will consider and have the capacity to hire. Identify MA’s, PA’s, etc. willing to work at the different times. If none, identify if you will consider and have the capacity to hire. Conduct a survey on faculty willingness. Financial Evaluation Complete ROI. Define your estimated cost for expansion. Identify your variable costs. Identify your staffing costs. Identify your invariable costs. Identify your equipment costs. Identify your facility costs. Define your estimated revenue. Implementation Planning Conduct a patient survey to identify possible hours. Identify how are you proposing to implement extended hours. Define when you would like to extend these hours. Evening? Morning? Weekend? Define how often you are planning on holding these extended hours. Daily basis? Select days in a week? Monthly basis? Identify where you would like to extend these hours. On-site? Satellite location? Identify if there is a current flexibility within your provider’s schedule. Identify if there is patient demand for earlier or later hours. Identify if there is room availability during desired hours. Identify if room capacity is at full utilization. Identify how soon can you launch these extended hours. E-4 Appendix F. Partially Completed Feasibility Checklists for Clinics Below are the partially completed checklists for the three clinics, Adult Pulmonary, Adult Nephrology, and Adult Otolaryngology completed by the team through interviews with the clinic managers. Pulmonary Checklist: Market—Business Need: Define your patient population by program area. Identify where there is growth. COPD and Cystic fibrosis Identify where there is a deficit. Only 1 provider does COPD Define your goals for your patient populations. Define your market projection. Define your health care needs. Identify any changes in the market. Identify your current service offerings. Identify where you currently have services. Taubman, Brighton, Briarwood, Northville Identify if these services are under utilized. Identify if you are considering a satellite location. Identify the hours of operation at the satellite location. Brighton: M-TH 7am-7pm, F 7:30am-5:30pm, Sat 8am-12pm Briarwood: MW 8am-7pm, T,TH,F 8am-5pm, Sat 8am-12pm Northville: Future Site Needs Assessment: Define your current access. New Patients being seen in less than 4 weeks is 72% Identify specific appointment types where your access is lower. NP Sarcoid has the lowest access at only 44%. Identify if your provider template is at capacity. Identify client demand. Identify if your rooms are being utilized to capacity. Operating at approximately 85% capacity Identify if your current staff is being utilized to capacity. Operating at approximately 85% capacity Identity if you are providing make up clinics when providers cancel. Strongly recommended Identify if your currents days and hours are at capacity. Operating at approximately 85% capacity F-1 Define your cancel appointment back-up procedure. Wait list? Overbooking? Other? Identify who your direct competitors are. Beaumont Health System, Mayo Clinic, Cleveland Clinic, Henry Ford, IHA Identify competitor’s current service hours. TC M-F 8 am-5pm Beaumont M-F 8 am-5pm, Sat 9am-1pm Mayo M-F 8 am-5pm Cleveland M-F 8 am-5pm Henry Ford M-TH 7am-7pm, F 7am-5pm IHA M-F 8 am-5pm Define how your patients rate your overall services. Identify your customer satisfaction with lead-time. Identify how your patients rate provider performance. Operational Planning: Identify your clinical resources by service. Identify equipment needed for: New patient appointments. Return patient appointments. Procedures that take place during appointments. Identify if you need MA’s, PA’s, clerks, etc. during an appointment. 1 provider, 2 MA (2 MA's per provider), and 1 clerk Identify ancillary services needed. PFT, Radiology (General CT, HRCT), Phlebotomy Identify the current hours of operation for your ancillary services. PFT: M-F 8am-5pm Radiology: M-F 7:30am-6pm Phlebotomy: M-F 8:30am-3:30pm Identify if you have satellite location/s that have the same services. Briarwood: PFT, Radiology, Phlebotomy Brighton: Radiology, Phlebotomy Northville: Identify hours of operation for ancillary services at satellite location/s. Briarwood: PFT: M 1pm-5pm, T-F 8am-5pm Radiology: M-F 7:30am-5pm, Sat 9am-1pm Phlebotomy: MW 8am-7pm, T,TH,F 8am-5pm, Sat 8am-12pm Brighton: Radiology: M-TH 7:30am-7:30pm, F 7:30am-5:30pm, Sat 8:30am-12:30pm Phlebotomy: M-TH 7am-7pm, F 7:30am-5:30pm, Sat 8am-12pm F-2 Identify if there are any process improvements in the already instated hours. Define your current recruiting plan. Identify provider/s willing to work at the different times. Identify if you will consider and have the capacity to hire. Identify MA’s, PA’s, etc. willing to work at the different times. If none, identify if you will consider and have the capacity to hire. Conduct a survey on faculty willingness. Financial Evaluation Complete ROI. Define your estimated cost for expansion. Identify your variable costs. Identify your staffing costs. Identify your invariable costs. Identify your equipment costs. Identify your facility costs. Define your estimated revenue. Implementation Planning Conduct a patient survey to identify possible hours. Identify how are you proposing to implement extended hours. Define when you would like to extend these hours. Evening? Morning? Weekend? Probably most plausible 6:30am-7am Define how often you are planning on holding these extended hours. Daily basis? Select days in a week? Monthly basis? Identify where you would like to extend these hours. On-site? Satellite location? Identify if there is a current flexibility within your provider’s schedule. Identify if there is patient demand for earlier or later hours. Identify if there is room availability during desired hours. Identify if room capacity is at full utilization. Identify how soon can you launch these extended hours. F-3 Nephrology Checklist: Market—Business Need: Define your patient population by program area. Identify where there is growth. Identify where there is a deficit. Define your goals for your patient populations. Define your market projection. Define your health care needs. Identify any changes in the market. Identify your current service offerings. Identify where you currently have services. Taubman, Brighton Identify if these services are under utilized. Identify if you are considering a satellite location. Identify the hours of operation at the satellite location. Brighton: M-TH 7am-7pm, F 7:30am-5:30pm, Sat 8am-12pm Needs Assessment: Define your current access. New Patients being seen in less than 4 weeks is 50% Identify specific appointment types where your access is lower. NP has the lowest access at 0%. While the second worst is NP PHARMD at 15% Identify if your provider template is at capacity. Identify client demand. Identify if your rooms are being utilized to capacity. Identify if your current staff is being utilized to capacity. Identity if you are providing make up clinics when providers cancel. Identify if your currents days and hours are at capacity. Define your cancel appointment back-up procedure. Wait list? Overbooking? Other? Identify who your direct competitors are. Beaumont Health System, Mayo Clinic, Cleveland Clinic, Henry Ford, IHA Identify competitor’s current service hours. TC M-F 8 am-5pm Beaumont M-F 8 am-4:30pm Mayo M-F 8 am-5pm Cleveland M-F 8 am-5pm Henry Ford M-TH 7am-7pm, F 7am-5pm IHA M-F 8 am-5pm Define how your patients rate your overall services. Identify your customer satisfaction with lead-time. Identify how your patients rate provider performance. Operational Planning: F-4 Identify your clinical resources by service. Identify equipment needed for: New patient appointments. Return patient appointments. Procedures that take place during appointments. Identify if you need MA’s, PA’s, clerks, etc. during an appointment. Identify ancillary services needed. Identify the current hours of operation for your ancillary services. Identify if you have satellite location/s that have the same services. Identify hours of operation for ancillary services at satellite location/s. Identify if there are any process improvements in the already instated hours. Define your current recruiting plan. Identify provider/s willing to work at the different times. Identify if you will consider and have the capacity to hire. Identify MA’s, PA’s, etc. willing to work at the different times. If none, identify if you will consider and have the capacity to hire. Conduct a survey on faculty willingness. Financial Evaluation Complete ROI. Define your estimated cost for expansion. Identify your variable costs. Identify your staffing costs. Identify your invariable costs. Identify your equipment costs. Identify your facility costs. Define your estimated revenue. Implementation Planning Conduct a patient survey to identify possible hours. Identify how are you proposing to implement extended hours. Define when you would like to extend these hours. Evening? Morning? Weekend? Define how often you are planning on holding these extended hours. Daily basis? Select days in a week? Monthly basis? Identify where you would like to extend these hours. On-site? Satellite location? Identify if there is a current flexibility within your provider’s schedule. Identify if there is patient demand for earlier or later hours. Identify if there is room availability during desired hours. Identify if room capacity is at full utilization. Identify how soon can you launch these extended hours. F-5 Otolaryngology Checklist: Market—Business Need: Define your patient population by program area or subspecialties. General Otolaryngology Identify where there is growth. Growth within General Otolaryngology Identify where there is a deficit. Provider availability, resources, equipment, space Define your goals for your patient populations. Define your market projection. Define your health care needs. Identify any changes in the market. General is likely to grow. Identify your current service offerings. Identify where you currently have services. Taubman, Livonia Identify if these services are under utilized. Identify if you are considering a satellite location. Identify the hours of operation at the satellite location. Livonia: M-TH 7:30am-6pm, F 8am-5pm, Sat 9am-1pm Needs Assessment: Define your current access. General New Patients being seen in less than 4 weeks is 29% Identify specific appointment types where your access is lower. Identify if your provider template is at capacity. Identify client demand. Identify if your rooms are being utilized to capacity. Monday through Thursday yes, capacity on Fridays Identify if your current staff is being utilized to capacity. Identity if you are providing make up clinics when providers cancel. Not right now Identify if your currents days and hours are at capacity. Monday through Thursday yes, capacity on Fridays Define your cancel appointment back-up procedure. Wait list? Overbooking? Other? Wait list, although not being utilized effectively Identify who your direct competitors are. F-6 Beaumont Health System, Mayo Clinic, Cleveland Clinic, Henry Ford, IHA Identify competitor’s current service hours. TC M-F 8 am-5pm Beaumont M-F 8 am-4:30pm Mayo M-F 8 am-5pm Cleveland M-F 8 am-5pm Henry Ford M-F 8 am-5pm IHA M-F 8 am-5pm Define how your patients rate your overall services. Have a 98.6% overall satisfaction rating Identify your customer satisfaction with lead-time. A lot of complaints about long lead-times Identify how your patients rate provider performance. Rating of care and providers is very high Operational Planning: Identify your clinical resources by service. Identify equipment needed for: New patient appointments. Flexible scopes and any room available Return patient appointments. Depends on patient type and provider Procedures that take place during appointments. Scopes and biopsy equipment Identify if you need MA’s, PA’s, clerks, etc. during an appointment. The number depends on the day. PA's are not needed. 1 MA per provider, at least 1 clerk to check in and out patients Identify ancillary services needed. Radiology (MRI, CT), Phlebotomy, Pathology Identify the current hours of operation for your ancillary services. Radiology: M-F 7:30am-6pm Phlebotomy: M-F 8:30am-3:30pm Pathology: Identify if you have satellite location/s that have the same services. Livonia: Radiology (MRI), Phlebotomy, Pathology Identify hours of operation for ancillary services at satellite location/s. Identify if there are any process improvements in the already instated hours. Improve clinic flow, look into Fridays, increase overall utilization Define your current recruiting plan. Identify provider/s willing to work at the different times. Identify if you will consider and have the capacity to hire. Identify MA’s, PA’s, etc. willing to work at the different times. If none, identify if you will consider and have the capacity to hire. F-7 Conduct a survey on faculty willingness. Financial Evaluation Complete ROI. Define your estimated cost for expansion. Identify your variable costs. Identify your staffing costs. Identify your invariable costs. Identify your equipment costs. Identify your facility costs. Define your estimated revenue. Implementation Planning Conduct a patient survey to identify possible hours. Identify how are you proposing to implement extended hours. Define when you would like to extend these hours. Evening? Morning? Weekend? Define how often you are planning on holding these extended hours. Daily basis? Select days in a week? Monthly basis? Identify where you would like to extend these hours. On-site? Satellite location? Identify if there is a current flexibility within your provider’s schedule. Identify if there is patient demand for earlier or later hours. Identify if there is room availability during desired hours. Identify if room capacity is at full utilization. Identify how soon can you launch these extended hours. F-8