"Manage The Disease" presentation.
advertisement

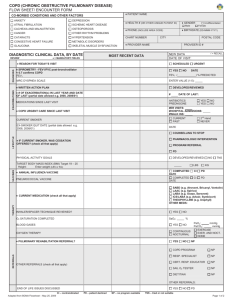
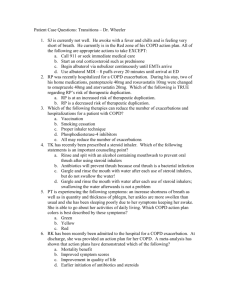
White Memorial Medical Center January 31, 2014 Los Angeles CA COPD: Managing the Disease Not The Symptoms Patrick J. Dunne, MEd, RRT, FAARC HealthCare Productions, Inc. Fullerton, CA 92838 pjdunne@sbcglobal.net Disclosure Professional relationships with: Monaghan Medical Corporation Mylan Specialty, LP Ohio Medical Corporation Objectives Review the provisions / timelines of Medicare’s Hospital Readmission Reduction Program; List the clinical and economic impact of COPD and associated comorbidities; List the evidence-based care guidelines for the inpatient treatment of a COPD exacerbation, and Describe potential strategies to help reduce all-cause 30-day COPD readmissions. Hospital Readmission Reduction Program Section 3025 Affordable Care Act Effective FY 2013 (10/1/12 - 9/30/13) 2nd of 2 new payment policies Financial penalties for excessive 30-day readmissions 3 Targeted conditions Acute MI (19.9%); CHF (24.5%); Pneumonia (18.2%) Additional conditions to be added in FY 2015 Hospitals identified nationwide FY 2013 - - 2,213 hospitals w/ $280 million in penalties (up to 1%) FY 2014 - - 2,225 hospitals w/ $227 million in penalties (up to 2%) FY 2015 - - penalty up to 3% of total Medicare payments Page 113: “We believe the COPD measure warrants inclusion in the Hospital Readmission Reduction Program for FY 2015” Fiscal Year 2015 October 1, 2014 – September 30, 2015 Index Years: July 1, 2010 – June 30, 2011 July 1, 2011 – June 30, 2012 July 1, 2012 – June 30, 2013 Penalty in FY 2015: Up to 3% of Medicare payments Now, About COPD . . . . Definition: A progressive, inflammatory chronic disease characterized by increasing airflow obstruction coupled with destruction of pulmonary gas exchange areas. There are clinically relevant extra-pulmonary effects secondary to systemic inflammation Prevalence is increasing; 3rd Leading cause of death Airflow obstruction/alveolar destruction largely irreversible Primary cause: Long-term exposure to noxious inhalants A largely preventable disease Fourth leading cause of recidivism Risk Factors for COPD Genes Infections Socio-economic status Aging Populations © 2013 Global Initiative for Chronic Obstructive Lung Disease COPD is a Multisystem Disease Anxiety, Depression, Addiction Lung Cancer Pulmonary Hypertension Anemia Cardiovascular Disease Peripheral Muscle Wasting & Dysfunction Osteoporosis Diabetes Metabolic Syndrome Peptic Ulcers GI Complications Cachexia Adapted from Kao C, Hanania NA. Atlas of COPD. 2008. COPD Comorbidities COPD Opportunities for Improvement Currently, care outcomes less than optimal Growing concern over high recidivism rate Unplanned re-admissions are costly 30 day re-admits largely preventable COPD evidence-based care guidelines exist For both in-patient (exacerbation) and out-patient (Sx control) Use of evidence-based care guidelines is low Under-treatment of COPD Record review: 553 pts. discharged with Dx of COPD Darmella W, et al. Respir Care; October 2006 Only 31% had confirmatory spirometry We must raise awareness of the need to confirm the diagnosis of COPD and it’s severity with spirometry Record review: 169 pts. with 1,664 care events Mularski RW, et al. Chest; December 2006 Subjects received 55% of recommended care; Only 30% with base-line hypoxemia received LTOT The deficits and variability in processes of care for patients with obstructive lung disease presents ample opportunity for improvement Inpatient COPD Care: The Evidence McCrory DC, et al. Chest; 2001 EFFICACY EVIDENCE EXISTS EFFICACY EVIDENCE LACKING Chest radiography/ABGs Sputum analysis Oxygen therapy Acute spirometry Bronchodilator therapy Mucolytic agents Systemic steroids Chest physiotherapy Antibiotics Methylxanthine bronchodilators Ventilatory support (as required) Leukotrine modifiers; Mast cell stablizers Level 1-2 evidence of efficacy = Recommended care Insufficient efficacy evidence = Non-recommended care Non-recommended care = Unnecessary care Under-treatment of COPD Record review: 69,820 records from 360 hospitals Lindenauer PK, et al. Ann Intern Med; June 2006 66% received all of recommended care; 45% received at least one non-recommended care; Only 30% received Ideal Care We identified widespread opportunities to improve quality of care and to reduce costs by addressing problems of underuse, overuse and misuse of resources, and by reducing variation in practice Claims data review: 42,565 commercial, 8,507 Medicare Make B, et al. Int J Chron Obstruct Pulmon Dis; January 2012 No pharmacotherapy – 60% commercial, 70% Medicare No smoking cessation – 82% commercial, 90% Medicare No influenza vaccination – 83% commercial, 76% Medicare This study highlights a high degree of undertreatment of COPD, with most patients receiving no maintenance pharmacotherapy or influenza vaccination Under-treatment of COPD: Summary COPD - an expensive, chronic condition Incidence is increasing Financial liability is escalating Diagnostic spirometry is woefully under-used Use of evidence-based treatment guidelines is low Failure to control symptoms a precursor to exacerbations COPD hospital re-admissions are largely preventable Chronic disease management strategies a necessity GOLD Guidelines Pre-2013 IV: Very Severe III: Severe II: Moderate I: Mild • FEV1/FVC < 0.70 • FEV1 ≥ 80% predicted • FEV1/FVC < 0.70 • 50% ≤ FEV1 < 80% predicted • FEV1/FVC < 0.70 • 30% ≤ FEV1 < 50% predicted • FEV1/FVC < 0.70 • FEV1 < 30% predicted or FEV1 < 50% predicted plus chronic respiratory failure Active reduction of risk factor(s); smoking cessation, flu vaccination Add short-acting bronchodilator (as needed) Add regular treatment with long-acting bronchodilators; Begin Pulmonary Rehabilitation Add inhaled glucocorticosteroids if repeated acute exacerbations Add LTOT for chronic hypoxemia. Consider surgical options Combined Assessment of COPD GOLD Guidelines (2013) 4 (C) (D) ≥2 3 Risk Risk GOLD Classification of Airflow Limitation Exacerbation history 2 (A) (B) 1 1 0 mMRC 0-1 (or) CAT < 10 mMRC > 2 (or) CAT > 10 Symptoms (mMRC or CAT score) Left (or) Right: Up (or) Down > 2 exacerbations 0-1 exacerbations Fewer Symptoms More Symptoms Assessment of Symptoms GOLD Guidelines (2013) Modified British Medical Research Council (mMRC) Dyspnea Questionnaire: A 5-item measure of perceived dyspnea Self-report on grade 0 – 5 (or) COPD Assessment Test (CAT): An 8-item measure of health status impairment in COPD Self-report on scale 0 – 5 Both have been validated and relate well to other measures of health status and predict future mortality risk. Modified MRC (mMRC) Questionnaire GOLD Guidelines (2013) COPD Assessment Test (CAT) GOLD Guidelines (2013) COPD Assessment Test (CAT) GOLD Guidelines (2013) Combined Assessment of COPD Global Strategy for Diagnosis, Management and Prevention of COPD Risk (C) (D) 3 4 30-50% <30% Pre-2013 GOLD Classification of Airflow Limitation ≥2 Risk (A) (B) 1 1 2 0 ≥ 80% 50-80% mMRC 0-1 (or) CAT < 10 mMRC > 2 (or) CAT > 10 Symptoms (mMRC or CAT score) Exacerbation history Combined Assessment of COPD GOLD Guidelines (2013) When assessing risk, choose the highest risk according to GOLD grade or exacerbation history Patient Characteristics Spirometric Classification Exacerbations per year mMRC CAT A Less Symptoms Low Risk GOLD 1-2 0-1 0-1 < 10 B More Symptoms Low Risk GOLD 1-2 0-1 ≥2 ≥ 10 C Less Symptoms High Risk GOLD 3-4 ≥2 0-1 < 10 D More Symptoms High Risk GOLD 3-4 ≥2 ≥2 ≥ 10 COPD Maintenance Treatment by Airflow Limitation/Risk GOLD Guidelines (2013) FEV1 % PREDICTED EXACERBATION GRADE TREATMENT CONSIDERATIONS (AIRFLOW LIMITATION) (RISK) ≥ 80% LOW Smoking cessation; Vaccinations; SABA prn 50 – 80% MEDIUM Add to above: Nebulized LABA-LAMA daily; Pulm Rehab; Exacerbation action plan 30 – 50% HIGH Add to above: ICS for exacerbation prone; Referral to pulmonologist ≤ 30% VERY HIGH Add to above: long-term oxygen therapy; Consider surgical options Inpatient COPD Care: The Evidence McCrory DC, et al. Chest; 2001 EFFICACY EVIDENCE EXISTS EFFICACY EVIDENCE LACKING Chest radiography/ABGs Sputum analysis Oxygen therapy Acute spirometry Bronchodilator therapy Mucolytic agents Systemic steroids Chest physiotherapy Antibiotics Methylxanthine bronchodilators Ventilatory support (as required) Leukotrine modifiers; Mast cell stablizers Acute Spirometry with COPD Exacerbation Isn’t spirometry needed to Confirm Dx and Grade Airflow Limitation? Acute spirometry Hospitalized patients not ready for full PFT studies Unable to exert maximal effort; Repeat maneuvers Pre-post bronchodilator response of limited value Make appointment for 4-6 weeks post recovery What about peak inspiratory flow? Not a demanding test but insightful Ability to use a DPI Generate ≥ 40 L/min PIF Secretion Retention with COPD Exacerbation Can Contribute to Airflow Obstruction; WOB Chest physiotherapy An airway clearance technique (ACT) Secretion retention, ineffective cough problematic Trendelenburg position contraindicated in COPD Proven alternate ACT techniques in use for CF ACBT, AD, HFCWO, IPV, OPEP Which to consider for COPD? OPEP Rx a viable regimen Inexpensive, non-invasive Alone or in combo with SVN Medication Nebulizers Not all jet-nebulizers are created equal! Respirable Dose 10% Respirable Dose 15% Respirable Dose 30% Higher respirable dose = Quicker onset of action! Higher respirable dose = Shorter treatment times! Quicker onset/less time = Better RT deployment! Dynamic Hyperinflation Dynamic hyperinflation Breath Actuated Nebulizer in COPD Haynes J. Respir Care; Sept 2012 Prospective, randomized controlled trial Objective: compare bronchodilator response w/ BAN to standard SVN Patients admitted w/ COPD exacerbation N = 40 of 46; Similar baseline characteristics Dyspnea secondary to dynamic hyperinflation Medication regimen 2.5 mg albuterol/0.5 mg ipratropium (3 mL) Q4H 2.5 albuterol Q2H prn Common adverse effects monitored during/after each Rx Data collected 2 hrs post 6th scheduled Rx (collector blinded) Inspiratory capacity; dyspnea; RR Breath Actuated Nebulizer in COPD Haynes J. Respir Care; Sept 2012 Findings: Both groups received same # Rxs (6.25; 6.20) IC higher in BAN v. SVN (1.83 L v. 1.42 L; P .03) Change in IC greater BAN v. SVN RR lower in BAN v. SVN (19/min v. 22/min; P = .03) No difference in BORG or LOS Breath Actuated Nebulizer in COPD Haynes J. Respir Care; Sept 2012 Conclusions: In this cohort of patients with ECOPD, the AeroEclipse II BAN was more effective in reducing lung hyperinflation and respiratory rate than traditional SVN. It may be that the BAN group simply received more medication because of the breath activated mode…Aerosols with MMAD of 3.0 μm produce the highest physiological response in terms of FEV1 and airway conductance. Role of Nebulized Therapy in COPD Dhand R, et al. COPD; Feb 2012 RECOMMENDATION: Many patients, especially elderly patients with COPD, are unable to use their pMDIs and DPIs in an optimal manner. For such patients, nebulizers should be employed on a domiciliary basis. . . Nebulizers are more forgiving to poor inhalation technique, especially poor coordination with pMDIs and the requirement to generate adequate peak inspiratory flows with DPIs. Nebulized Therapy at Home Ease of use; simple technique Addresses inconvenience issue Effective and reliable drug delivery Use not limited by disease severity or mental acuity Device & medications covered under Medicare Part B Managing Stable COPD Goals of Therapy Relieve airflow obstruction Improve exercise tolerance Reduce symptoms Improve health status Relieve airflow obstruction Improve exercise tolerance Reduce risk Improve health status Reduced symptoms + Reduced risk = Successful disease management Improving COPD Care Outcomes Summary A new COPD care pathway essential COPD pts. will impact hospital’s revenue Pt. volume will vary by institution 1-2/month up to 6-8/month Allocate resources accordingly Re-design current workload Advocate evidence-base care Start small; Expand accordingly Appoint, anoint, elect one departmental COPD Guru Let pt. volume drive program development Determine risk grade per 2013 GOLD Guidelines Use CAT (or) mMRC Ensure proper controller medications prescribed Appointment for follow-up MD appointment 5-7 days AARC Resources Domain of Likely COPD Performance Measures Timely and Effective Care Performance measures tied to readmission penalties Already required under Physician Quality Reporting System (PQRS) Documented evidence in medical record of: Smoking cessation (discussed at every visit) Spirometry (within past 2-3 yrs.) Bronchodilator therapy (esp. controller medications) Immunizations (pneumococcal, influenza) White Memorial Medical Center January 31, 2014 Los Angeles CA COPD: Managing the Disease Not The Symptoms Patrick J. Dunne, MEd, RRT, FAARC HealthCare Productions, Inc. Fullerton, CA 92838 pjdunne@sbcglobal.net