Obesity
advertisement

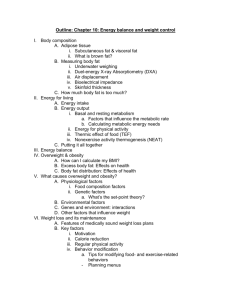
Aetiology and current evidence base for Weight Management Naveed Sattar Professor of Metabolic Medicine BHF GCRC, University of Glasgow & Hon Consultant Glasgow Royal Infirmary Outline How much obesity and where? What are the medical consequences? Mechanisms to metabolic disease – “ectopic fat” Some hard truths about wt loss – “why hard to lose…..” What can be done about it Rates UK, social class variations Worldwide Children UK rates since 1980 epidemic Lean, Gruer, Alberti, Sattar (2006) BMJ FORESIGHT forecast 2025 40% adults obese (2 in 5) By 2050 – Britain a mainly obese society Changing prevalence of obesity in the UK Prevalence of obesity (BMI > 30) in UK women 1994 - 2002 Which disease process is more closely linked to obesity? Type 2 diabetes – the microvascular burden at diagnosis a decade or so ago Retinopathy1 21% Nephropathy2 18% 20% Neuropathy1 Erectile dysfunction1 12% 1. UKPDS Group. Diabetes Res 1990; 13: 1–11. 2. The Hypertension in Diabetes Study Group. J Hypertens 1993; 11: 309–317. Yearly diabetes prevalence 1995-2005 Ontario Canada Lipscombe & Hux Lancet 2007 Summary on obesity rates On rise globally UK – ahead in Europe 40% obesity in ~17 year time Deprivation-linked Diabetes most closely associated T2DM in children Preventing Obesity is real target Less well know risks of Obesity? Medical Complications of Obesity Pulmonary disease abnormal function obstructive sleep apnea hypoventilation syndrome Stroke Idiopathic intracranial hypertension Cataracts Coronary heart disease Pancreatitis Nonalcoholic fatty liver disease steatosis steatohepatitis cirrhosis Gall bladder disease Cancer breast, uterus, cervix, prostate, kidney colon, esophagus, pancreas, liver Skin Gout Diabetes Dyslipidemia Hypertension Gynecologic abnormalities abnormal menses/ infertility polycystic ovarian syndrome Numerous pregnancy comps. Osteoarthritis Phlebitis venous stasis Populations more susceptible to adverse effects of weight gain? Hot spots for type 2 diabetes IDF Atlas 2003 The Middle-East – world diabetes hot-spot 18.7% 15.4% 16.8% 14.6% 13.4% DM prevalence for adults age 20-79 Age at diagnosis BMI Whites n=1557 57 30 South Asians n=210 46 28.7 Mukhopadhyay*, Forouhi*, Fisher, Kesson, Sattar. Diab Med 2005 Weight gain pulls trigger Risk of Type 2 diabetes 60 OVERWEIGHT OVERWEIGHT OBESE OBESE 50 40 30 20 10 0 < 23 23– 23.9 24– 24.9 25– 26.9 27– 28.9 BMI Chan JM et al. Diabetes Care 1994; 17: 961–969. 29– 30.9 31– 32.9 33– 34.9 > 35 Obesity to Diabetes – concept of ectopic fat…. Or “fat in wrong places” Most fat is healthy Who has most fat? Women Less CHD? Less diabetes? Why? More Subcutaneous fat Average BMI (kg / m^2) Men vs. Women – DM riskrisk? Men Women 40 35 30 30 40 50 60 70 80 Age at diagnosis of diabetes (years) Logue et al (In press) Diabetologia 90 ECTOPIC CONCEPT Consider 100kg man Total fat ~35kg 70-75% will be Subcutaneous 10-15% Visceral fat 10-15% elsewhere (E) Ethnicity Genes/ Programming Illness Subcutaneous GOOD But if storage capacity exceeded Or diminished These sites empty quicker 5% weight loss (100kg man) ~ 30% VF loss VF (0.5-6kg) E Ectopic fat Muscle and Liver Elsewhere Excess calories (increased intake or reduced energy expenditure) Subcutaneous stores overwhelmed (genes, ethnicity, ageing) Hepatic lipid accumulation muscle FAT ‘Spill over’ Insulin resistance pancreatic beta cell Perivascular fat Endothelial dysfunction Hyperglycaemia Fat accumulation in liver – when and what signs? oxidation Fat Glucose (protein) glucose Production (FBG) Fatty acids trigs DNL fat cells larger Liver Enzymes ALT GGT Sattar et al (2007) Diabetes Less insulin Liver fat ALT > AST GGT high Overweight Glucose high normal HDL-C often low vs. alcohol AST>ALT MCV high HDL-C higher than expected! Not necessarily overweight or high glucose Case MR RCN BMI 34 FBG 6.2 mmol/l ALT 67 (<50) AST 34 (<50) Trig 3.9 (<2.3mmol/l) HDL-c 0.9 (>1.0 mmol/l) IF AST starts to rise >0.8 of ALT (e.g. AST 80 vs ALT 85) – then think of NASH Keeping liver fat down? N=8 subjects with diabetes - Hypocaloric low fat diet (3%) Wt Glucose Insulin 86 to 78 kg 8.8 to 6.6 mmol/l 174 to 66 pmol/l Percent fat 12% to ~2% Petersen et al Diabetes. 2005 Research summary Diabetes unmasked by excess weight gain if family Hx DM, South Asian, at lower BMI weight leads to ectopic fat Ectopic fat makes organs insulin resistant Signs of excess ‘ectopic’ liver fat common Expanding visceral fat – i.e. waist line – a marker of ‘saturated’ subcutaneous fat store PART 2 – treatment of obesity thoughts on prevention Why are we in this mess? Foresight Simple surely “Too much in, not enough out” Moving on from Foresight Understanding obesity hampered by inaccurate data on energy intake and expenditure – Heavier people have higher energy expenditure and intake – Almost all the increase in weight in US can be attributed to Total Energy Intake (rather than PA) (500kcal adults, 300kcal children) Children x Adults Data from Swinburn et al 2009 Heavier people have higher energy expenditure, and thus intake Implications People with lower BMIs need substantially less food energy to maintain weight To achieve and maintain “healthy” weight, obese individuals need big sustained reduction in energy intake or huge increases in PA Are we lazier and greedier than prior generations? What did foresight conclude? People in the UK are not more glutinous that previous generations, and their biology is not different But major changes in society, work patterns, transport, food production and sales Pace of technology exceeding human evolution “What is provided is what is eaten So what is provided has to change” Lean, Gruer, Alberti, Sattar (2006) BMJ Recommended for 5-10yr olds. Contains 40g of sugar per 100g 174 calories per bowl Salt also is its third biggest ingredient The label boasts virtually fat free •Contains Artificial sweeteners 108 calories and 9.6g of sugar per 100g Other facts about food changes Cost of fruit & veg: Sugar and fat cost: Overproducing food 80% of daily salt intake via processed foods – cereals etc Products designed to be tastier Sugar, fat, salt 1978 Crisp packet once per week, if lucky Perhaps one biscuit per day, if lucky No coke, yogurts, fast foods except chip shops All meals at home cooked by mum Walked everywhere, played outside all time No computer, etc Much more complex FORESIGHT The full obesity system map with thematic clusters Primary driver for epidemic Overeating or under activity? Jeffery RW, Harnack LJ. Evidence Implicating Eating as a Primary Driver for the Obesity Epidemic. Diabetes 2007;56:2673-6 Simple considerations We all love food – even…. Food more plentiful Increasing density, less time, consume fast Sugary drinks abound How fast can you eat 200 calories? How fast can you burn 200 calories? A moment on the lips…. 1949 “…an epidemic; under the right economic & social circumstances, obesity from overeating will be a dominant nutritional problem.” Ancel Keys Government Leadership People and the public (you and me) Public education little effect on behaviour sets the scene, increase awareness, helps support for action recognise inequalities Public sector work (Schools, prisons, hospital ) Food industry (the Five Ps product, promotion, portion size, packaging, pricing) Re-formulations and labelling; Portions and promotions Advertising and marketing Huge Tin of Roses £4 Food, retail and catering Industry “Increase healthy options” “increase range of portion sizes” “promoting fruits and vegetables” Food, retail and catering Industry- HALF A STORY! “Increase healthy options” “increase range of portion sizes” “promoting fruits and vegetables DECREASE LESS HEALTHY OPTIONS DECREASE LARGE PORTION SIZES DECREASE CONFECTIONERY OPTIONS At very least …?Level playing field……. Reality: incredibly hard to lose AND sustain weight loss Very hard to lose weight by physical activity alone “Most do not wish to be overweight” Up to half who are obese will not lose weight by any medical method Lean, Gruer, Alberti, Sattar (2006) BMJ Appetite/satiety signals impaired when obese Stanley S et al. Physiol Rev 2005; 85: 1131 Obesity – public health issue – prevention must be priority Limit “energy dense” foods sat fat, refined sugar Fruit & Veg. fibre…. Snacking – eat more fruit…. Chew etc Less smoothies / fruit juices Treating obesity? Systematic reviews - SIGN Dietary and lifestyle up to 5kg (2-4 yrs) Drugs 5-10kg (1-2 yrs) Surgery ~25-75kg (2-4 years) 1. Cut sugary drinks – Asked how many spoonfuls of sugar in x,y, z etc • Coca-Cola • Red Bull • Irn Bru “Healthy drinks?” • Copella Apple Juice • Frijj Chocolate Milk Shake • Lucozade Orange • Pom Wonderful • Ribena • Innocent Smoothie • Tropicana Orange Tea spoons of sugar Drinks sugar content not understood • People slightly overestimated the amount of sugar in carbonated drinks, • BUT significantly underestimated sugar levels in – – – – – milkshake, a smoothie, a leading sports drink and a variety of fruit juices – by as much as 17 tea spoons for one fruit juice drink • An example of lack of clarity / miss-selling? • Paper being written up…….. In clinical practice? Refer to where? NHS not alone Ask – not all patients ready to discuss weight Assess – BMI still best (accuracy – more data on longer associations) Advice – health service may not be best place to improve weight Susan Jebb (Foresight report) Weight watchers beats GP practice (Jebb et al Lancet 2011 RCT, 722 patients) WW - good for wider use Referral to WW with regular weighing, advice about diet and activity, motivational sessions and group support can offer early intervention for weigh management in overweight and obese that can be delivered at large scale What do we tell our patients Body weight 50-100kcal per day for weight maintenance Successes 1. Sustained weight, no increase. Obese 2. Minor weight loss with dietary change to reduce risk of complications. Overweight Normal 3. Weight normalisation: rare Treatment strategies Years of management or intermittent monitoring Adapted from Rössner, 1992 by U.S. Institute of Medicine, 1995. Graded reductions in energy intake & effect over time Retrain your taste buds gradually – goal setting 1st change 2nd change 3rd change Final summary Rates – epidemic – 40% by 2025 Risks – plentiful – all body systems, QOL Research – ectopic fat many effects Reality – prevention must be key as once obese, reversal v. hard by any medical method Patients – emphasise small and sustainable changes…intake and activity…achieve and extend if needed.