Active Disease (Tuberculosis)
advertisement

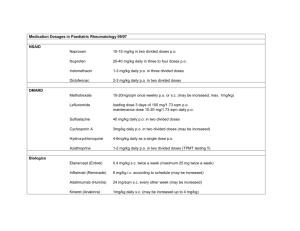
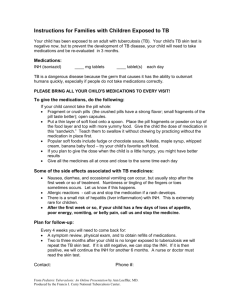
Clinical Pharmacy Tuberculosis is caused by M. tuberculosis, an aerobic, non–spore-forming bacillus that resists decolorization by acid alcohol after staining with basic fuchsin. For this reason, the organism is often referred to as an acid-fast bacillus (AFB). It is also different from other organisms in that it replicates slowly once every 24 hours instead of every 20 to 40 minutes as do some other organisms. M. tuberculosis thrives in environments where the oxygen tension is relatively high, such as the apices of the lung, the renal parenchyma, and the growing ends of bones. Mycobacterium tuberculosis is transmitted through the air by aerosolized droplet nuclei that are produced when a person with pulmonary or laryngeal TB coughs, sneezes, speaks, or sings. These droplet nuclei, which contain one to three M. tuberculosis organisms, are small enough (1–5 µg) to remain airborne for long periods of time and reach the alveoli within the lungs when inhaled. Tubercle bacilli are not transmitted on inanimate objects such as dishes, clothing, or bedding, and organisms deposited on skin or intact mucosa do not invade tissue. Latent Infection versus Active Disease A clear distinction should be made between latent infection and active disease (tuberculosis). Latent infection occurs when the tubercle bacilli are inhaled into the body. After inhalation, the droplet nuclei containing M. tuberculosis settle into the bronchioles and alveoli of the lungs. Development of infection in the lung is dependent on both the virulence of the organism and the inherent microbicidal ability of the alveolar macrophages. In the nonimmune (susceptible) host, the bacilli initially multiply unopposed by normal host defense mechanisms. The organisms are then taken into alveolar macrophages by phagocytosis and may remain viable, multiplying within the cells for extended periods of time. After 14 to 21 days of replication, the tubercle bacilli spread via the lymphatic system to the hilar lymph nodes and through the bloodstream to other organs. In most patients, active TB disease results from reactivation of a previously controlled latent infection, termed reactivation tuberculosis. Approximately 10% of individuals who acquire TB infection and do not receive therapy for the latent infection will develop active TB disease. The risk of developing active disease is highest in the first 2 years after infection, when half of the cases occur. The annual and lifetime risks for reactivation TB have been shown, however, to be directly related to the size of the induration on tuberculin skin testing. The risks for reactivation TB were greater in patients with larger induration diameters. The ability of the host to respond to M. tuberculosis may also be reduced by certain diseases such as diabetes mellitus, silicosis, chronic renal failure, and diseases or drugs associated with immunosuppression (e.g., HIV infection, antitumor necrosis factor-α agents, organ transplantation, corticosteroids, and other immunosuppressive agents). The overall goals for the treatment of TB are to cure the patient and to minimize the transmission of M. tuberculosis to others. The primary goals of antituberculosis chemotherapy are to kill the tubercle bacilli rapidly, prevent the emergence of drug resistance, and eliminate persistent bacilli from the host's tissues to prevent relapse. To accomplish these goals, it is essential that treatment be tailored and supervision be based on each patient's clinical and social circumstances (patient-centered care). Effective treatment of TB requires a substantial period (minimum 6 months) of intensive drug therapy with at least two bactericidal drugs that are active against the organism. The initial phase of treatment is crucial for preventing the emergence of resistance and for the ultimate outcome of TB therapy. Four basic regimens are recommended for the treatment of adult patients with TB caused by organisms that are known or presumed to be drug susceptible. Initial Phase Regimen 1 Interval and Doses (Minimal Drugs Duration) INH, RIF, PZA, EMB 7 days/week for 56 doses (8 weeks) OR 5 days/week for 40 doses (8 weeks)d Continuation Phase Interval and Dosesc (Minimal Drugs Duration) INH/RIF 7 days/week for 126 doses (18 weeks) OR 5 days/week for 90 doses (18 weeks)d INH/RIF Twice weekly for 36 doses (18 weeks) INH/RPT Once weekly for 18 doses (18 weeks) 2 3 4 INH, RIF, PZA, EMB 7 days/week for 14 doses (2 weeks) then twice weekly for 12 doses (6 weeks) OR 5 days/week for 10 doses (2 weeks)d then twice weekly for 12 doses (6 weeks) INH, RIF, PZA, EMB Three times weekly for 24 doses (8 weeks) INH, RIF, EMB 7 days/week for 56 doses (8 weeks) OR 5 days/week for 40 doses (8 weeks)d INF/RIF Twice weekly for 36 doses (18 weeks) INH/RPT Once weekly for 18 doses (18 weeks) INH/RIF Three times weekly for 54 doses (18 weeks) INH/RIF 7 days/week for 217 doses (31 weeks) OR 5 days/week for 155 doses (31 weeks)d INH/RIF Twice weekly for 62 doses (31 weeks) First line agents Isoniazid Rifampin Rifabutin Rifapentine Ethambutol Pyrazinamide Streptomycin Second-Line Agents Cycloserine Ethionamide Amikacin Capreomycin Para-aminosalicylic acid (PAS) Levofloxacin Moxifloxacin Gatifloxacin DOT is the practice of a health care provider or other responsible person observing as the patient ingests and swallows the TB medications. DOT is the preferred core management strategy for all patients with TB. The purpose of DOT is to ensure adherence to TB therapy. DOT not only ensures completion of therapy, but it may also reduce the risk of developing drug resistance. By improving these two factors, it also reduces the risk to the community. DOT can be administered with daily or two- to three-timesper-week regimens. It can be administered to patients in the office or clinic setting, or it be given at the patient's home, school, work, or other mutually agreed on place. Treatment of latent TB infection is effective in preventing active TB disease in persons who have positive tuberculin skin tests and in those at risk for reactivation of active TB. It is usually with daily INH alone for 6 months or RIF & INH for 3 months.