TOPCAT ACCP Cardiology PRN Journal Club Presentation
advertisement

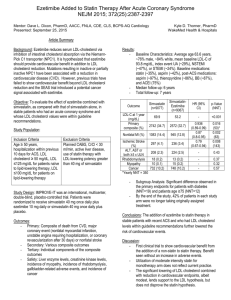
ACCP Cardiology PRN Journal Club 1 Announcements • Thank you attending the ACCP Cardiology PRN Journal Club – Thank you if you attended before or have been attending • I have created a PB Works Site that will house our recorded calls, handouts, and Summary/Q&A documents. The link is https://accpcardsprnjournalclub.pbworks.com/ • If there are any suggestions, please let us know. Ezetimibe Added to Statin Therapy after Acute Coronary Syndrome (IMPROVE-IT) Kyle Thorner, Pharm.D. PGY2 Cardiology Resident WakeMed Health & Hospitals Raleigh, NC Disclosure Statement Kyle Thorner has no conflicts of interest to disclose. Background • Ezetimibe inhibits the absorption of LDL-C from the intestinal lumen via inhibition of Niemann-Pick C1 (NPC1L1). • Mutations in NPC1L1 reduce plasma LDL-C and have been associated with reduced risk of CHD NEJM 2014;371:2072-82 Science 2004;303:(5661):1149 Background • Prior clinical trial experience with ezetimibe Trial Treatment Primary Outcome Result ENHANCE Simvastatin/Ezetimibe 80/10 mg vs Simvastatin 80 mg SEAS Simvastatin/Ezetimibe 40/10 mg vs Placebo Composite of major cardiovascular events 35.5% vs 38.2%; HR 0.96 (0.83-1.12), p=0.59* SHARP Simvastatin/Ezetimibe 20/10 mg vs Placebo First major atherosclerotic event 13.4% vs 11.3%; RR 0.83 (0.74-0.94), p=0.0021 Mean Δ carotid-artery 0.0058 mm vs intima-media thickness 0.0111 mm, p=0.28 *Incidence of cancer: 105 vs 70, p=0.01 NEJM 2008;358(14):1431-1443 NEJM 2008;359:1343-1356 Lancet 2011;377:2181-2192 IMPROVE-IT Study Objective To evaluate the effect of ezetimibe combined with simvastatin, as compared with that of simvastatin alone, in stable patients who had had an acute coronary syndrome and whose LDL cholesterol values were within guideline recommendations. NEJM 2015;372(25):2387-2397 Study Population Inclusion Criteria Exclusion Criteria - Age ≥ 50 years - Hospitalization within previous 10 days for ACS - LDL cholesterol ≥ 50 mg/dL - LDL ≤125 mg/dL for patients naïve to lipid-lowering therapy - LDL ≤100 mg/dL for patients on lipid-lowering therapy - Planned CABG CrCl < 30 ml/min Active liver disease Use of statin therapy with LDL-lowering potency greater than 40 mg of simvastatin NEJM 2015;372(25):2387-2397 Study Design • International, multi-center, double-blind, placebo-controlled, randomized trial Simvastatin 40* mg + Placebo daily (n=9077) 18,144 patients Simvastatin 40* mg + Ezetimibe 10mg daily *Simvastatin could be uptitrated to 80 mg if LDL-C >79 mg/dL, addendum made after FDA advisory in 2011 (n=9067) • Follow-Up – Visits: At 30 days, 4 months and every 4 months thereafter – Blood Samples: at randomization, at 1, 4, 8, and 12 months, and then yearly NEJM 2015;372(25):2387-2397 Study Endpoints Primary Endpoint • Composite of death from CVD, major coronary event, or nonfatal stroke Safety Endpoints • • • • • Liver enzyme levels CK levels Episodes of myopathy or rhabdomyolysis Gallbladder-related adverse events Cancer NEJM 2015;372(25):2387-2397 Statistics & Enrollment Statistics Enrollment • Estimated that 5,250 events required for 90% power to detect a 9.375% lower relative risk for the primary end point with simvastatinezetimibe vs simvastatin • Intention-to-treat analysis • • • • N = 18,144 Median follow-up = 6 years Total follow-up = 7 years Regions: – – – – – North America (N=6,973) Western Europe (N=7,274) Eastern Europe (N=1,416) Asia Pacific (N=896) South America (N=1,585) NEJM 2015;372(25):2387-2397 Baseline Characteristics Simvastatin Simvastatin-Ezetimibe (n=9077) (n=9067) Mean Age, yrs 63.6 63.6 Male Sex, % 75.9 75.5 84 83.6 93.8 93.8 28.7 / 46.9 / 24.4 28.5 / 47.5 / 24 PCI, % 69.7 70.5 Medications prior to index ACS Statin, % Aspirin, % 34.3 42.5 35.6 41.9 Medications post ACS Aspirin, % Thienopyridine, % Beta Blocker, % ACE-Inhibitor or ARB, % 96.9 86.1 86.8 75.8 97.1 86.6 87.3 75.3 Variable White Race, % Mean LDL, mg/dL Index Event STEMI / NSTEMI / UA, % NEJM 2015;372(25):2387-2397 Results 1 Yr Mean LDL-C TC TG HDL hsCRP Simva 69.9 145.1 137.1 48.1 3.8 EZ/Simva 53.2 125.8 120.4 48.7 3.3 Δ in mg/dL -16.7 -19.3 -16.7 +0.6 -0.5 Simva EZ/Simva NEJM 2015;372(25):2387-2397 Results Total NNT= 50 Yearly NNT= 350 NEJM 2015;372(25):2387-2397 Results Tertiary Outcomes Simvastatin (n=9077) SimvastatinEzetimibe (n=9067) HR (95% CI) p-Value (NNT) Nonfatal MI 1083 (14.4%) 945 (12.8%) 0.87 (0.80.95) 0.002 (63) Ischemic Stroke 297 (4.1%) 236 (3.4%) 0.79 (0.67-0.94) 0.008 (143) Simvastatin SimvastatinEzetimibe Safety Outcomes (n=9077) p-Value (n=9067) ALT, AST, or both ≥3 ULN 208 (2.3%) 224 (2.5%) 0.43 Rhabdomyolysis 18 (0.2%) 13 (0.1%) 0.37 Myopathy 10 (0.1%) 15 (0.2%) 0.32 Cancer 732 (10.2%) 748 (10.2%) 0.57 NEJM 2015;372(25):2387-2397 Author’s Conclusion The addition of ezetimibe to statin therapy in stable patients with recent ACS and who had LDL cholesterol levels within guideline recommendations further lowered the risk of cardiovascular events. NEJM 2015;372(25):2387-2397 Study Critique Strengths Weaknesses • Large sample size with long duration of follow-up • Low incidence of adverse effects with simvastatin/ezetimibe • Age subgroup analysis comparable to modern guidelines • Intensity of statin therapy does not reflect current guideline recommendations • Amount of study drug discontinuation • Modest benefit and primarily in nonfatal endpoints Impact on Clinical Practice • First clinical trial to show benefit on composite CV outcome when adding non-statin therapy to a statin. Trial Treatment Primary Outcome Result The ACCORD Study Group Simvastatin + Fenofibrate/Placebo Nonfatal MI/Nonfatal stroke/CV death HR 0.92 (0.79-1.08) P=0.32 AIM-HIGH Simvastatin +/- Ezetimibe + Niacin/Placebo Nonfatal MI/Ischemic Stroke/ACS hospitalization/ Revascularization/CV death Stopped early due to lack of efficacy HPS2-THRIVE Simvastatin +/- Ezetimibe + Niacin/Placebo Time to first major vascular event RR 0.96 (0.90-1.03) P=0.29 The dalOUTOMES Investigators Dalcetrapib vs placebo in addition to standard of care (98% statins) CHD death, nonfatal MI, ischemic stroke, unstable angina, cardiac arrest HR 1.04, (0.93-1.16) P=0.52 NEJM 2010;362(17):1563-1574, NEJM 2011;365(24):2255-2267 NEJM 2014;371(3):203-212, NEJM 2012;367(22):2089-2099 Impact on Clinical Practice • May support the LDL hypothesis, but does not disprove the statin hypothesis. – Reconsider LDL-C targets in future guidelines – Future study: High intensity statin compared to ezetimibe/simvastatin with equal LDL lowering • Could apply results to justify addition of ezetimibe to moderate intensity statin therapy – Patients intolerant of high-intensity statins – Elderly patients – Diabetic patients Acknowledgements • Dave L. Dixon, Pharm.D., AACC, FNLA, CDE, CLS, BCPSAQ Cardiology – Virginia Commonwealth University School of Pharmacy • Erin (Allender) Ledford, Pharm.D., BCPS-AQ Cardiology – WakeMed Health & Hospitals • Janna Beavers, Pharm.D., BCPS – WakeMed Health & Hospitals • Craig Beavers, Pharm.D., AACC, BCPS-AQ Cardiology – TriStar Centennial Medical Center Questions? Thank you for attending! • If you would like to have your resident present, would like to be a mentor, or have questions or comments please e-mail the journal club at accpcardsprnjournalclub@gmail.com or craig.beaverspharmd@gmail.com • Join us next month when we hear the BRIDGE Trial from Leah Sabato, PharmD PGY-2 Cardiology from Vanderbilt with Michael Gulseth , PharmD as mentor 22