Case Example Sytems and Individual Error
advertisement

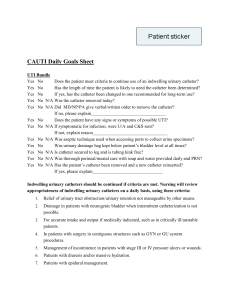
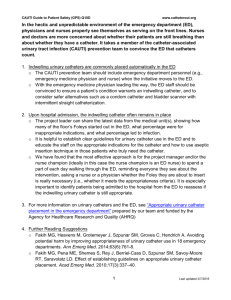
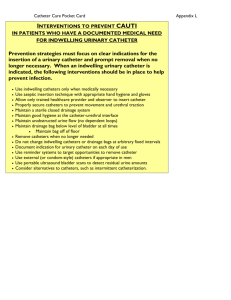
CASE STUDY IN COMBINED SYSTEMS AND INDIVIDUAL FAILURE Ethan Cumbler M.D. Assistant Professor of Medicine Hospitalist Section University of Colorado Hospital 2007 Case represents an example based on real case. Some details have been changed and case de-identified to preserve patient confidentiality CASE OF THE TRAUMATIC URINARY CATHETER REMOVAL 86 y/o male with hx of CHF, Afib, and Dementia presents with increased lower extremity edema and SOB. Documented to be non-compliant with medications for months. PMH CHF Afib Hypothyroid Osteoporosis Dementia Parkinson’s Urinary Incontinence CASE Allergies-NKDA Medications Noncompliant with: Linsinopril Amiodarone Carvedilol Furosemide Warfarin Asprin Calcium-Vit D Alendronate Carbidopa/levodopa Levothyroxine Social Hx Lives with wife who also has significant dementia. APS involved in his care multiple occasions Hospital Course- Day 1 Admit to Cardiology Service. For CHF exacerbation due to medication noncompliance. Treating with IV furosemide Indwelling urinary catheter ordered. Documented need for strict Is + Os along with presence of stage II sacral skin breakdown. Hospital Course- Day 3 Care transferred to Internal Medicine service. Patient transitioned to oral furosemide Medicine team is post-call and discusses patient on “sit down rounds” (not at bedside). No mention of urinary catheter on rounds Medicine Attending #1 notes presence of catheter while rounding alone later in day. Verbal order to nurse to remove catheter. At end of day Attending #1 discusses plan to remove catheter with Resident. Neither Attending #1 nor Resident write order to remove catheter. Nurse forgets to remove catheter in response to verbal order by Attending #1. Hospital Course- Day 4 Attending #1 is no longer on service (scheduled switch at end of week). Resident has day off Resident and Attending do not communicate intended catheter removal during check-out Intern not aware of plan to remove catheter Intern and Attending #2 do not discuss presence of urinary catheter or plan for it’s removal Hospital Course- Day 5 Intern has day off Resident returns to service. Notes presence of urinary catheter and assumes that it was removed but then replaced for a medical indication for which resident is not aware Hospital Course- Day 6 Patient wakes in the middle of the night confused. Gets out of bed and walks towards bathroom Catheter bag is attached to opposite side of bed, traction rips it (with bulb inflated) out of penis causing urethral tear and significant bleeding Pt had bleeding for 3 days requiring aspirin and heparin prophylaxis to be held. Urology consulted. Hct drops. One week after discharge patient was readmitted for transfusion STRUCTURED ANALYSIS OF MEDICAL ERROR Use (Systematic Analysis of a Medical Error form to guide discussion) Step 1 Adverse event, Medical error, Causation Was There an Adverse Event? Yes. A traumatic removal of an unnecessary urinary catheter represents an adverse event Was there a Medical Error? Yes. The failure to remove unnecessary urinary catheter despite plan to do so represented a medical error Were the two related? Yes. In this case the medical error directly lead to the adverse event. Step 2 Were There Systems Issues Which Contributed to This Error? -Communication -Information management -Technology -Supervision -Workload -Human resources support issues (staffing) Systems issues Communication Breakdown in intra-team communication based on failure to discuss plan of care during team rounds and fragmented communication of plan to remove catheter with some but not all members of the care team. Failure to sign-out elements of care during transitions off service. Use of verbal orders- a form of communication with nursing prone to failures and miscommunication Diffusion of responsibility- Attending did not write order believing that resident would do so. Resident assumed Attending had already written order. Systems issues Information Management Check-out system not formalized to include plan of care for items such as urinary catheters. Computerized nursing record tracks urinary catheter presence but lacks connection to physician accessed portion of electronic medical record. Since removal of urinary catheters is a physician-driven active process this removes opportunity for increased physician awareness and prevents electronic prompts to the physicians for removal. Systems issues Technology While decidedly low tech, the design of current indwelling urinary catheters predisposes to this form of urethral trauma. Use of condom catheter rather than indwelling catheter presents less risk of traumatic injury (assuming the goal is strict Is+Os or skin protection rather than obstructive uropathy) The design of the urinary catheter which encourages it to be attached to bed rather than the patients leg creates a form of single point restraint which may induce injury when a patient with dementia tries to get out of bed. Systems issues Supervision No significant issues Systems issues Workload Nursing had multiple patients with active issues on day of verbal order to remove catheter. This likely contributed to nurse forgetting to remove catheter. Low priority request easy to forget without reminder from written order Systems issues Human Resources Staffing model failed to preserve continuity of team. Both Attending and Resident went off service on same day. Multiple transitions between teams during short patient hospitalization. Step 3 Which Type of Individual Error Occurred? Knowledge based- mistake from inadequate or incomplete information or base of knowledge Skill based- performance error. Not doing the action which was intended. We think of this as a “slip” Rule based- the incorrect application of the information. We think of this as a “Judgment failure” Step 3 Which Type of Individual Error Occurred? Skill basedThe request to remove catheter was forgotten by nurse who received the verbal order (nurse became distracted by other tasks and forgot to do so in absence of written prompt) Step 4 List Heuristic Failures Leading to Individual Judgment Error There was no judgment error and thus Heuristics failure does not apply to this case Step 5 What Level Harm Occurred As a Result of The Adverse Event? 123456- No harm, error identified prior to affecting patient Minor temporary harm Minor permanent harm Major temporary Major permanent Death Harm Major temporary harm Bleeding sufficient to require transfusion represents a major adverse event but the patient did not suffer permanent injury Step 6 What Would You Disclose In This Case? In this case the fact of the urethral trauma due to the patient accidentally pulling out catheter in the night was disclosed but the medical error causing the catheter not to be removed was not discussed. It would be easy, but not ethically appropriate, to pretend that no error had occurred. Step 6 Disclosure It would be appropriate to explain to patient/family that the team had intended to remove catheter but that this had not actually occurred during the transitions over the weekend. The patient had become confused in the middle of the night and pulled the catheter out causing injury (facts of the case). Since the plan was to remove the catheter it is appropriate to express regret that this occurred and an expression such as a “wish statement”. “I recognized that with his confusion he is at increased risk for this sort of event. There was a good reason for the catheter to be placed but I wish that I had removed it earlier.” A straightforward apology is appropriate along with an explanation of how the error will change your practice to prevent this in the future Disclosure will be discussed in detail in the third seminar. Step 7 What Steps Could be Taken to Prevent This From Occurring in The Future Small group break-away sessions. Each group should be assigned an element contributing to the medical error Potential Steps Communication Bedside team rounding decreases chance that issues such as urinary catheter use will not be noticed and discussed in the plan. Team rounds later in the day would prevent fragmentation of communication Creation of checklist of items to be addressed on every patient in rounds decreases chance that multiple necessary elements will be missed (catheters, intravenous lines, DVT prophylaxis, skin care ect) Avoid verbal orders unless in emergency Clear delineation of responsibilities for who on a team will write orders Potential Steps Human Resources Personnel turnover is unavoidable but certain staffing models create more turnover than others. Staggering days off to prevent all senior members of the team from taking the same day off decreases risk of discontinuity. Potential Steps Information Management Change in system of care such that multiple members of patients care team (physicians and nursing) are empowered to remove urinary catheters Creation of new system to remind team that urinary catheters are in place. Could be electronic in conjunction with I.T. department or handwritten reminders in chart. Would need interdisciplinary and administration buy-in to institute this potent QI step. Potential Steps Technology Preventive measures to decrease chance of demented patients from wandering. Assessment of wandering risk/impulsivity for patients with dementia. Use of bed alarms for those at high risk. Catheter attachment to leg rather than bed for patients at high risk Use of condom catheters for patients with dementia who have indication for catheter which does not require indwelling form Next Step Each small group reports back its potential solutions. The entire group then examines solutions to determine which are most feasible and have greatest potential to come up with an action plan for a QI project.