Determination of New or Established Patient
advertisement

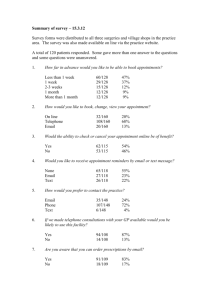
Improving the Productivity of Your Financial Operations Michael Holton Manager RSM McGladrey, Inc. 919-571-3266 Michael.Holton@RSMI.Com Subhead GOALS TODAY •Discuss the importance of systems in monitoring community health center efficiency and operations. •Identify system approaches and methodologies to assist in managing health center operations. •Develop measurement tools for key operational indicators. Registration/ Certification Patient Reception Patient Clinical Visit – Service Delivery Appointment Scheduling The Accounts Receivable Management and Collections Revenue Documentation & Coding Cycle Denied Claims Management Charge Processing/Check Out Claims & Patient Payments Processing Patient Statement & Claim Production EXAMPLE OF HEALTH CENTER OPERATIONS Patient Flow Intake/ Registration Medical Records Appointment Scheduling Business Office Follow Up/ Referral Patient Flow Patient Flow Triage Service Delivery IMPACT OF PATIENT FLOW/ACCESS ON PRODUCTIVITY • Before a physician sees a patient, the patient needs to register, have their vital signs taken, and have their charts pulled. • Make a commitment to improve efficiencies and remove bottlenecks in the process • How can we identify and improve on patient cycle time? IMPACT OF PATIENT FLOW/ACCESS ON PRODUCTIVITY • Evaluating the space needs and design layout of various areas, CHCs can identify areas for potential patient flow improvement. 1. Is the space designed to maximize the flow of patients, to move them through the health center as quickly and efficiently as possible? 2. Are there opportunities to relocate certain functions (registration, cashiering) to more central areas nearer to the front desk? 3. Other? • How is exam room utilization? Are there times when the exam rooms are full during the day, and other times when they are empty? What are your health center hours? For staff, providers, patients? What happens at lunch time? • EXAMPLE WORKFLOW OF INTAKE/REGISTRATION Patient Arrival Notification at Front Desk Data Collection Eligibility Verification New or Existing Patient Service Delivery MAIN COMPONENTS OF INTAKE/REGISTRATION • Notification at Front Desk - The front desk staff ensures that all patients who arrive for service identify themselves upon arrival. • Determination of New or Established Patient -The front desk staff identifies whether a patient is new to the center or is an existing patient (if this has not been done when the appointment was made). • Data Collection - New patients are referred to the patient registration staff for data collection activities and eligibility determination. • Eligibility Determination - Existing patients are referred to patient registration staff upon arrival for eligibility determination and data updating. IMPACT OF INTAKE/REGISTRATION ON PRODUCTIVITY • If the intake / registration process is not coordinated efficiently, then there are potential bottlenecks including: – Line for Patients Waiting to Notify Front Desk – Line of Patients Waiting for Registration – Line of Patients Waiting for Eligibility Determination • If patients are backed up at intake / registration, then there will be delays in getting patients into exam rooms. This problem could be when the health center first opens in the morning and at lunch time. • It is critical that there is a strong front desk to collect complete and accurate data. This data is used for a variety of important functions. SELECT PRODUCTIVITY MEASURES FOR INTAKE/REGISTRATION • Average Number of Patients Registered Per Hour Per Provider (new and established patients) • Average Waiting Time in Registration • Average Time to Complete an Intake (new and established patients) MAIN COMPONENTS OF APPOINTMENT SCHEDULING • Reminder Phone Calls - The front desk staff calls all patients the day or two before the appointment to confirm the date and time of the scheduled visit. • Check-in for Day’s Appointment - The front desk staff check the patient in and note the time the person arrived for his or her scheduled appointment. The person is put into the queue to be seen by the provider. The encounter form for the patient is printed and placed in the person’s medical chart. MAIN COMPONENTS OF APPOINTMENT SCHEDULING • Schedule Follow-up Appointments - The front desk staff identifies whether a patient is new to the center or is an existing patient (if this has not been done when the appointment was made). • Complete Lab / Specialty Referral Forms - The front desk staff completes any referral or insurance forms that are required. • Documentation and Notification of No-Shows - The front desk makes note of the patients who missed appointments and places follow-up phone calls to those patients to schedule a new appointment. IMPACT OF APPOINTMENT SCHEDULING ON PRODUCTIVITY • Due to the high no-show rate, it is important to efficiently manage appointment scheduling and ensure that there is a routine flow of patients for providers to see. CHC’s must account for walk-in rates when scheduling appointments. • Health centers should develop policies on how to block schedule their patients (e.g., standard time slots for different appointment types); what percentage of slots should be double and triple booked; and how walk-ins should be treated. • The distribution of new and established patient visits throughout the day must be well-thought out in order to maximize provider productivity and must be flexible and changed when appropriate. IMPACT OF APPOINTMENT SCHEDULING ON PRODUCTIVITY • Scheduling staff must make every attempt to make appointments as quickly as possible. The goal should be that the next available appointment which is convenient for the patient be scheduled. • On a regular basis, someone should review and monitor the scheduling of new patient visits, check that appointments are being double-booked as appropriate, and review the impact of any special requests on appointment scheduling. . IMPACT OF APPOINTMENT SCHEDULING ON PRODUCTIVITY • If volume permits, routine ancillary services should be available onsite and scheduling for ancillary services should be coordinated through a central scheduling function. • Automated scheduling systems should provide: Automatic reminders for standard visits (flu shots in the fall); The ability to discretely schedule different length visits and different physicians; Access to schedules for all physicians in all clinics (e.g., medicine, pediatrics, women’s health, HIV); and Access to scheduling for specialty appointments. SELECT PRODUCTIVITY MEASURES FOR APPOINTMENT SCHEDULING Percentage of Reminder Phone Calls / Postcards Completed (attempted and completed) • No-Show Rates By Provider (new and established patients) • Waiting Time from Check-In to Provider Visit (scheduled appointments and walk-ins) • Percentage of Walk-In Visits • Average Appointment Waiting Time (Urgent Medical Visit, Routine / Well Visit, and Non-Urgent Sick Visit) • Percentage of Unfilled Patient Slots COMPONENTS OF SERVICE DELIVERY Triage / Data Collection Exam Room If No Patient Waits Is Provider Ready? If Yes Patient Exam Business Office Ancillary Service IMPACT OF SERVICE DELIVERY ON PRODUCTIVITY • Patients must be in exam rooms when providers are ready and all necessary information must be available prior to the arrival of the provider (e.g., complete medical record). • Medical support staff must be focused on ensuring that each patient is efficiently managed throughout the service delivery process. • Each patient should be assigned a primary physician and the majority (>80%) of that patient’s visits to the health center should be with the same physician. • All providers should be educated in managed care. SELECT PRODUCTIVITY MEASURES FOR SERVICE DELIVERY • Average Number of Visits Per Provider (e.g., General and Internal Medicine, Family Practice, Pediatrics and Well-Baby, OB/GYN) • Number of Referrals / Primary Care Visit (specialty and ancillary) • Percentage of Eligible Patients with Up-to-Date Immunizations • Percentage of Patient No-Shows that are Evaluated to Determine Follow-Up • Provider Turnover Rate • Average Turn-Around Time for Test Results After Referral is Made (acute and non-acute) • Percentage of Abnormal Laboratory Results with Appropriate Follow-Up • Average Exam Room per Provider • Average Support (direct medical and administrative) per Provider COMPONENTS OF BUSINESS OFFICE/FOLLOW-UP Exam Room Business Office If Yes Appt. Sched. Is there F/U or Referral? If No Patient Exits IMPACT OF BUSINESS OFFICE ON PRODUCTIVITY • The business office should check each encounter form to ensure that the critical information is included (e.g., service documented, patient data complete, etc.), prior to claims submission. • Providers are responsible for accurate coding, thus they must correct any errors. • Claims filing and patient statements must be generated timely. SELECT PRODUCTIVITY MEASURES FOR BUSINESS OFFICE (Handout 1) • Percentage of Accurate and Complete Encounter Forms • Percentage of Rejected Bills • Percentage of Allowable Co-Pays / Sliding Fees Collected • Days in Accounts Receivable • Percentage of Bills Submitted Electronically COMPONENTS OF MEDICAL RECORDS The key issues in the area of medical records are as follows: • Incomplete Records • Compliance • Quality Assurance • Technology Opportunities • Availability IMPACT OF MEDICAL RECORDS ON PRODUCTIVITY • If providers complete the medical chart documentation immediately following the service delivery, then the information is more likely to be accurate than if this activity occurs weekly, or only once per day. • Medical records compliance includes: Diagnosis - The diagnosis must be included in the medical record and must be supported by the chart notes. Encounter Form - The CPT Code on the encounter form must be consistent with the diagnosis in the chart. Bill/Claim - The bill or claim submitted must be consistent with the encounter form. • Common missing data includes: – Results of Ancillary Services (e.g., lab tests) – Results of External Referrals for Service IMPACT OF MEDICAL RECORDS ON PRODUCTIVITY • CHCs should conduct regular internal chart audits, to monitor the quality of the care provided and to ensure that services provided meet the established clinical pathways. • Standard clinical quality indicators should be used • Compliance audits should be conducted regularly to ensure that the medical records, encounter forms and bills or claims are accurate and complete. IMPACT OF MEDICAL RECORDS ON PRODUCTIVITY • Using EMRs or Computer-Based Patient Records (CPR) can assist community health centers in improving the accuracy of medical data captured in the medical record, decrease the number of lost medical charts, and provide a powerful management tool. SELECT PRODUCTIVITY MEASURES FOR MEDICAL RECORDS • Percentage of Medical Records Available at Patient Visit (scheduled and walk-in) • Percentage of Incomplete Medical Records IDENTIFYING BOTTLENECKS • There are several ways in which CHCs can identify which operational area(s) require examination and possible reengineering. – Routinely Reviewing Productivity, Management, and Financial Data Quality – Conducting Internal Workflow Analyses – Administering Patient Satisfaction Surveys Assurance, IDENTIFYING BOTTLENECKS • Operations Committee - CHCs can bring together a small team of individuals including providers, administrators, and finance / billing staff in order to develop strategies aimed at addressing the operational issue(s). • Established by CEO, chaired by COO. • The team should identify issues and problems that would improve operations if resolved. • The team should propose recommendations to the CEO, identifying the lowest “hanging fruit” first, and then prioritizing other issues that involve more time and money. PROVIDER MONITORING • Monitoring providers can assist health centers in many areas, including the following: – Improving Productivity – Improving Quality of Care – Improving Patient Satisfaction – Providing Cost Efficient Care WHY MONITOR PROVIDERS? Competitive Environment • Health centers are facing increased competition for Medicaid and other insured populations. • Health center cost per visit is 30% - 50% greater than the cost per visit for private physicians and other competitors. • Health centers must understand the components of their costs and identify strategies to increase efficiency. • Health center costs can be 30% - 50% greater than the revenue streams for managed care and commercial patients. WHY MONITOR PROVIDERS? Optimize Efficiency Given limited funding resources for the uninsured and under-served, the more efficient a health center is in the delivery of services: The more services can be provided to these populations, and The greater the access to services. WHY MONITOR PROVIDERS? Optimize Efficiency • Health centers must optimize the efficiency and effectiveness with which services are delivered in all areas without compromising quality of care. • Optimum efficiency will vary based on the unique characteristics of individual health centers and their specific missions. CONCLUSION • Operational efficiency should focus on maximizing provider productivity. • Productivity is affected by all operations at a health center. • Systems should be developed and monitored for their impact on provider productivity. • Focus on opportunities!