Dietetics
advertisement
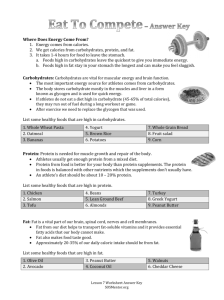
Dietetics I ABU NURUDEEN DEFINITION • Dietetics - The branch of therapeutics concerned with the practical application of diet in relation to health and disease. • Dietetics - the science of applying nutritional principles to the planning and preparation of foods and regulation of the diet in relation to both health and disease. Dietitians in practice • Clinical dietitians • Clinical dietitians work in hospitals, nursing care facilities and other health care facilities to provide nutrition therapy to patients with a variety of health conditions, and provide dietary consultations to patients and their families. • They confer with other health care professionals to review patients' medical charts and develop individual plans to meet nutritional requirements. Some clinical dietitians will also create or deliver outpatient or public education programs in health and nutrition. • Community dietitians • Community dietitians work with wellness programs, public health agencies, home care agencies, and health maintenance organizations. • These dietitians apply and distribute knowledge about food and nutrition to individuals and groups of specific categories, life-styles and geographic areas in order to promote health. • Foodservice dietitians • Foodservice dietitians or managers are responsible for large-scale food planning and service. They coordinate, assess and plan foodservice processes in health care facilities, school food service programs, prisons, restaurants, and company cafeterias. • These dietitians may perform audits of their departments to ensure quality control and food safety standards, and launch new menus and various programs within their institution to meet health and nutritional requirements. • Gerontological /geriatric dietitians • Gerontological dietitians are specialist in nutrition and aging. • They work in nursing homes, communitybased aged care agencies, government agencies in aging policy, and in higher education in the field of gerontology (the study of aging). • Neonatal dietitians • Neonatal dietitians provide individualized medical nutrition therapy for critically ill premature newborns. They are considered a part of the Neonatal Intensive Care Unit's medical team. • The neonatal dietitian performs clinical assessment of patients, designs nutrition protocols and quality improvement initiatives with the medical team, develops enteral and parenteral regimens. • They also help to establish and promote lactation/breastfeeding guidelines and often oversees the management of infection prevention in the handling, storage, and delivery of nutritional products. • Pediatric dietitians • Pediatric dietitians provide nutrition and health advice for infants, children, and adolescents. • They focus on early nutritional needs, and often work closely with doctors, school health services, clinics, hospitals and government agencies, in developing and implementing treatment plans for children with eating disorders, food allergies, or any condition where a child’s diet factors into the equation, such as childhood obesity. • Research dietitians • Research dietitians are involved with dieteticsrelated research conducted in hospitals, universities, government agencies, food and beverage companies, and the pharmaceutical industry. • They may conduct research in clinical aspects of nutrition, for example, the effects of diet on cancer treatment. • Administrative dietitians • Administrative or management dietitians oversee and direct all aspects of food policy and largescale meal service operations in hospitals, government agencies, company cafeterias, prisons, and schools. • They recruit, train and supervise employees of dietetics departments including dietitians and other personnel. • Consultant dietitians • Consultant dietitian is a term sometimes used to describe dietitians who work under contract with health care facilities or in private practice. • Consultant dietitians are contracted independently to provide nutrition services and educational programs to individuals and health care facilities as well as sports teams, fitness clubs, supermarkets, and other health and nutrition-related businesses. • The 6 Basic Principles of Diet Planning • Ask most people what the word "diet" means and they describe short-term weight loss goals and countless food restrictions. However, the term "diet" simply refers to what we eat. • A good diet promotes positive change and helps you incorporate sensible eating into your daily lifestyle. • The six principles of diet planning include; Adequacy Nutrient density Moderation Variety Balance Calorie control Adequacy • An adequate diet provides the human body with enough energy and nutrients for optimal growth, maintenance and repair of tissue, cells and organs. • Water, carbohydrates, fats, proteins, vitamins and some minerals comprise the six nutrient classes relied upon for performance of essential functions and activities. • These nutrients must be replaced through diet to keep the body working efficiently. • An adequate diet includes foods containing proper amounts of these nutrients to prevent deficiencies, anemia, headaches, fatigue and general weakness. Balance • A balance diet provides foods of a number of types in proportion to each other such that foods rich in some nutrients do not crowd out of the foods that are rich in other nutrients. • Balance in the diet helps to achieve adequacy. • The essential minerals calcium and iron, taken together illustrate the importance of dietary balance. Meat , fish and poultry are rich in iron but poor in calcium. • Similarly, milk and milk products are rich in calcium but poor in iron. • In fact, milk(except breast milk) and milk products are so low in iron that overuse of these foods can actually lead to iron-deficiency anemia by displacing iron-rich foods from the diet. • The art of balancing the diet involves using enough of each type of food. • Consuming the proper amount of servings from each food group ensures a wellproportioned diet. Calorie Control • Once you know what to eat, the next factor is how much. It is possible to eat healthy foods and still overindulge. • Clearly, the task of designing an adequate, balanced diet requires some thought and skillful planning. Even more thought and skill are required to create an adequate and, balance diet without overeating. • Therefore, a reasonable calorie allowance must be established. The amount of energy the body receives from incoming food needs to match the amount of energy needed for the body to sustain its biological and physiological activities. • In other words, input needs to match output. An imbalance leads to weight loss or gain. Nutrient density • Eating well without overeating is often challenging. • Nutrient density is a measure of the nutrients a food provides relative to the energy it provides. The more nutrients and the fewer kcalories, the higher the nutrient density. Nutrient density promotes adequacy and kcalorie control • You must select foods that pack the most nutrients into the least amount of calories. • For example, 1 oz. of cheese and 1 cup of fat-free milk contain the same amount of calcium. • While both foods are adequate sources of calcium, the milk is more calcium-dense than the cheese because you get the same amount of calcium with one-half the calories and no fat. • Designing a nutritionally sound diet requires proper "budgeting" of calories and nutrients so that you eat less while supporting good health. Moderation • Socrates once said "Everything in moderation; nothing in excess." Though over 2,500 years old, this adage still holds true. • Those who place severe restrictions on what they can or cannot eat often find it difficult to stick to a pattern of sensible eating. • Depriving yourself of foods rich in fat and sugar is not necessary. • When eaten on occasion, these treats are not detrimental to your health and often provide enough enjoyment to keep one motivated to continue healthy eating practices. Variety • It's possible for a diet to have all the aforementioned characteristics, but still lack variety if the person eats the same foods day after day. People should vary their choices within each class of foods from day to day for three reasons. • First, different foods in the same group contain arrays of nutrients. Among the fruits for example, strawberries are especially rich in vitamin C while bananas are rich in potassium. • Second, no food is guaranteed entirely free of constituents that in excess, could be harmful. • Third, as the adage goes, variety is the spice of life. Even if a person eats beans frequently, the person can choose red beans today, garbanzo beans tomorrow, and baked beans on the weekend. • Good nutrition does not have to be boring. Diet planning guides • To plan a Diet that achieves all of the dietary ideals just outlined, a planner needs not only knowledge but tools. • Four of the most used tools for diet planning are; 1. Food group plans 2. Food exchange lists 3. Food guide pyramid 4. WHO recommendations Food group plans • This is a food planning tool that sorts foods of similar origin and nutrient content into groups and then specify that people should eat certain numbers of serving from each group. • Of the diet –planning principles introduced earlier, food group plans help the diet planner best to achieve dietary adequacy, balance and variety • • • • Four food group plan 4 servings of vegetables and fruits 4 servings of bread and cereals 2 servings of milk and milk products 2 servings of meat and meat products Daily food guide • The daily food guide differs from the four food group plan by splitting vegetables from fruits, so that there are five groups of foods. • The numbers of serving suggested are also more generous. 6--11 servings of breads and cereals 3– 5 servings of vegetables 2--4 servings of fruits 2– 3 servings of meats and meat products 2 servings of milk and milk products Food Exchange List • This is a diet planning tool that organizes foods by their nutrient and energy contents. Foods on any list can be used interchangeably. • Exchange list provide additional help in achieving kcalorie control and moderation. • Originally developed for people with diabetes, exchange system have proved so useful that they are now in general use for diet planning. • Unlike the food group plan, which sort foods primarily by their protein, vitamin, and mineral, the exchange sorts foods by their proportions of carbohydrates, fat and protein. • Portion sizes are strictly defined so that the amount of energy provided by any food item is the same as that from any other item within a given list. • All of the food portion in a given list provide approximately the same amount of energy nutrients(carbohydrates, fat and protein) and the same number of calories. • Any food on the list can be exchanged or traded for any other food on that same list without affecting a plans balance or total calories. • The six exchange list are as follows: Starch/bread- 1 slice bread(80 calories) Meat-1ounce lean beef(55 calories) Vegetables-1/2 cup cooked carrots(25 calories) Fruits-1/2 banana(60 calories) Milk- 1 cup nonfat milk(90 calories) Fat- 1 teaspoon butter(45 calories) Starch/bread exchange • 1 slide of bread is like • ¾ c ready-to-eat cereals • ½ c cooked pasta • 1/3 c cooked rice • 1/3 c cooked beans • ½ corn • 1 small( 3oz) potato (1 bread = 15g carbohydrate, 3g protein, trace of fat, and 80 kcal) Food Guide Pyramid • The most recent food guide designed to provide sound nutritional advice for daily food selection is the food guide pyramid. • It is designed to provide visual image of the variety of foods that people should eat, the proportion of calories that should come from each of the groups, and the use of moderation in consumption of fats, oils and sweets. • The food guide pyramid is result of years of deliberation by renowned nutrition scientists. • Although there are six categories of foods in the pyramid, • Nutritionists do not regard fats, oil and sweets as an actual food group. • The base of the pyramid, which should constitute the majority of daily calories, is represented by the bread, cereal, rice, and pasta group(6-11 serving) and the fruit group(2-4 serving). These three foods group are derived from grains and plants. • Fewer servings are recommended from the milk, yogurt, and cheese group(2-3 servings) and the meat, poultry, fish, dry beans, eggs and nuts group derived primarily from animals. • Fats, oils and sweets(not classified as a group) should be used sparingly. • Typical serving sizes are defined for each food item in each group. eg, a serving of milk is 1 cup while a serving of cooked or chopped vegetable is ½ a cup. WHO recommendation • According to WHO recommendation on daily food selection; • 60 % of daily calorie should come carbohydrates. • 30% from fat. • 10% from protein. HEALTHY DIET • In the past most morbidity and mortality in the developed nations were caused by nutrientdeficiency diseases and infectious diseases, • But advances in nutritional and medical sciences have almost eliminated most of the adverse health consequences of associated with these disease. • Today, most morbidity and mortality are associated with various chronic diseases(e.g., coronary heart disease, stroke, cancer, diabetes, obesity), • And most dietary guidelines for healthful nutrition are targeted to prevent these chronic diseases. • An unhealthy diet is a major risk factor for a number of chronic diseases including: High blood pressure, Diabetes, Abnormal blood lipids, Overweight/obesity, Cardiovascular diseases, and Cancer. • The WHO estimates that 2.7 million deaths are attributable to a diet low in fruit and vegetable every year. • Globally, it is estimated to cause about 19% of gastrointestinal cancer, 31% of ischaemic heart disease, and 11% of strokes, thus making it one of the leading preventable causes of death worldwide. • The essence of healthy diet is to promote good health and significantly reduce the risk of developing chronic diseases. • The following dozen guidelines represent what is called a healthy diet. Healthy Diet 1. Balance the food you eat with physical activity to maintain or improve your weight. 2. Eat a nutritional adequate diet consisting of a wide variety of foods. 3. Choose a diet low in fat, saturated fat and cholesterol. 4. Choose a diet with plenty of whole grain products, legumes, fruits and vegetables, which are rich in complex carbohydrates and fiber. 5. Choose a diet moderate in sugars 6. Choose a diet moderate in salts and sodium 7. If you drink alcoholic beverages, do so in moderation. Pregnant women should not drink any alcohol. 8. Maintain protein intake at a moderate, yet adequate level, obtaining much of your daily protein from plant sources. 9. Choose a diet adequate in calcium and iron 10. Children and others susceptible to tooth decay should obtain adequate fluoride. 11. In general avoid taking dietary supplements in excess of the RDA in any one day. 12. Eat fewer foods with questionable additives 1. Balance the food you eat with physical activity to maintain or improve your weight • Preventing obesity helps to reduce the risk of numerous chronic diseases such as heart disease and cancer. • To avoid becoming overweight, you should consume only as many calories as you expend daily. • An aerobic exercise program and adherence to the concept of nutrient density, could serve as the basis for sound weight-control program. 2. Eat a nutritionally adequate diet consisting of a wide variety of foods • Eating a wide variety of natural foods from within and among the six food groups or Food Guide Pyramid or the Food Exchange List will assure you of obtaining a balanced and adequate intake of all essential nutrients. • Stress foods that are high in the key nutrients. 3. Choose a diet low in total fat, saturated fats, and cholesterol • Currently, fat comprises almost 35 percent of total daily calories. • The recommended dietary goal is to obtain less than 30 percent of calories from fat. • In addition, the amount of saturated fat in the diet should be 10 percent or less, and cholesterol intake should be limited to 300 milligrams or less per day. • However, it should be noted that some healthful diet plans recommend lower values, such as 10-20 percent total fat, less than 7 percent saturated fat, and less than 200 milligrams of cholesterol. • The following practical suggestions will help people meet the recommended dietary goal. Eat less meat with a high –fat content. Avoid hot dogs, luncheon meats, sausage, and bacon. Trim of excess fat before cooking. Eat only lean red meat and more white meat, such as turkey and chicken, which have less fat. Remove the skin from poultry. Eat more fish. Many fish, such as sardines, salmon, tuna, and mackerel, are rich in omega-3 fatty acids. White fish, such as flounder, is very low in fat Calories. Eat no more than 6 ounce of animal meat per day. Eat only two to three eggs per week. One egg yolk contain about 220-250 milligrams of cholesterol, close to the limit of 300 milligrams per a day. Egg whites have no cholesterol and are an excellent source of high-quality protein. Eat fewer diary products that are high in fat. Switch from whole milk to skim or nonfat milk, such as yogurt and cottage cheese. If you like cheese, switch from hard cheese to soft cheeses although most cheeses, except low-fat cottage cheese are still high in fat and calories. Some fat-free cheeses are now available. Eat less butter, which is high in saturated fats, by substituting soft margarine made or polyunsaturated, such as corn oil Avoid margarine made from hydrogenated or partially hydrogenated oils, which basically are metabolized like saturated fat. Eat margarine sparingly. Some fat-free margarines are also available. Eat fewer commercially prepared baked goods made with eggs and saturated or hydrogenated fats. Limit your consumption of fast foods. Although fast-food chains generally serve grade A foods, many of their products are high in fat. The average fast-food sandwich contains approximately 50 percent of its Calories in fat. Some fast-food restaurant do serve nutrient-dense foods. Wise choices, such as baked fish grilled skinless chicken, lean meat, baked potatoes and salads can provide healthy nutrition. Use food labels to help you select foods low in total fat, saturated fat and fat Calories, all of which are listed on the food label for most products. Broil, bake, grill, boil or microwave your foods. Limit frying. If you must use in your cooking, try to use monounsaturated oils such as olive or peanut oil. • In general, decrease your intake of cholesterol, total fat, and saturated fat by substituting monounsaturated, polyunsaturated and omega-3 fatty acids for saturated or hydrogenated fats 4. Choose a diet with plenty of whole-grains products, fruits and vegetables, foods which are rich in fiber & complex carbohydrates • In general, about 60 percent or more of your daily Calories should come from carbohydrates, about 50 percent from complex carbohydrates, and the other 10 percent from simple, naturally occurring carbohydrates. • To accomplish this, you need to eat more wholegrain products (breads and cereals), legumes (beans and peas), and vegetables and fruits. • Stress vegetables and fruits high in betacarotene and vitamin C ( the antioxidant vitamins) such as carrots and sweet potatoes. • Deep yellow and orange fruits and vegetables as well as dark-green leafy vegetables are usually good sources of these vitamins. • Also increase intake of cruciferous vegetables, those from the cabbage family. • These fruits and vegetables contain various phytochemicals which protect people against several forms of cancers. • Another benefit of complex carbohydrates is their high fiber content. Whole-grain products and numerous vegetables are excellent sources of water insoluble fiber. • The high fiber content of these foods is believed to be important in the prevention of diseases such as colorectal cancer and coronary heart disease. • Food labels list the total carbohydrates and the amount of dietary fiber per serving. 5. Choose a diet moderate in sugars • The recommended dietary goal is to reduce consumption of refined sugar from the current level of 24 percent of daily Calories to 10 percent or less. • Excessive consumption of refined sugar has been associated with high blood triglyceride level. Sticky sugars are a major contributing factor to dental cavities. • Sugars also significantly increase the caloric content of foods without an increase in nutritional value, so they may contribute to body weight problems. • To meet this goal you should reduce your intake of common table sugar and products high in refined sugar. • Sugar is one of the major additives to processed foods, so check the labels. If sugar is listed first, it is the main ingredient. • Use naturally occurring sugar to satisfy your sweet tooth. Most fruits have high sugar content, but also contain vitamins, minerals, and fiber as well. • Also look for terms such as corn syrup, dextrose, fructose, and malt sugar, which are also primarily refined sugars. 6. Choose a diet moderate in salt and sodium • Restrict sodium intake to less than 2,400 mg daily, which is the equivalent of 6,000 milligram, or 6 grams, of table salt. • This lower amount will provide sufficient sodium for normal physiological functioning. • Sodium is found naturally in a wide variety of foods, so it is not difficult to get an adequate supply. • The following key suggestions may help people reduce the sodium content in their diets Get rid of your salt shaker. One teaspoon of salt is 2,000mg of sodium; the average well-salt meal contains about 3,000 to 4,000mg. Put less salt on your food both in your cooking pot and on your table. Reduce the consumption of obviously high-salt foods such as most “koobi” and potato chips, pickles and other such snacks Check food labels for sodium content, if salt or sodium is one of the ingredients listed, you have a high-sodium food. Salt is a major additive in many processed foods, often disguised by terms such as monosodium glutamate and others. Food labels list the sodium content per serving. Use fresh herbs, spices that do not contain sodium, or little salt as seasoning alternatives. 7 If you drink alcoholic beverages, do so in moderation • The current available scientific evidence does not suggest that light to moderate daily alcohol consumption will cause any health problems to the healthy, nonpregnant adult. • However, excessive alcohol consumption is one of the most serious health problems in our society today, and even small amounts may pose health problems to some individuals. • Light to moderate drinking is based upon a limit one drink for nonpregnant woman and two drinks for a man. • A drink is defined as a dose of any alcoholic beverage that delivers ½ oz of pure ethanol; • one 12-oz bottle of beer, • one 4-oz glass of wine, or • 1.5 ounces of 80-proof distilled spirits. 8 Maintain protein intake at a moderate, yet adequate level, obtaining much of your daily protein from plant sources. 8. • The recommended dietary intake is 0.8 grams of protein per kilogram body weight, which average out to about 50 to 60 grams per day or 10-12 percent of daily calories. • It appears that most people are staying within the guidelines. • However, most of the protein people eat is of animal origin. • Although animal products are an excellent source of complete protein, they tend to be higher in saturated fats and cholesterol compared with foods high in plant protein. • On the other hand, animal’s protein is usually a better source of dietary iron and other minerals like zinc and copper than plant protein is. • Four ounces of meat, fish, or poultry, together with two glasses of skim milk, will provide the average individual with daily RDA for protein totaling about 45 grams. • Combining this animal protein intake with plant foods high in protein, such as whole-grain products, beans and peas, and vegetables, will substantially increase protein intake and more than meet your needs. 9. Choose a diet adequate in calcium and iron • This is particularly important for women and children. Skim or low-fat milk and other low-fat dairy products are excellent source of calcium. • For example, one glass of skim milk provides nearly one-third the RDA for calcium. • Iron is found in good supply in the meat and starch exchanges. • Lean or very-lean meat should be selected so as to limit fat intake and whole-grain or enriched products should be chosen over those made with bleached, unenriched white flour. 10. Children and others susceptible to tooth decay should obtain adequate fluoride. • This is particularly important during childhood when the primary and secondary teeth are developing, for fluoride helps prevent tooth decay by strengthening the tooth enamel. • Your water supply may contain sufficient fluoride—naturally or artificially- to provide an adequate amount, but if not, fluoride supplements or use of fluoride toothpaste is recommended. 11. In general, avoid taking dietary supplements in excess of the RDA in any one day • Dietary supplements of most vitamins and minerals are not necessary for individual consuming a balanced diet. • If you adhere to the recommendation listed here, you are not likely to need any supplementation at all, for the consumption of nutrient dense foods should guarantee adequate vitamin and mineral nutrition. 12. Eat fewer foods with questionable additives. • The general consensus is that most additives used in processed foods are safe. • But several health agencies, recommend caution with additives such as saccharin and nitrates, which have been linked to the development of cancer in laboratory animals. • And other substances such as sulfites and certain food colours, which may cause allergic reaction in some individuals. • Eating fresh, natural foods is one of the best approaches to avoiding additives. • HEALTHY EATING STEPS Healthy Eating Steps • To help make healthy choices of food easy, all food have been arranged into three food steps. Step 3 • Fats and oils-example – palm oil, all types of vegetable oil, palm soup , margarine, planta, sheabutter, avocado pear, • Example of one serving/meal • 1/3 small tomato tin of oil(3 dessertspoon) • ½ match box size sheabutter • 3 soup ladleful oily soup(palm soup/groundnut soup • avocado pear- 1/8 large , ¼ small, • 2-3 servings daily Step 2 • Animal and Vegetable protein • Examples- all types of meat, fish, chicken, beans, cheese, crab, eggs, milk, snails, groundnuts and all nuts and plant seeds like agushie. • Examples of one serving/meal • 1 joint chicken- remove skin • 1-3 match box size meat-lean meat • 1 medium fish • 2 eggs per week • ¼ evaporated tin milk, • 1 teaspoon- powdered milk • 2-3 stewing spoons of beans Step 1 • Starches, vegetables and fruit • Starches- fufu, kenkey, banku, akpler, omo tou, gari, bread, cassava, plantain, yam and rice( eat enough to satisfy) 3-4 servings daily. • Vegetables: okro, garden eggs, tomatoes, aleefu, ayoyo, kontomire, cassava leaves, sweet potatoes leaves, onion, pepper, green beans, cabbage, carrots, lettuce, cucumber, bra, bito bitter leaves2-3 servings daily. • Fresh fruits- orange, pawpaw, watermelon, mango, pineapples, apple, grape fruit, lemon(one slice of fresh fruit) 2-3 servings daily. Food labels • Knowing how to interpret food label, to prepare foods, and to avoid dietary contaminants may guide you in developing a nutritious, safe, and healthful diets. • By law, food labels must contain the following information: List of ingredients-ingredients will be listed in descending order by weight. Serving size- serving sizes must be expressed in both household measures such as cups and metric measures such as milliliters to accommodate users of both types of measure. Servings per container. Amount per serving of the following: Total calories Calories from fat Total fat Saturated fat Cholesterol Sodium Total carbohydrates Dietary fiber Sugars Protein Vitamin A Vitamin C Calcium Iron The following may be listed voluntarily Calories from saturated fat Polyunsaturated fat Monounsaturated fat Potassium Soluble fiber Insoluble fiber Sugar alcohols How can people use this information to select healthier diet • To provide information to help consumers see how foods may be part of a daily diet plan, a new label reference value, the Daily Value(DV) has been created. • The DV for a nutrient represents the percentage contribution one serving of the food makes to the daily diet for that nutrient based on current recommendation for healthful diets. • A lower DV is desirable for total fat, saturated fat, cholesterol, and sodium, while a higher DV is desirable for total carbohydrates, dietary fiber, iron, calcium, vitamins A and C The diet history: the technique of obtaining dietary information • A brief (assessment) diet history consists essentially of the same steps but requires less detailed probing for quantities. • 24-hour recall. Take the patient through the previous day meals noting times of all meals and snacks and what was eaten. • This is relatively easy to do, concentrates the patient‘s mind on food and gives a guide to meal patterns. If the respondent is an inpatient, establish the pattern of a typical day at home . • If the 24-hour recall is difficult, then a diet history is probably impossible! • Establish the quantities eaten on 24-hour recall. • This relates to one specific day, and is therefore less hypothetical than ‘what quantity might you eat? • Get the patient to describe quantities, which will give a guide to appetite and a cross-check on reliability of later answers. If possible, use portion models. • Establish the weekly pattern • Is the specific 24-hour pattern different in any way from the ‘usual’ pattern? Take the patient through the day again. • What other dishes might be eaten at each meal? What happen on Saturday and Sunday? What happen if the respondent is working a different shift? • How often does he go out? How often does he have visitors? What dishes would be eaten? • Probe specifically for sweets, and snack and other items consumed between meals, also alcoholic drinks. • Establish likely quantities. • Use portion models; it is easier for the respondent to say ‘my portion looks like that ’than to search for verbal descriptions, particularly if inarticulate. • The interviewer’s interpretation is also likely to be more accurate. • Respondent who do their own shopping can also provide information on quantities bought and for how many people. • Establish recipes for composite dishes. This is not always possible with those who do not cook. • Cross-checks the information already obtained against a list of foods appropriate for the purpose of the study. • e.g. to assess vitamin C, only fruit and vegetable (and composite dishes containing them) and squashes, need to be include. • The cross –checking can take the form of a set of cards handed to the respondent, rather than the interviewer questioning about each food individually, for each food, ascertain how frequently a ‘portion’ is eaten on a daily , weekly or monthly basis. • Particularly in a full diet history this section demands the best of the interviewer’s techniques, as it can be lengthy, repetitious and boring. Essential points to remember • Do not assume anything about patient’s meal patterns, recipes or portion sizes. • It is all too easy to assume meal patterns for people, e.g. ‘ Fridays we have fried fish ’, what does the respondent mean by this? Is it cod coated in butter and deep fried, or plaice lightly of tossed in butter, or some thing else? • Do not assume it actually means what you think it means; check it. If there is not a full description of the food, you may not be able to complete the calculation later. • Write every thing down. If information is received from the respondent but not recorded, then the interviewer’s memory becomes a factor in the accuracy of the diet history. • Check that you have not made any obvious mistake like recording 1000g instead of 10g of sugar in tea. • Checking that you have recorded the respondent accurately is as important as checking that the respondent has reported fully. • It should be possible for someone else to check and calculate a diet history and get the same results as the interviewer. Use pre-designed form and not scraps of paper. • Watch for non-verbal clues of boredom or irritation as it is difficult to avoid the inquisitorial aspect. • To counteract this, break the flow of questioning by making some comments on how much time is needed to complete the interview or a humorous reference to the number of questions being asked. Problems of the diet history Holding all the points on which information is needed in one’s head is difficult, particularly if inexperienced. Questions may be phrased inappropriately, particularly while thinking of others points to be covered. It is easy to put words into the respondent’s mouth. Beware of leading questions. Verbal descriptions of quantity may be very unreliable and may be mistranslated by the interviewer. Bias is introduced by the patient’s memory and subjective impressions. • • • • For instance (a) A tendency to over –remember ‘proper’ meals. (b)A tendency to under-remember snacks. (c)I always have fish on Friday’s may in fact mean two Fridays out of three. • (d)Memory is weighted by the last seven days. • (e)Cross –checking generally overestimates food used infrequently, i.e. if liver is eaten ‘once a mouth; it is probably in fact less frequencies are probably more reliable. The more irregular the pattern, the less reliable a diet history tends to be. Patients may not be entirely truthful. Analysis and interpretation of information • Assessment of food intake • Depending on the purpose of taking the diet history, the food intake may be assessed or analyzed in a variety of ways. By relating the food intake to a daily food guide. By using knowledge of food composition to make a judgment about some aspects of the diet, e.g. the adequacy of fiber intake or the likely contribution of the diet to dental caries. By using a table of approximate food values to make a crude calculation of the intake of one or more dietary constituents. By using detailed tables of food composition to calculate the intake of specific nutrients. • Points1-3 above are relevant to the brief diet history and point 4 to the full diet history. Assessment of nutrient intake • Nutrient intake =nutrient content of food × portion weight × frequency of consumption. • For example, compare the relative contributions of parsley and milk to vitamin C intake. • Parsley provides 150mg/100g×1gportion ×once/week=0.2mg/day • Milk provides 1.5mg/100g×30g portion × eight/day=3.6 mg/day. • Be careful to select from the tables the food which best represents the food described by the respondent. Similarly, care must be taken in translating the respondent’s description of portion sizes into weights. Evaluation The quality of the personal contact. Was the respondent relaxed and talking at ease? Validity: am I measuring what I think I am measuring? Is the answer obtained the correct answer? Reality: Can I get the same answer on two separate occasions (unless the respondent has changed eating habits)? Standardization of interview techniques and of tools used in analysis (and methods of use) is essential otherwise different interviews will obtain different result. Verbal communication skills • During the presentation of questions the following ideas should be considered. You credibility in the eye of the patient will increase if you demonstrate expertise and show concern and dedication. Try to be forceful but not overbearing. Rapport is increased if the patient perceives some similarity with you, eg. Physical similarityage, sex, race, ethnic features, dress, dialect, etc. However, hidden barriers may be set up by the lack of such similarities, e.g. Young dietitian and older patient, slim dietitian and fat patient. Rapport is also helped if you begin with an aspect that the patient would want to hear. Show by your manner that you are interested and that your attention is uninterrupted. Your manners and your words should not indicate shock or surprise at answer and should not imply criticism or impatience towards what is being said. You have the power to reinforce many behaviors of the patient. It should be used judiciously, e.g. Attentive listening; eye-contact; addressing the person by name; saying ‘goodʹ, ‘that is interesting’, reinforce specific behaviours. Pause for a few seconds after the patient has apparently finished and before more questions are asked, in order to give him a chance to speak further. Remember that under normal circumstances there is no time for the patient to be prepared and there is the inevitable pressure of trying to provide a quick reply when an interviewer is waiting for your answer! Return to topics on which the patient ‘froze’ in order to determine if lack of response is significant. Avoid bringing the patient abruptly back when he digresses. Use appropriate wording for ‘probing’ question to maintain a good relationship, e.g. ‘I am interested in what you are saying could you tell me more about that?’. • You could also adopt a questioning tone when repeating key sentences of the patient to indicate that you want elaboration. Leave any personal or potentially embarrassing question as near to the end as possible so that a good rapport has already been established. At the end of the interview, thank the respondent and give a positive indication of the usefulness of the interview. DIET LABORATORY Specific objectives • Learn to use local foods to prepare nutritious meals. • Learn to combine foods in a number of ways to constitute a variety of meals to avoid monotony in feeding any group of people. • Learn the equivalents measures of the weights of different foods items. • To familiarise oneself with appropriate serving portion for the various age groups in the family. • Learn to use Food Composition Tables to calculate the energy and nutrient contents of foods and meals. • Be able to evaluate the nutritional adequacy of daily. Assessment • 10% for the paper work • 10% for practical work • Total = 20% Uses Of The Composition Table • The nutrients values are based on quantitative analysis of the food samples so it is important that they represent the average composition of typical foods. • They are useful in clinical practice can be used to assess nutritionally related disease and to accurately prescribe diets containing known amounts of nutrients. • It can be used to determine the nutrients adequacy of diets. • It can be used to detect imitation or substitute food Limitations • No food composition can represent the exact composition of food that is eaten. • For prepared dishes the recipe used in the table might not be same as the person whose dietary data you are collecting. • If adequate sampling was not done during compilation of the table, you end up with food samples that are not representative. • There could also determination be analytical errors in the Assignment • Plan, prepare and serve a suitable breakfast, lunch and supper for a 10-year old boy from Eastern region. Attempt to meet the RDA and cost the meal. • RDA for a 10- year old boy(FAO/WHO) • Energy – 2200 • Protein- 34 gm Meal planning steps • Select the staple food item • Select the vegetable that goes very well with the staple. • Select a protein-rich item • Select a oil if necessary • Determine quantities of ingredients • Lunch – jollof rice 2 slices of pawpaw • List of ingredients Rice -- 1kg---10GHC Fresh tomatoes ----500grams----- 2GHC Oil(peanut) Onions Pepper Salt Smoked fish(salmon) Beef • Weigh all ingredients and their prices on a sheet of paper. Food item Rice Oil Beef Tomatoes Onion Mackerel Cost (GHC) t Weight(oz/gm) Energy (kcal) Protein (gm) Diabetic diet • Globally, as of 2010, an estimated 285 million people had diabetes, with type 2 making up about 90% of the cases. Its incidence is increasing rapidly, and by 2030, this number is estimated to almost double. • Diabetes mellitus occurs throughout the world, but is more common (especially type 2) in the more developed countries. • The greatest increase in prevalence is, however, expected to occur in Asia and Africa, where most patients will probably be found by 2030. • The increase in incidence in developing countries follows the trend of urbanization and lifestyle changes, perhaps most importantly a "Westernstyle" diet. Definition • Diabetes is a metabolic disorder characterised by high blood glucose and either insufficient or ineffective insulin. Pathophysiology • An understanding of the pathophysiology of diabetes rests upon knowledge of the basics of carbohydrate metabolism and insulin action. • Following the consumption of food, carbohydrates are broken down into glucose molecules in the gut. Glucose is absorbed into the bloodstream elevating blood glucose levels. • This rise in glycaemia stimulates the secretion of insulin from the beta cells of the pancreas. Insulin is needed by most cells to allow glucose entry. • Insulin binds to specific cellular receptors and facilitates entry of glucose into the cell, which uses the glucose for energy. • The increased insulin secretion from the pancreas and the subsequent cellular utilization of glucose results in lowered of blood glucose levels. • Lower glucose levels then result in decreased insulin secretion. • If insulin production and secretion are altered by disease, blood glucose dynamics will also change. If insulin production is decreased, glucose entry into cells will be inhibited, resulting in hyperglycemia. • The same effect will be seen if insulin is secreted from the pancreas but is not used properly by target cells. • If insulin secretion is increased, blood glucose levels may become very low (hypoglycemia) as large amounts of glucose enter tissue cells and little remains in the bloodstream. • Following meals, the amount of glucose available from carbohydrate breakdown often exceeds the cellular need for glucose. • Excess glucose is stored in the liver in the form of glycogen, which serves as a ready reservoir for future use. • When energy is required, glycogen stores in the liver are converted into glucose via glycogenolysis, elevating blood glucose levels and providing the needed cellular energy source. • The liver also produces glucose from fat (fatty acids) and proteins (amino acids) through the process of gluconeogenesis. • Glycogenolysis and gluconeogenesis both serve to increase blood glucose levels. • Thus, glyceamia is controlled by a complex interaction between the gastrointestinal tract, the pancreas, and the liver. • Multiple hormones may affect glycemia. Insulin is the only hormone that lowers blood glucose levels. • The counter-regulatory hormones such as glucagon, catecholamines, growth hormone, thyroid hormone, and glucocorticoids all act to increase blood glucose levels, in addition to their other effects. Classification • There are three major types namely; • Type 1 • Type 2 • Gestational diabetes Type 1 Diabetes • The underlying pathophysiologic defect in type 1 diabetes is an autoimmune destruction of pancreatic beta cells. • Following this destruction, the individual has an absolute insulin deficiency and no longer produces insulin. • Autoimmune beta cell destruction is thought to be triggered by an environmental event, such as a viral infection. • Genetically determined susceptibility factors increase the risk of such autoimmune phenomena. • The onset of type 1 diabetes is usually abrupt. It generally occurs before the age of 30 years, but may be diagnosed at any age. • Most type 1 diabetic individuals are of normal weight or are thin in stature. • Since the pancreas no longer produces insulin, a type 1 diabetes patient is absolutely dependent on exogenously administered insulin for survival. Type 2 Diabetes • The underlying pathophysiologic defect in type 2 diabetes does not involve autoimmune beta-cell destruction. Rather, type 2 diabetes is characterized by the following three disorders: Peripheral resistance to insulin, especially in muscle cells. Increased production of glucose by the liver. Altered pancreatic insulin secretion. • Increased tissue resistance to insulin generally occurs first and is eventually followed by impaired insulin secretion • The pancreas produces insulin, yet insulin resistance prevents its proper use at the cellular level. Glucose cannot enter target cells and accumulates in the bloodstream, resulting in hyperglycemia. • The high blood glucose levels often stimulate an increase in insulin production by the pancreas; thus, type 2 diabetic individuals often have excessive insulin production (hyperinsulinemia). • Over the years, pancreatic insulin production usually decreases to below normal levels. • In addition to hyperglycemia, type 2 diabetic patients often have a group of disorders that has been called "insulin resistance syndrome" or syndrome X • Obesity contributes greatly to insulin resistance, even in the absence of diabetes. In fact, weight loss is a cornerstone of therapy for obese type 2 diabetic patients. • Insulin resistance generally decreases with weight loss. • Obesity also may explain the dramatic increase in the incidence of type 2 diabetes among young individuals in the world in the past 10 to 20 years. • Once considered a disease of adults, type 2 diabetes has increased among the youth in direct correlation with the increase in the average weight of children and young adults during that time period. Gestational Diabetes • Gestational diabetes occurs in approximately 4% of pregnancies. • It usually develops during the third trimester and significantly increases perinatal morbidity and mortality. • The proper diagnosis and management of gestational diabetes improves pregnancy outcomes. • As with type 2 diabetes, the pathophysiology of gestational diabetes is associated with increased insulin resistance. • Most patients with gestational diabetes return to a normoglycemic state after parturition; • However, about 30 to 50% of women with a history of gestational diabetes will develop type 2 diabetes within 10 years. Impaired Glucose Tolerance and Impaired Fasting Glucose • The conditions known as Impaired Glucose Tolerance (IGT) and Impaired Fasting Glucose (IFG) represent metabolic states lying between diabetes and normoglyceamia. • People with IFG have increased fasting blood glucose levels but usually have normal levels following food consumption. • Those with IGT are normoglycemic most of the time but can become hyperglycemic after large glucose loads. • IGT and IFG are not considered to be clinical entities; rather, they are risk factors for future diabetes. • The pathophysiology of IFG and IGT is related primarily to increased insulin resistance whereas endogenous insulin secretion is normal in most patients. • Approximately 30 to 40% of individuals with IGT or IFG will develop type 2 diabetes within 10 years after onset. Symptoms Polyuria (frequent urination) Polydipsia (increased thirst) Polyphagia (increased hunger). Physiological basis of symptoms of diabetes • Without sufficient insulin, glucose accumulates in the blood, resulting in hyperglycemia. • Normally, the kidneys retain glucose rather than excrete it, but when blood glucose rises too high, the excess ‘spills’ into the urine (glucosuria). • High blood glucose creates an osmotic effect, drawing water from the cells into the blood. • Furthermore, as glucose spills from the blood into the urine, water leaves with it. • Thus both the intracellular fluid and extracellular fluid become depleted, and as a consequence, people with uncontrolled diabetes can become severely dehydrated. • They produce excessive urine (polyuria) and being dehydrated they may also experience excessive thirst (polydipsia). • These are early symptoms of diabetes. • Both types of diabetes deprive cells of fuels they need for energy. • Amino acids and glucose may abound in the body fluids, but the cells have little access to them and therefore mobilize their own protein and fat supplies for energy. • They break down large amounts of fatty acids, and liver responds by making ketones bodies, which accumulates in the blood (ketonemia). • Ketones in the blood lower its pH because they contain acid groups in their their structure. • Ketones may begin to appear in the urine (ketonuria) • In addition, sodium and potassium become depleted because the kidneys excrete them along with ketones. The loss of sodium and potassium, both base formers, worsens the acidosis. • When acidosis becomes severe enough, a potential fatal coma may follow(diabetic coma or insulin shock). • Losses of glucose and ketone bodies(both energy sources) in the urine, and protein breakdown, leads to weight loss. • The person with IDDM is likely to be thin and may eat excessively(polyphagia). Risk factors Family history Obesity Lack of exercise Poor diet Excess consumption sugar-sweetened drinks↑ Saturated fats↑ Monounsaturated and polyunsaturated ↓ Urbanization Stress Diagnosis Condition 2 hour glucose mmol/l(mg/dl) Fasting blood glucose mmol/l(mg/dl) Normal <7.8 (<140) <6.1 (<110) Impaired fasting glyceamia <7.8 (<140) ≥ 6.1(≥110) & <7.0(<126) Impaired glucose tolerance ≥7.8 (≥140) <7.0 (<126) Diabetes mellitus ≥11.1 (≥200) ≥7.0 (≥126) Complications • In uncontrolled diabetes, small arteries that feed tissues become blocked or destroyed causing the tissues to die from lack of nourishment. The end result are; loss of circulation to the legs and feet, sometimes leading to amputation; loss of circulation to the heart; sometimes leading to heart attack or strokes; loss of vision due to retina degeneration (retinopathy) loss of nerve function(neuropathy) causing loss of sensation in the limbs; and loss of kidney function (nephropathy) sometimes requiring hospital care or kidney transplant. • Infections are likely because bacteria strive in glucose-rich blood and can advance undetected in limbs already made insensitive by loss of nerve function. Objectives of dietary treatment To achieve optimal blood glucose concentration. To achieve optimal lipid concentration. To prevent, delay, complications. and treat-diabetes-related To improve health through balanced nutrition. To achieve weight loss in the overweight diabetic To minimize the risk of hypoglycemia in diabetics treated with insulin and certain oral hypoglycemic agents. General dietary guidelines • Modern dietary management of diabetes essentially involves modification of the quality and quantity of food to be taken by the diabetic patient. • The following guidelines are applicable to diabetes irrespective of type, weight, status, age, gender, or occupation Separate meals or specially prepared foods are not necessary Eat three meals a day about the same volume at the same time everyday. Snacks(small meal may be added if necessary). Allow 4-5 hours between meals. Take 10-20 minutes to eat a meal. Insulin injection and diabetes tables except metformin should be taken 30 minutes before meals. Metformin should be taken with meals. No fasting Most of the carbohydrates consumed should be in the form of starch(polysaccharides) such as maize, rice, beans, bread, potatoes, yam, cassava, plantain. All refined sugars such as glucose, sucrose, and their products(soft drinks, malt drinks, sweets, toffees and honey should be avoided except during severe illness or episodes of hypoglyceamia. These foods contain sugars in simple form which is easily absorbed causing rapid rise in blood sugar. Non-nutritive sweetener, e.g. canderel, saccharine, nutrasweet, aspartame are suitable sugar substitutes for diabetics subjects. Animal fat such as butter, lard, egg yolk, and other foods high in saturated fatty acids and cholesterol should be reduced to a minimum and replaced with polyunsaturated fats such as vegetable oils. Salt should be reduced whether hypertensive or not. Protein (fish, meat, beans, crab, crayfish, soybean and chicken) and salt are restricted for those with diabetic nephropathy. The items allowed for free consumption include; (a)water, green vegetables, tomatoes, onions, cucumber peppers, vegetable salad without cream. (b)Any brand of tea, coffee or drinks that contain very low or no calories For patients too ill eat solid food, a fluid or semi solid diet should be substituted . The following should be given; • Any soup plus one of the following : 2 egg size of fufu, banku, TZ, apkle, potatoes or agidi • 2 laddleful of mpotompoto • ½ yogurt or ice cream or ½ bottle of soft drink • ½ cup porridge, mashed kenkey or fula plus milk and ½ dessertspoon of sugar if desired. Patients treated with insulin or certain oral hypoglyceamic agents e.g, sulphonylureas, must be advised to eat regularly and often to prevent hypoglyceamia. Cigarettes smoking should be avoid by diabetics patients. Alcohol should be taken in moderation. Small meals spaced over the day rather than one or two big meals are helpful in avoiding postprandial peaks in blood sugar. The diet should be varied to avoid monotony and provide a wider range of nutrients for healthy living. In case of on coming hypoglycaemia (low blood sugar level), Patients may feel shaky, sweaty, dizzy, weak and fainting: patients should be advised to take one of these: • 1 dessertspoon(eating spoon) of sugar or honey( in water if possible) • 3 cubes of sugar dissolved in water • ½ bottle of soft drink or ½ refresh. • Regular insulin has an onset of action (begins to reduce blood sugar) within 30 minutes of injection, reaches a peak effect at 1-3 hours. Anthropometrics and dietary recommendations • The broad principle of daily energy recommendation for diabetics is based on maintaining the ideal body weight for the height of the individual. Underweight(BMI<18.5kg/m²) The goal here is to gain or regain weight. To gain weight the patient must take in more calories than needed to meet the body’s physical requirements. Emphasis should be on balance diet Keeping to his or her favourite foods Regular meals Increasing serving sizes to about twice what the patient is already consuming. • Weight gain is gradual and the patient should be regularly reviewed (at 2 to 4-week intervals) and further increase in ‘serving sizes’ made when deem necessary. Overweight (BMI>25kg/m²) The aim here is to reduce weight while optimising drug therapy. Weight reduction must be gradual over a period of time-the target should be about 1.01.5kg loss every 1 to 2 weeks In limiting the number of calories calories consumed per day, the patients does not need to abstain from his/her favourites foods What is needed is to know how much to cut back on portion sizes(portion control) The target initially is to cut down to half the previous serving sizes per meal with a monthly review and subsequent reduction when deemed necessary. The serving size reduction should affect particularly the complex carbohydrates, which constitute the main staple foods in the tropics. Many type 2 diabetes patients find portion control an important aspect of the solution to losing weight. By monitoring the ‘serving sizes’ combining it with regular exercise drugs(especially metformin), patients enjoy a wider variety of meals including favourites foods and still lose weight. and and can their Portion control can also help overcome the biggest challenge, which is maintaining healthy weight. When overweight diabetic patients shed some weight by trimming down ‘serving sizes’ and calories, insulin sensitivity improves, thereby optimising drug therapy. Normal weight(18.5-24.9kg/m²) • The fundamental principle behind maintenance of body weight is the energy balance. • This group should encouraged to maintain their weight by: Maintaining current ‘portion sizes’ Eating about the same amount of food each day Taking their drugs at the same time each day Exercising at the same time each day These patients should endeavour to choose their daily foods from starches, vegetables, fruits and protein while limiting the amount of fat. Ethical issues in dietetics practice in Ghana REFER TO PATIENT’S CHARTER