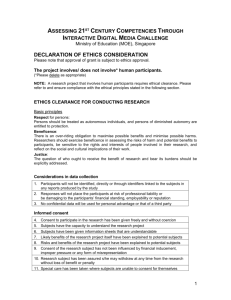
Ethical Principles for Biomedical Research Involving Human
advertisement

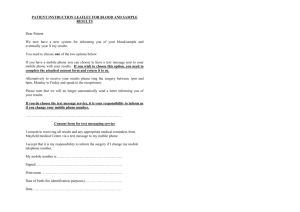
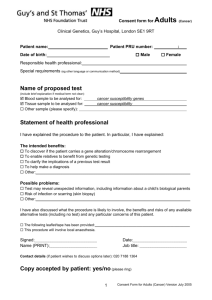
Ethical Principles for Biomedical Research Involving Human Subjects: Overview of International Guidelines Maria Fidelis C. Manalo, MD, MSc Epidemiology Department of Community & Family Medicine Far Eastern UniversityNRMF Medical Center Philippines Public Concern for Vulnerable Subjects Nazi Experiments and the Nuremberg Trials Tuskegee Syphilis Study-involvement of black males Willowbrook Study-hepatitis study among children in New York State institution for mentally defective persons Jewish Chronic Disease Hospital Studyinjection of live cancer cells into patients to study transplant rejection process San Antonio Contraceptive Study-study of side effects of contraceptives on Mexican American women In research using human subjects, several categories of persons maybe involved: Normal healthy adults, including the investigator, and elderly persons Sick adults, including the acutely and terminally ill People living in highly controlled situations, such as, prisoners, soldiers, and students Children, both healthy and ill Mentally incompetent persons, whether adults or children Unborn fetuses or still living aborted fetuses Use of Vulnerable Persons Not forbidden by ethical codes or regulations Need for justification for their inclusion Unsuitability of less vulnerable populations Use of mitigation to address vulnerability NUREMBERG CODE: INFORMED CONSENT The voluntary consent of the human subject is absolutely essential. This means that the person involved should have legal capacity to give consent; Should be . . . able to exercise free power of choice, without the intervention of any element of force, fraud, deceit, duress, . . . or coercion; Should have sufficient knowledge and comprehension . . . . NUREMBERG CODE: INFORMED CONSENT The duty and responsibility for ascertaining the quality of consent rests upon . . .each individual who initiates, directs, or engages in the experiment. It is a personal duty that may not be delegated ELEMENTS OF INFORMED CONSENT (1) DISCLOSURE In general necessary items to disclose include: a) the patient’s current medical status including the likely course if no treatment is provided. b) the contemplated procedure or medication c) alternative available procedures or medication d) anticipated risks and benefits of both e) a statement offering an opportunity to ask further questions f) in case of research, his right to withdraw any time g) a professional opinion about the alternatives ELEMENTS OF INFORMED CONSENT (2) COMPREHENSION 7th grade level (US Standard) Language understood by the subject Oral or written quizzes to assess comprehension Use of educational intervention prior to getting consent Allowed into research environment to experience routine and procedures ELEMENTS OF INFORMED CONSENT (3) VOLUNTARINESS - The patient must of his own free will make a choice without being unduly pressured by anyone else. Being free in making a decision means that the patient owns the decision, that the decision is the patient’s alone, that the patient has chosen the option based on the information disclosed to him/her. ELEMENTS OF INFORMED CONSENT (4) COMPETENCE - patient’s capacity for decision making. One is considered competent when (a) one has made a decision (i.e. one can choose between alternatives) (b) one has the capacity to justify one’s choice (i.e, give reasons for one’s choice) (c) one justifies one’s choice in a reasonable manner HUMAN SUBJECTS OVER SCIENCE AND SOCIETY . . . considerations related to the well-being of the human subject should take precedence over the interests of science and society. (Helsinki Declaration, par. 5) Protection of Special Populations Embryos And Human Fetuses Since the human individual, in the prenatal stage, must be given the dignity of a human person, research and experimentation on human embryos and fetuses is subject to the ethical norms valid for the child already born and for every human subject. Protection of Special Populations Pregnant Women, Embryos And Human Fetuses Research in particular, that is the observation of a given phenomenon during pregnancy, can be allowed only when “there is moral certainty that there will be no harm either to the life or the integrity of the expected child and the mother, and on the condition that the parents have given their consent.” THERAPEUTIC CRITERIA ONLY Experimentation is possible only for clearly therapeutic purposes, when no other possible remedy is available. “No finality, even if itself noble, such as the foreseeing of a usefulness for science, for other human beings or for society, can in any way justify experimentation on live human embryos and fetuses, whether viable or not, in the maternal womb or outside of it. Protection of Special Populations Experimentation of embryos or fetuses has the risk, indeed in most cases the certain foreknowledge, of damaging their physical integrity or even causing their death. To use a human embryo or the fetus as an object or instrument of experimentation is a crime against their dignity as human beings. Protection of Special Populations “The practice of keeping human embryos alive, actually or in vitro, for experimental or commercial reasons,” is especially and “altogether contrary to human dignity.” The informed consent, normally required for clinical experimentation on an adult, cannot be given by the parents, who may not dispose of the physical integrity or the life of the expected child. PROPORTIONALITY OF RISKS TO BENEFITS Degree of risk to be taken should never exceed . . . humanitarian importance of the problem to be solved . . . . (Nuremberg, #6) Medical research . . . should only be conducted if the importance of the objective outweighs the inherent risks and burdens to the subject. (Helsinki, #18) Right to refusal or withdrawal of treatment “the patient has the right to refuse or withdraw from treatment to the extent permitted by law and to be informed of the medical consequences of his action.”- Patient’s Bill of Rights a patient may refuse or withdraw from medical treatment because their religious convictions prohibit them from doing so (e.g., a patient who is a member of a particular religious sect may refuse to undergo blood transfusions) PLACEBO MAY BE USED: When there is no established effective intervention; When withholding an established effective intervention would expose subjects to, at most, temporary discomfort or delay in relief of symptoms; When use of an established effective intervention as comparator would not yield scientifically reliable results and use of placebo would not add any risk of serious or irreversible harm to the subjects (CIOMS #11) Are there ethical issues in social science or behavioral research? Most common methodology used involves interviewing people and asking questions “We would just like to ask some questions…” “We would just like to observe…” “We would just like to share your life…” Focus Group discussion (FGDs), Survey Does not involve invasive procedures Ethical Issues in Social Science & Behavioral Research Privacy Confidentiality Linking behavior with medical procedure DO NO HARM Experiment should . . . avoid all unnecessary physical and mental suffering and injury. (Nuremberg, #4) Forms of Harm to Human Subjects in Behavioral Research Psychological harm – recalling a traumatic event Social stigma – loss of reputation Cultural effects – going against existing cultural norms Political effects – disturbing existing power relationships Economic repercussions – loss of jobs HOW TO AVOID HARM The experiment should be conducted only by scientifically qualified persons. (Nuremberg #8) . . . human subject should be at liberty to bring the experiment to an end . . . (#9) . . . terminate the experiment at any stage, if . . . continuation of the experiment is likely to result in injury, disability, or death (#10) HOW TO AVOID HARM [Ensure that] risks involved have been adequately assessed and can be satisfactorily managed. Cease . . . investigation if: 1. 2. the risks are found to outweigh the potential benefits, or there is conclusive proof of positive and beneficial results (Helsinki #17) Mitigating harm to human subjects Research design- community inputs Adequate research preparationfamiliarization with local culture, sociopolitical structures, traditions and cultural norms Good reason to conduct research in a particular community Ethical Consideration Section in the protocol NBAC Guideline “ Whenever possible, preceding the start of research, agreements should be negotiated by the relevant parties to make effective intervention or other research benefits available to the host country after the study is completed.” Mitigating harm to human subjects Research methodologies should avoid harm Mechanisms for protection of privacy and confidentiality Avoidance of social stigmatization Process of data storage Adequate infrastructure to protect privacy Research methodologies should provide opportunities for empowerment-reflexivity Mitigating harm to human subjects-Reviewing the protocol Technical review Risk-benefit analysis Benefits should be defined in the protocol Provisions for support mechanisms Consent process should be as strict as requirements in clinical trials Recruitment procedures Full disclosure of information Reconsenting mechanisms Feedback to community Mitigating harm to human subjects- Reviewing the protocol Culturally competent consent form Individual consent Family consent-secondary subjects Community consent Mechanisms for protection of privacy and confidentiality defined in the consent form of information sheet Provision of support/coping mechanism Need to take precaution to protect identity of host community Informed consent: Community Context - CIOMS “When it is not possible to request informed consent from every individual to be studied, the agreement of a representative of a community or group should be sought, but the representative should be chosen according to the nature, traditions and political philosophy of the community or group.” Feedback to the Community Reporting results to the community A good means to highlight good practices: positive reinforcement Suggestions for improvement should be presented as constructive recommendations Public forum: a means to get public commitment from public officials Opportunities for researchers to connect community to larger community RELEVANCE & RESPONSIVENESS OF RESEARCH Medical research is only justified if there is a reasonable likelihood that the populations in which the research is carried out stand to benefit from the results of the research. (Helsinki #19) CIOMS RELEVANCE AND RESPONSIVENESS The sponsor and the investigator must make every effort to ensure that: 1. 2. the research is responsive to the health needs and the priorities of the population . . . ; and any intervention or product developed, or knowledge generated, will be made reasonably available for the benefit of that population. (CIOMS #10) GENETIC RESEARCH: Privacy, Confidentiality and Integrity Respect the privacy of the subject, the confidentiality of the patient's information and minimize the impact of the study on the subject's physical and mental integrity (Helsinki #21) MEDICAL RECORDS & BIOLOGICAL SPECIMENS Exempted from individual consent requirement only if an ethical review committee has determined that: Research poses minimal risk Rights or interests of the patients will not be violated privacy and confidentiality or anonymity are ensured Research is designed to answer an important question Impracticable if the requirement for informed consent were to be imposed (CIOMS) HUMAN GENETIC DATA Clear, balanced, adequate and appropriate information shall be provided to the person whose prior, free, informed and express consent is sought. Information shall . . . specify the purpose for which human genetic data . . . are being derived, . . . used and stored (International Declaration on Human Genetic DataAdopted by the UNESCO General Assembly on 16 October 2003) WITHDRAWAL OF CONSENT (a) . . . Consent may be withdrawn by the person concerned unless such data are irretrievably unlinked to an identifiable person. (b) When a person withdraws consent, the person’s genetic data, proteomic data and biological samples should no longer be used unless they are irretrievably unlinked to the person concerned. (c) If the person’s wishes cannot be determined or are not feasible or are unsafe, the data and biological samples should either be irretrievably unlinked or destroyed. UNESCO Int’l Declaration, Art. 9 RIGHT TO BE, OR NOT TO BE INFORMED OF RESULTS The person concerned has the right to decide whether or not to be informed of the results UNESCO Int’l Declaration, Art. 10 GENETIC COUNSELLING . . . When genetic testing . . . is being considered, genetic counselling should be made available . . . . Genetic counselling should be nondirective, culturally adapted and consistent with the best interest of the person concerned. UNESCO Int’l Declaration, Art. 11 CLINICAL TRIAL REGISTRATION A Requirement for Publication Trials must register at or before the onset of patient enrollment. Selective reporting . . . distorts the body of evidence available for clinical decision-making. Trial results that place financial interests at risk are particularly likely to remain unpublished and hidden from public view. Anyone should be able to learn of any trial's existence and its important characteristics. BIBLIOGRAPHY 1. Ethical Review of Research: Overview of International Guidelines and Principles by Prof. Leonardo de Castro, Ph.D, Department of Philosophy, University of the Philippines, Diliman 2. Ethical Issues in Social Science Research: by Prof. Cristina E. Torres, Ph.D, College of Arts and Sciences, University of the Philippines, Manila & National Institute of Health 3. Protection of Vulnerable Subjects by Prof. Cristina E. Torres, Ph.D, College of Arts and Sciences, UP Manila & National Institute of Health 4. World Medical Association (WMA): Declaration of Helsinki, Tokyo, 2004 5. The Nuremberg Code 1947 BIBLIOGRAPHY 6. The CIOMS Guidelines Nov 2000, International Ethical Guidelines for Biomedical Research Involving Human Subjects 7. The NBAC Report Aug 2001, Ethical and Policy Issues in Research Involving Human Participants 8. International Declaration on Human Genetic Data, UNESCO, October 16, 2003 9. The Belmont Report, 1979, Ethical Principles and Guidelines for the Protection of Human Subjects of Research 10. Fifth Global Forum for Health Research, Paris, 2004