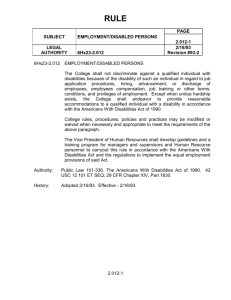
Prevalence of people with a Learning Disability
advertisement

NHS Western Isles Learning Disabilities Collaborative Learning Disabilities Change Programme (Equally Well) Funding End report August 2013 Please note this document has embedded files and hyperlinks to relevant material – therefore is best viewed on a computer 1 Learning Disabilities Change Programme (Equally Well) Funding End Report August 2013 Prepared by; Kathryn MacIver, Learning Disabilities Collaborative Programme Manager NHS Western Isles 37 South Beach Street Stornoway Isle of Lewis HS1 2BB M – 07891951920 http://www.wihb.scot.nhs.uk/ Front Cover Stand Up for Yourself Advocacy Group members meeting senior executives and managers of NHSWI Health Board. 2 Contents EXECUTIVE SUMMARY ...................................................................................................... 5 INTRODUCTION ................................................................................................................ 6 MAIN REPORT .................................................................................................................. 7 LEGISLATIVE AND POLICY CONTEXT ....................................................................................................................... 7 LEARNING DISABILITIES DEFINITION: ..................................................................................................................... 8 PREVALENCE OF PEOPLE WITH A LEARNING DISABILITY .............................................................................................. 9 LOCAL DEMOGRAPHIC ....................................................................................................................................... 9 HEALTH NEEDS ................................................................................................................................................ 9 MENTAL HEALTH CONDITIONS ............................................................................................................................. 9 DEMENTIA .................................................................................................................................................... 10 EPILEPSY ...................................................................................................................................................... 10 COMMUNICATION NEEDS ................................................................................................................................. 10 HEALTH INEQUALITIES EXPERIENCED BY PEOPLE WITH AN LD.................................................................................... 11 Reasonable adjustments to Practice ............................................................................................................ 11 CAPACITY AND VALID CONSENT WHEN RESPONDING TO PEOPLE WITH A LEARNING DISABILITY ........................................... 12 BARRIERS TO HEALTH CARE .............................................................................................................................. 12 PROJECT OUTCOMES ...................................................................................................... 12 CHANGE MODEL ............................................................................................................. 13 PRODUCT DEVELOPMENT AND DELIVERY ............................................................................................................. 15 LOCAL MODEL OF COLLABORATION .................................................................................................................... 15 INPUT AND INVOLVEMENT FROM CLIENTS WITH A LEARNING DISABILITY....................................................................... 17 Advocacy Presentation – .............................................................................................................................. 17 SUMMARY OF LOCAL ENHANCED SERVICE ................................................................................................. 20 HEALTH SCREENING TEMPLATE .......................................................................................................................... 20 AWARENESS TRAINING .................................................................................................................................... 21 LD COLLABORATIVE TRAINING EVENTS AND ATTENDANCE ....................................................................................... 21 Learn Pro Modules - transcribed with kind permission from NHS Lothian................................................... 23 AWI Website Legislation DVD development with Nicola Smith, Cairn Management Trust. ........................ 23 LD Services Website http://www.wihb.scot.nhs.uk/LD/index.html..................................................... 24 Learning Disability Link Role ........................................................................................................................ 25 Communication Training .............................................................................................................................. 26 HEALTH PROMOTION POLICY ............................................................................................................................ 26 DENTAL TREATMENT ....................................................................................................................................... 27 ADMISSION/DISCHARGE POLICY ........................................................................................................................ 28 HEALTH IMPROVEMENT WORK.......................................................................................................................... 28 DISTAT – DISTRESS ASSESSMENT TOOL – ............................................................................................................. 29 HTTP://DISDATTOOL.WORDPRESS.COM/ABOUT/ .................................................................................................. 29 ADAPTED NUTRITIONAL SCORING SYSTEM ............................................................................................................ 29 SENSORY INTEGRATION TRAINING ...................................................................................................................... 29 HEALTHY EATING , HEALTHY LIVING.................................................................................................................... 30 3 PROJECT PRODUCT TABLE............................................................................................... 30 FINANCIAL OVERVIEW ................................................... ERROR! BOOKMARK NOT DEFINED. REFERENCES AND BIBLIOGRAPHY ................................................................................... 30 BIBLIOGRAPHY ............................................................................................................... 32 APPENDICES ................................................................................................................... 33 APPENDIX 1 – PRIMARY CARE WORK .................................................................................................................. 33 APPENDIX 2 LD LINK ROLE DESCRIPTOR .............................................................................................................. 36 HEALTH PROMOTION POLICY APPENDIX 3 ........................................................................................................... 37 HOSPITAL POLICY DRAFT APPENDIX 4 ................................................................................................................ 38 ADAPTED NUTRITIONAL SCORING SYSTEM - APPENDIX 5 ........................................................................................ 38 4 Executive Summary NHS Western Isles was awarded funding from the Learning Disabilities Change Programme (Equally Well) Funding to implement a programme to address the health inequalities and target health promotion activity for people with learning disabilities. During 2012/13 additional funding was made available based on the success of the outcomes over the first two years of the project. This paper is the final report and will be complimented by the formal evaluation once completed. This will be undertaken by Glasgow University on behalf of the Scottish Learning Disabilities Observatory. Based on the Improvement Scotland model for Long Term Conditions, Mental Health and 18 weeks RTT, the Western Isles Learning Disability Collaborative has been the first project in Scotland to use this model aimed at addressing health inequalities for people with Learning Disabilities. The principle that people with Learning Disabilities have equal rights to others when accessing health care underpinned the work of the project. To achieve this the aims of the project were to influence managers and clinicians who provide general health care services to recognise, prepare and implement the special measures that would be needed to address the unique needs of people with a learning disability: The right to make informed choices affecting their care, to have information and communications needs met, to put in place measures that negate inequality in health care, regular health reviews for example; means of tracking referrals to specialist health care in hospitals; signage to direct people with a learning disability to the correct department. 5 The project involved people with a learning disability through the ‘Stand Up for Yourself Advocacy Group’ from the beginning and this culminated in the group making a power point presentation to Board Executives and Senior Hospital Managers and Heads of Departments, about their hospital experiences and how hospital services could be improved based on their experiences. They have now received direct funding from the project to enable them to train as communication trainers based on the Renfrewshire model ‘The Good Life’ and are in the process of development. The recommendations from the Fatal Accident Enquiries into the deaths of James Mauchland (2003) and Roderick Donnet (2007) were key influences in the design and objective setting of the project. Work is now complete and rolled out across NHS Western Isles to integrate an electronic tri-annual health review in embedded template across all GP practices. The option to now track patients linked to SCI Gateway/Topas and EMIS is complete – with a substantial expansion to the ability to provide alerts to services regarding patients' access/sensory/mobility and representation needs in advance of any appointment is now in place. The Health Assessment Tool using EMIS has been read coded and will populate GP records. Training was provided for GPs and practice staff in February 2012. A national recommendation has indicated the benefits of appointing a Learning Disabilities Coordinator in hospitals. Due to the low ratio of people with a learning disability and the dispersed population across all our islands, it was thought that this would not be the best model. Instead Learning Disability Link Staff have been identified in all GP practices and in all hospital departments, 34 people across the services of NHS Western Isles. The predicted benefit of this approach is that no matter what service people with a learning disability need to use locally there will be at least one member of staff trained in the particular skills needed to meet their needs. It is also anticipated that these staff members will also act as a source of advice and support to their colleagues. Introduction The full 3 years funding was allocated from the Scottish Government based on implementing the following recommendations; Vulnerable Groups: access to services 52. NHS Boards should target health promotion and health improvement action better for people with learning disabilities and others who may need support with access to information, in line with statutory disability requirements. 53. The Government should lead development of a framework for regular health assessments for people with learning disabilities in all NHS Board areas. 54. Each NHS Board should have a designated senior post responsible for ensuring that people with learning disabilities receive fair and equitable treatment from health services. There were two members of staff employed specifically for The Learning Disabilities Programme Learning Disabilities Collaborative Programme Manager and Learning Disabilities Collaborative Programme Administrator. The project sits within the Public Health and Health Strategy Directorate Planning and Development Department. The Depute Head of Planning , to whom the project reports, has the strategic lead. 6 National networking is with the Scottish Government, Health Inequalities quarterly meetings – enabling links with the Scottish Government and special and local Health Boards for exchange of ideas, products and legislative developments. This has proved an invaluable resource which has directly impacted on successful outcomes. The programmes links with multi-agency Learning Disabilities services has been through the local Learning Disabilities Partnership with 24 representative organisations and groups across primary and secondary care, Local Council Education and Housing and many third sector agencies. Attendance at the Learning Disabilities Nurses Team meeting in Tarbert has been on a regular basis with individual project joint work streams being advanced in less formal meetings. Communication of progress to staff has been structured through articles in the Slainte magazine and through the link role structure. Main Report Legislative and Policy Context The legislative and policy environment is aimed at protecting people with disabilities, including those with a learning disability from direct discrimination by promoting and supporting their rights to enjoy equal opportunities in all aspects of life for example employment, education and health care. This is supported by the legislative framework and focused on people with a learning disability. Adult Support and Protection (Scotland) Act, (2007) Mental Health, Care and Treatment Act (Scotland), (2003) The Equality Act, (2010) Adult with Incapacity(Scotland) Act, (2000) The Same as You (Scottish Executive, 2000) has identifies seven key principles as central to their care. People with learning disabilities should be: Valued Treated as individuals Asked about what they need and involved in choices Given the health and support to do what they want to do Able to get local services just like everyone else Able to access specialist services when they need them Able to have services which take account of age, ability and needs. These principles underpin the findings and recommendations of subsequent government reports. The aim is to ensure that account is taken of the human, civil and legal rights of people with a 7 learning disability and that these are embedded locally in the responses of each of the NHS Health Boards at a strategic and operational level. The national reports also call for a proactive rather than a reactive approach to the health needs of people with learning disabilities, with organisations working together in order to support a holistic, person centered approach to health care( Keys to life 2013) The focus is on sustainable change within generic health care services. All nurses and midwives access the different levels and locations of health care provision have a key role to play. The Scottish Government document, Promoting Health, Supporting Inclusion, (2002), states that with the changing profile of general and learning disability population will have an impact on all services, including health. Innovative approaches and models of service delivery that take account of their health care needs have been lacking in the past... must change to improve access to health and co ordination of the care journey. These approaches will challenge traditional boundaries and ways of working. This is further substantiated by the Fatal Accident Inquiries and the Mencap document ‘Death by Indifference’ with the subsequent ombudsman review – the later document 74 lives and Counting, (2012) supports the conclusion that omissions and gaps in generic service delivery are linked to treatable and avoidable deaths in people with a learning disability. The Best Practice Statement (2006) for promoting access to healthcare for people with a learning disability identifies three principles which underpin the work; ‘The health needs of people with a learning disability are greater and more complex and often present differently to those from the general population. People with a learning disability are more likely than the rest of the population to have impairment to communication and therefore require special consideration. People with a Learning Disability have a right to access health services and these should be provided within the current legislative framework and in a way which upholds the principles of inclusion and respect, and conforms to professional standards.’ Learning Disabilities Definition: The definition of learning disabilities applied to this health needs assessment is taken from ‘The same as you? A review of services for people with learning disabilities’ (Scottish Executive 2000) and is as follows: People with learning disabilities have a significant, lifelong condition that started before adulthood, that affected their development and means they need help to: understand information; learn new skills; and ability to cope independently. This definition has been adopted by a range of policy documents developed by the Scottish Government specific to those with learning disabilities, and is widely recognised and understood. Prevalence of people with Autism Spectrum Disorders Prevalence estimates in the Public Health Institute of Scotland’s (PHIS) ASD Needs Assessment Report suggested 60 in every 10,000 people are affected by ASD. More recent Autism Strategy 8 (2012)for Scotland suggest that a rate of around 1 in 100 is currently the best estimate of the prevalence in children and adults. Prevalence of people with a Learning Disability The Same as you (2000) and the Health Needs Assessment (2004) refer to the following prevalence rates when estimating the number of people with a learning disability living in Scotland. It is estimated that: 120,000 people with a learning disability in Scotland. 20 people in every 1,000 have a mild or moderate learning disability; and 3 to 4 people for every 1,000 have a profound or multiple disabilities. This prevalence figure would indicate approx 604 people with a learning disability within the Western Isles based on a general population of 26,000. The future projection is a year on year increase of 1 - 2% per annum over the next 10 years due in part to improved antenatal outcomes for premature children. More boys are born with learning disabilities than girls – this may be due to some inherited conditions being linked with the male gender. Local Demographic There are currently 215 people on the LD register held by North Harris Medical Practice. This is a voluntary register. Please note locally that although some children are reflected in the numbers in general - unless there is a firm diagnosis most children will be identified within the Individual Education programme structure within education and will at times only transfer to the LD register at the time of transition from education. There are different inclusions criteria for IEP and the Learning Disability register. Health Needs Life expectancy is one of the key public health measures to determine the health of the population. Life expectancy for people with a learning disability while improving is still lower by 10 – 20 years than the rest of the population being shortest for people with a learning disability who are least able. While Scottish public health strategies are aimed at tackling firstly cancer, then ischemic heart disease and thirdly cardiovascular disease. For people with a learning disability the leading cause of death is respiratory disease related to pneumonia and aspiration, posture, swallowing and feeding problems and gastro-oesophageal reflux disorder. Studies show congenital rather than ischemic heart disease and cancer being the lowest ranked cause of death – the types of cancer most commonly experienced differ from the general population. In particular people with a learning disability have reduced rates of lung, prostate and urinary tract malignancies but increased oesophagus, stomach and gall bladder malignancies. Mental Health conditions Affect 40 – 50% of people with a learning disability. Prevalence of psychiatric disorders is 36% in children with a learning disability compared to 8% among those without. Children with learning disabilities account for 14% of all British children with a psychiatric disorder Emerson (2007) This is also especially marked for people with Autistic Spectrum Disorder, ADHD and conduct /behavioural disorders. 10 – 15% of people with a Learning disability will present with challenging behaviour(aggression, destruction, self-injury) there is evidence to show that the prevalence of for 9 schizophrenia in people with a learning disability is three times greater than the general population. Incidences of anxiety and depression are also higher. Dementia Prevalence is higher at 22% compared to 6% in the general population aged over 65 and is associated with a range of potentially challenging behaviours and health problems. Onset can be at a younger age eg 30 – 40 for Down ’s syndrome patients. Epilepsy Prevalence rate identified as at least twenty times more within the population with a learning disability. Often linked with more complex epilepsy and at times resistance to drug therapy, which in turn can have a negative impact on quality of life and mortality. Some other disorders/conditions have increased importance – due to conditions generally being not recognised, not treated and not know about – examples include: Choking/aspiration risk Impacted cerumen Oral and dental health Nutrition/Malnutrition Reflux Disorder Constipation Sleep disorders Sensory Needs - Visual Impairment/cerebral visual impairment and hearing impairments Injuries accidents and falls/mobility, balance, coordination, footcare Haematological disorders Sexual Health Adverse experiences and abuse Metabolic and endocrine disorders – both general and attributing condition specific Osteoporosis Poly-pharmacy For the purpose of this report detailed analysis has not been completed on all conditions, for further information please refer to the Scottish Health Needs Assessment Report – People with Learning Disabilities in Scotland(2004) Communication needs 10 Up to 80% of people with a Learning Disability will have communication barriers and needs (Same as You, 2000) The range includes problems with expression, comprehension and pragmatic communication in social situations. Problems with communication may be related to problem behaviours and can be a significant barrier to accessing healthcare. Health Inequalities Experienced by People with an LD Health Inequalities: Inequity in access to health care services and health status between different and discrete populations, for example people living in defined geographical areas, different ethnic communities, or people with learning disabilities. These populations may experience multiple factors that result in health inequalities. Examples of health inequalities include differing access to health information access to mainstream health care chances of employment Emerson (2010) identifies that health inequalities faced by people with a learning disability start early in life and result, to an extent, from barriers they face in accessing timely, appropriate and effective health care (Michael J, 2008) Reasonable adjustments to Practice This phrase is used to describe actions taken by health care professionals and others which make access to their service for people with a learning disability easier. Examples are longer appointment times, information in an easy to read format, familiarising individuals to the steps involved in a specific procedure before it happens, quiet waiting areas and providing care (where feasible) in an environment that suits the individual and the removal of any physical barriers. Valid consent: The phrase valid consent is used as it suggests that gaining consent is not only about providing information in a manner which allows an individual to make an informed choice, but that consent is sought from someone with the appropriate authority to make a decision. This may be a family carer who has guardianship or a health professional. Being aware - a lack of awareness about the needs of people with a learning disability and whether an individual had a learning disability was seen to have the potential to lead to wasted appointment times, unnecessary medical appointments which could lead to distress, ineffective consultations, or failure to attend appointments. 11 Communication - knowing how an individual communicates and their level of comprehension was identified as key to engaging people with a learning disability in the health care they may require. Communication, capacity and valid consent The health needs assessment process highlight the importance of understanding the interconnected nature of communication, capacity and valid consent when responding to people with a learning disability. Health professionals have a key role in ensuring people with a learning disability are able to both give and receive information to the best of their ability so that they are able to make decisions. It would seem that this does not always happen. Education and resources - The need for more awareness raising and education for health care professionals and those from other sectors, as to the health needs of people with a learning disability and the reasonable adjustments Capacity and valid consent when responding to people with a learning disability Health professionals have a key role in ensuring people with a learning disability are able to both give and receive information to the best of their ability so that they are able to make decisions. It would seem that this does not always happen. Barriers to Health Care Scarcity of services physical barriers to access failure to make ‘reasonable adjustments’ in light of literacy and communication difficulties experienced by many people with a learning disability Variability in the availability of interpreters/communication support ‘diagnostic overshadowing’ (symptoms of ill-health being attributed to either a mental health/behavioural problem or as being inherent in the person’s learning disability) Attitudes among healthcare staff. Project Outcomes Projects baseline outcomes – highlighted in initial proposal document. Specific outcomes will be: 12 • Key Staff in Primary and Secondary Care will have received training on the management and specific needs of people with learning disabilities and autistic spectrum disorder. • A single shared assessment will be in place supported with local protocols for the management of health screening, planned and emergency admission to hospital and discharge from hospital or community care. • Each person will be given the opportunity to be included in a register in their local general practice with an electronic record that will be used for call and recall for health screening and which will be used as a shared record for managing their care. • A range of health promotion and health care information in different media, including film / video, electronic and print, will be available and which will cover a number of key health subjects and specific service information. • A quality assurance and governance system will be in place for the continuous monitoring of services and care systems. • Communications systems and processes will be in place that ensures the timely transfer of information between primary and secondary care and across services. • A health screening programme will be fully implemented that offers regular health reviews for each person with protocols for onward referral to specialist health services for any detected health problems. • People will have the opportunity for planned access to dental care for regular examination and treatment. Please bear in mind that during the initial proposal and the actual setting up of the project there had been relevant organisational/ role changes which had accounted for some of these objectives being met elsewhere. In this situation the objectives were fully discussed and adapted with line management approval. Change Model 13 Monitor Knowledge Use Select, Tailor, Implement Interventions Assess Barriers/ Supports to Knowledge Use KNOWLEDGE CREATION Knowledge Inquiry Synthesis Adapt Knowledge to Local Context Evaluate Outcomes Products/ Tools Sustain Knowledge Use Identify Problem Knowledge to Action Graham et al 2006 Identify, Review, Select Knowledge ACTION CYCLE APPLICATION You will see that this Knowledge to Action Process fits with the steps of evidence-informed public health . As a front-line public health worker, manager or policy-maker, you will start with the box at the bottom of the diagram. In other words, you will first identify a problem, and identify, review and select knowledge, and then (moving clockwise in the outer circle) you will adapt the knowledge to the local context, consider barriers to its implementation, select interventions, monitor their use and evaluate outcomes. The final stage feeds back to where we started: the identification of problems 14 Product Development and Delivery Extensive collaboration has taken place across the duration of the project. Few aspects have been progressed in a formal manner such as structured formal meetings – smaller relevant groups according to each area of action - in closely accessible venues for staff to minimise disruption to their job delivery have proved more effective. Local Model of collaboration Strategic Lead and Executive Board Operational Managers Frontline Services Learning Disabilities Collaborative Programme People with a learning Disability The developing model which seems to reflect the approach in the Western Isles NHS best is detailed above. The focus of developing change by having input from clients with a learning disability has enabled staff to relate to and incorporate local clients needs in project planning. The work of the project to extend this message alongside the training package in place has impacted greatly on how effectively the issues have been received and developed. In identifying frontline staff specifically in both training and link role the adaptations to care delivery will be both of a practical and accessible form for direct positive impact on patients care delivery. The support of operational managers in releasing staff for training and input in policy setting and fatal accident reviews has been essential to the success of the work to date. The further identification by both strategic and executive leads of the necessary developments to incorporate change into the health delivery structure and support of continued learning will enable further sustainability of the changes identified throughout this document and the projects work. Throughout the time of the project there is a tangible change in the involvement of staff and local discussion of the issues surrounding how clients with a learning disability access health services and an improved understanding of their needs when they do. The project has enabled staff to identify with issues that previously they may just have felt and unease or dissatisfaction with care delivery, into areas of empowered positive change to improve care delivery. Staff report feeling more comfortable and supported with their role as advocates for clients with learning disabilities. 15 The project staff has been tasked to work with frontline general staff in Primary Care, Secondary Care and Dental Services. The aim was to influence other groups of staff – frontline services, Secondary and Primary Care and community staff alongside encompassing interagency working. The focus has been on improving peoples understanding of their responsibilities to deliver services to people with LD and to meet their general health needs. Starting with the basic principles these staff have been trained in the possible communication needs of people with LD. (Mauchland, Donnett 2003) The project was structured around key objectives and a detailed Project Plan evolved, after discussion with service leads, senior managers, primary care staff, local LDP (Learning Disabilities Partnership) and service users. People with LD have been involved in the process throughout and the project has developed a mutually rewarding relationship with the ‘Stand Up for Yourself ’ Self Advocacy group Western Isles. It was through this process that priorities were identified and resources allocated. Resources in this regard mean dedication of staff time and the funding of training alongside purchase of materials and equipment. Tracking/Identification of patients with a learning disability/Autism across the acute healthcare pathway SCI – Gateway is the programme used for referrals between primary and secondary care – as well as being able to identify LD and Autism data on referral form now an additional information tab allows for ease of transfer of information about patients additional needs: • Carer’s details • Literacy issues • Sensory needs • Mobility/access requirements • Learning Disability /Autism • Need for representation/Advocacy/Chaperone • Power of Attorney • Guardianship – Finance and Health • Identification of incapacity treatment plan being in place in the community Once completed these details will appear on the front page of the referral letter aiding the transfer of essential information between service providers to allow for improved consistency, quality and adaptations to be met and planned for according to individual patients need. It can be noted extensively throughout the report that the impact zones for the project products benefit a much wider group of patients needs such as sensory impairment, disability, dementia, brain injury and stroke, people with supported educational needs and also impacts across the age range. TOPAS is the data management system for transfer of information to Medical Records for requesting appointments at clinics. Initial uploading of a Learning Disability/Autism flag has been undertaken by the North Harris Medical Practice – who safeguard the local Learning Disability Register. This will be edited and adapted as changes to the register occur. 16 The SCI- Gateway is the portal also for SCI-discharge so completing the cycle of local information transfer between referral to admission and in patients stay and discharge into the community once more. SCI – discharge is completed at point of patients discharge into the community therefore highlighting patients discharge needs instantly to community services. Further work has been completed within the EMIS system for Health Screening needs – please refer to the section on Health Screening. Future focus may include identifying connections between further healthcare data systems eg dental, podiatry, ophthalmology, physiotherapy etc. The variation of data bases across the healthcare system restricted the practical scope of impact in the full identification across all pathways. One area of difficulty has been the work surrounding the Single Shared Assessment . There has been much work done on incorporating a structure through the TYNDALE system which is now to be replaced. There is interagency working towards this end and it is not within the remit or scope of the project to resolve this issue. However, the framework for TOPAS and health screening may be incorporated to some level whenever the SSA is in place. Input and involvement from clients with a learning disability. Clients from the ‘Stand up for Yourself’ Advocacy Group Western Isles have been involved in the project from the beginning. The project initially approached the group to inform the gathering of 15 adults with Learning Disabilities, about the areas to be developed within the project. The group wished to participate somehow. They spent several weeks discussing their views about accessing health care services locally and decided they wished to present their viewpoints to staff. The quality of the material was superb – dealing with confidentiality, going to theatre, Accident and Emergency, Doctors, signage and requirement for materials to be accessible in easy read format. Advocacy Presentation – Advocacy_presentati on_health_access.ppt A pre-authorised walk around the hospital followed the presentation. 12 clients from the “Stand up for yourself” group accompanied by the LD project team; Equality and Diversity Team and Advocacy Western Isles staff members. The areas visited were Erisort Ward, Outpatients Dept, A&E and the XRay Dept. Points raised: The group expressed difficulty in interpreting what some signage meant within the hospital. eg. Mixed Speciality Signage was felt to be hung at a level that was too high to be easily noticed and read. Main signage board at reception: 17 Bigger print required as it is difficult to read the print on the board. Colour coded signage to be used for orientation throughout the hospital. Eg green on a sign would always refer to surgical. Direction arrows to be included would help orientation Increased frequency of signage required – the group explained this as frequently forgetting what was read and needing another point of reference further down a route. Using maps with reference points and colour coding with varied “you are here” points on the walls. Patient facing information would be easier to read if it was in larger font and has a border around the page. This includes the Emergency notices and toilet signage. This presentation has been delivered by the group three times with very good staff, managerial and board representation and opening support provided by the Chief Executive, Gordon Jamieson. Further funding from the programme has enabled the Group to go on and develop themselves as Communication Trainers for local businesses, Health and Council staff. This has been based on the North Dunbartonshire model of communication training delivery by the ‘Good life Group’ – collaboration and joint working is adapting the programme for suitable interpretation into practice for the group based in the Western Isles. I believe they are keen to use the medium of drama to get the message of their support needs across to their audiences. In the future will cover costs by charging local businesses for the training . The Stand up for yourself , Self Advocacy Group have had three members who have been directly involved in the national consultation for the review of the ‘Same as You’ and some are now preparing to travel to Edinburgh for the Launch of the end product - ‘The Keys to Life’ the Learning Disability Strategy for Scotland, in June 2013. The AGM discussed the enormous positive impact these contacts and work outputs have had on the group members – both in up skilling and confidence building to encouraging their voice to be heard at a local and national level. The most reflective impact change is based around people who understand the issues best – people with a learning disability. The group have also been involved in reviewing and adapting and easy read letter, the easy read xray leaflets, and the easy read medicinal information leaflets (still in progress) X – ray form http://www.wihb.scot.nhs.uk/LD/easyread/Easy%20Read%20xray.pdf Ultrasound Scan http://www.wihb.scot.nhs.uk/LD/easyread/Easy%20Read%20ultrasound.pdf CT scan http://www.wihb.scot.nhs.uk/LD/easyread/Easy%20Read%20CT%20+%20C.pdf It was highlighted by the local group, to date that they generally receive no information/letters they can interpret for themselves from Healthcare or Local Council – they have to rely on a third party interpretation. The feedback was that they would love to receive a letter such as shown for appointments. 18 The local adaptations for mailing have yet to be met within the systems available to Medical Records. An additional Local enhanced service was completed for the year September 2011 – 2012 These are non-recurrent funding allocation. Primary Care Work for Learning Disability Collaborative As an area traditionally managed by specialist secondary care staff in institutions, LD has not always been covered to great depth or breadth by medical schools nor traditional general practice training. Working with local GPs the collaborative established that Primary Care physicians felt ill-equipped to manage patients with learning disabilities. As such it was felt that the first stage of work would aim to raise awareness, educate and support staff. Being a small health board, the Western Isles does not have the specialist staff that others boards. We are fortunate enough to have a team of two LD nurses covering seven separate islands over the distance of some 160 miles . The Local Enhanced Service helped identify primary care staff with an interest. They were then approached to become link personnel. Rather than relying on a small number of specialist staff the collaborative helped establish a larger group of staff with an interest who could develop their skills and knowledge over time and champion the cause throughout different areas of the organisation. The LES encouraged practices to code patients with LD appropriately and consistently. The practices were provided with an electronic template installed within their computer system. The training included sessions on completion of the template at the already established LD reviews. The project aims to capture this data and help practices and the Board use the information they have gathered to the benefit of their patients and services. The project was mindful that several FAIs have underlined the problems with information sharing between services. To attempt to improve information sharing with unscheduled care services, the LES stipulated that special notes were shared in ADASTRA for each LD patient on the practices' register. Since the LES, systems have moved on and Primary Care has recently started using KIS (Key Information Summary) which is integrated into the practices' computer systems and will allow notes to be updated and shared more easily with unscheduled care. The next stage of the Primary Care project (see APPENDIX 1) aims to fortify the work already completed, to capture data, identify issues for practices and to share examples of good practice/systems to continue developing services. It is hoped that this will help guide and plan services around unmet health needs. Visits have been undertaken in each practice. Practices are asked to allow the group to see waiting rooms and clinical rooms. Linking with the administrative staff to gain an understanding of the systems of organising LD review appointments and any issues (eg appointments not attended). They have met with a member of the clinical staff to review the LD register and some examples of LD 19 reviews. The group have learnt issues for the practices and patients but also what is needed in termsof pathways of care for unmet health needs highlighted by the LD reviews. Findings will now be presented to the practices and the Board SUMMARY OF LOCAL ENHANCED SERVICE Practice updates LD register based on approved criteria of LD definition Practice identifies a lead health professional for the LD LES to complete approved training programme Lead coordinates coding of all LD patients to ensure diagnosis is an ‘Active’ ‘Significant’ code Lead coordinates completion of ‘Patient Alert Note’ summary for OOH notes Lead coordinates education and implementation within practice of electronic review document Health Screening Template Health screening of adults with a learning disability registered with GPs reveals high levels of unmet physical and mental health needs. (Kerr and Robertson 2010) A Primary Care Local Enhanced Service for Health Screening patients with a Learning Disability has been in place across NHS Western Isles for several years. This facilitates North Harris Medical Practice (Learning Disability Register Holder) to inform GP practices of forthcoming tri-annual health screening checks due on their respective clients. Practices will then request attendance of a Learning Disability nurse if required. A considerable amount of work is being undertaken in the Western Isles to develop an IT structure to update and improve on the current health screening system in view of advancing technology. 20 Collaborative meetings were held with invited representation from across the service delivery pathway As of 2012 all GP practices in NHS Western Isles now use EMIS. The project researched suitable models for health screening and a joint consensus was to use the RCGP model which is suitable for EMIS read coding. http://www.rcgp.org.uk/learningdisabilities/~/media/Files/CIRC/CIRC-7680/CIRCA%20StepbyStepGuideforPracticesOctober%2010.ashx This has now been piloted in Leurbost GP Practice and adaptations met and launched across the Western Isles in February 2012. This will now allow the GP to complete an electronically based Health Assessment that will form part of the patient record. Adverse findings will be referred through general electronic referral systems. Dr Keith Burns GP supported the implementation of Health Screening template into practices 2012. The use of the EMIS template for Health Screening will truly be realised in the future if the Health Board is able to invest in EMIS web (This is under consideration by the eHealth Programmes Board). The potential for analysis of current health trends and patterns of extended health needs information will provide for a more robust review of the health needs within this client group and future planning for service redesign will then include Learning Disability needs. With the structuring and development Scottish Learning Disability Observatory – this would allow NHS Western Isles to be one of the first Health Boards to be in a position of being able to contribute nationally to this level. Awareness Training Raise profile of clients’ needs through awareness training for all staff. Local awareness training – delivered by Project Manager over period of twelve weeks – open to all interagency staff. The training session was developed from several training packages from Forth Valley, Tayside and Lothian Health Boards. Interagency attendance of 105 staff from primary and secondary care, social and community care, third sector, allied health professionals and dental. Prominent figures were also invited to the Western Isles linked with effective service improvement in order to heighten the awareness of need for change to a greater level. LD Collaborative Training Events and Attendance Training Number Attendees of Staffing groups 21 Project Training 105 Community and Hospital Nurses, Aneathetists, ODP, AHP’s and Dental Services, voluntary and support services, Administrative Staff, PFPI, Social Work, Education, Scottish 21 Consortium for LD Senior Strategic and Operational Managers, Gp’s , Ambulance Service, Social Work, Stand up for 52 Yourself Advocacy Group Western Isles Aneathetists, Nurses, CE, AHP’s, Local Councillors, Consultant Nurse Lead MH and LD, Depute Head of Planning and Development, LD Nurses 6 Napier University 47 and Greater Glasgow and Clyde Training Link personnel identified through LESPrimary Care and link role -secondary care Adults Incapacity Training Consultants, Operational Managers, Ward Unit Managers, Nurses from Cancer care, Community, Well North, Psychiatry, LD, Pre – operative care, Diabetes Services, Alcohol support. AHPs – Speech and Language, Physiotherapy, O T, Podiatry. Local Council – Education, Advocacy, Administration, senior and care workers, Housing Support, Care Home Managers. with 85 Adult with 0 Incapacity Training for staff No applicants SCLD Easy Read 10 Training – March 2012 NHS/Council National Autism 43 Society Training Spell 1 and 2 – Feb 2012 CNES/Council (Napier Training) 22 Autism Train the 7 Trainer NAS Previous attendees at Spell 1 and 2 a prerequisite Adult Support and 396 and 148 All NHS Staff Protection repeat attendees Module Learn Pro Learning Disabilities Module Learn Pro 69 since 1/2/13 All NHS Staff Learning Disability 1 Dementia trainer CPN – currently extending training across care home settings. Talking Mats 2 trainers – sexual disclosure Consultant Gynaecologist CPN 844 and 148 repeat attendees Total Learn Pro Modules - transcribed with kind permission from NHS Lothian Adult Support and Protection Module –– Included in Mandatory training Learning Disability Module covering – – – – Health Needs Reasonable Adjustments Adults with incapacity – legislation and consent Challenging behavior AWI Website Legislation DVD development with Nicola Smith, Cairn Management Trust. Staff evaluation from the awareness raising sessions identified a general need for educational input on issues of capacity and rights for clients with a learning disability, as did the Millan Recommendations within the Donnet and Mauchland fatal accident inquiries. Future Focus - Staff have not yet identified with the Incapacity training available through Napier University – all nurses and Allied Health Professionals dealing with clients who need their capacity 23 assessed in order to consent to treatment should be trained and qualified in assessing capacity and taking informed consent for treatment plans and interventions. Having heard Nicola Smith present at one of the national inequality Network meeting, she was asked by the project to record on DVD format, the practicalities interpreting the legislation and how this impacts on clinical practice. The areas covered are : introduction, Principles of the Act, Roles and Responsibilities, Capacity and Consent, Procedure for Delivering Medical Treatment, Guardians and Attorneys, Covert Medication, Disclosing Information and Human Rights Introduction. NHS Western Isles Chief Executive and Medical Director have also contributed to the DVD content and are recorded supporting the content of the DVD. This was completed by Dec 2011. This has been developed into a web site on the intranet only http://www.wihb.scot.nhs.uk/LD/awiindex.html where staff can access clips of film with links to local and national policies, documents and legislation. The site will also provide a source for mandatory forms required such as Section 47 consent form. This link will be highlighted during induction for new staff and will also be available on the intranet. Survey Monkey reveals that staff reports it as a useful resource for practice and have highlighted that it should be to some level a national resource. Having recently been asked to do a presentation on capacity/consent to Medical Staff it highlighted situations about guardianship/power of attorney/capacity consent that staff are involved in locally on a frequent basis for which further support and guidance would be helpful. LD Services Website http://www.wihb.scot.nhs.uk/LD/index.html The local QIS review 2006 – reviewed a lack of knowledge amongst general staff about the Learning Disability Service and their role and remit. The Learn Pro modules now outline this to some depth. It was felt that a website development would also enable the local community to directly access information about local learning disability service provision. This information is available on the NHS Western Isles internet site under – Our Services – Learning Disability Services. The page contains information on the following: Local Services; Interagency Links, Identifies key staff and their roles across the Western Isles. Local Easy Read information on Chest Xray, Ultrasound and CT scan Links to Falls, Occupational Therapy, Speech and Language Therapy and Physiotherapy websites Your Health: NHS Scotland Easy Information zone – launched Feb2013 NHS Inform Information about Health Conditions, Well Being and Tests and Treatment Toolkit: 24 NHS Western Isles Communication Book All about Me DisDat Assessment tool How to use NHS 24 Autism Alert Card Application and Highlands and Islands Interagency explanatory video for use of the card. Top ten tips on Autism Communication Information: Links to useful sites and national resources Scottish Consortium for Learning Disability National Autistic Society The Challenging Behaviour Foundation Profound and Multiple Learning Disabilities Contact a family – Scottish based site for families with children with a disability Foundation for people with a learning disability Enable Scotland Enquire – Scottish Advice Service for additional support for learning Improving Health and Lives - Learning Disabilities Observatory British Institute for Learning Disabilities MENCAP Guardianship and Intervention orders Autism Alert Card: Autism Alert Card Application and Highlands and Islands Interagency explanatory video for use of the card Advocacy Details of the local Advocacy Services Website Learning Disability Link Role Key recommendations suggest that a learning disabilities liaison nurse be present in each hospital. This model was deemed unsuitable in its present outline for the remote and rural area. We cover an area of 3,500 square kilometres across an archipelago of 12 inhabited islands with a population density of 8.5 people per square kilometre. There are approximately 175 people with a learning disability and no critical mass of sufficient size to merit the appointment of a dedicated nurse co-ordinator. Most specialist general health services are delivered in tertiary centres on the mainland. 25 In response to this NHSWI has developed its own model, the link role, which we believe is a good quality model for implementation (Appendix 2). Supporting this is the identification of Learning Disability Link Practitioners from each department in the acute and community services and through the Local Enhanced service and departmental representation – 24 members . The task ahead is to formalise this structure and ensure its sustainability, putting in place Quality Assurance and Governance structures to sustain it. There is the potential for this to link with a formal Managed Clinical Network. LD Link Practitioner Representation covers: Wards – Long term stay – elderly, Surgical, Acute and Community Psychiatry, Theatre, Medical and Stroke care, Pharmacy, Maternity, Outpatients, Physiotherapy, Dietetics, Speech and Language Therapists, Occupational Therapist, Podiatry, Child and Adolescent Psychiatry (CAMHS), Health Promotion, Community Nurses from each district, X ray and Dental Services. A role descriptor has been developed with the link staff and passed by the QIPB in 2011. The outline is provided in Appendix 2. It has been agreed that this will be half an hour for training and half an hour for shared development and any local issues arising. Any additional training to what has already been outlined has been provided by NHS and third sector staff based on the topics staff identify as a knowledge gap. There is also scope to develop a departmental standards charter which areas can sign up to. Communication Training Recently we have also purchased two Body boards (visual aid) which will assist staff to support any training and health education delivery. The information packages include Smoking, Alcohol and Healthy Eating and Nutrition. They are resourced through HIRS – Health Information resource service NHS Western Isles. Talking Mats Communication Book Easy Read Training Go Talk 4 I pads with applications loaded to assist communication at point of contact with staff. Improving information inputs and facilitating choice (available through Speech and Language Department) Health Promotion Policy The Health Promotion Policy was developed and integrated in 2012. (Appendix 3) It outlines the structure for professional development of staff within the department to incorporate adapted approaches to information and sessional delivery inputs to take into consideration the needs of the 26 LD group. Active seeking out engagement opportunities in entire scope of health promotion and in particular topics where increased occurrence is recognised. Several local initiatives are underway and national projects are currently being absorbed into practice ie Healthy Eating, Healthy Living from NHS Greater Glasgow and Clyde. There has been the very recent launch of the NHS Easy Information zone – this link has been embedded in the intranet and internet site for ease of access by patients, carers and staff alike A range of health Promotion and healthcare information in different media, including film/video, electronic and print will be available and will cover a number of key health subjects and specific service information. The Western Isles also has a local Health Information site which provides information for clients and healthcare staff in leaflet, book , DVD and training packages format. The project has established a working relationship in extending the resources available to support clients with a Learning Disability. Within the project we are reviewing the easy read accessible information for specific conditions made available by the Scottish Consortium for Learning Disabilities through the Accessible Information link on the Knowledge Network. We are working at present on reviewing these materials with leads in specific departments and thereafter they will be incorporated into practice. Topics include : Cancer, Diabetes, Emotional Health, Epilepsy, Sexual Health This process is ongoing and will be aided in implementation by the staff in the link role. Video streaming of information onto local website is an option which would be useful for clients but this may take longer than the duration of the project. We have financed three licences’ of the Boardmaker software to give departmental access to symbols and templates for their own design and development Dental Treatment People will have the opportunity for planned access to dental care for regular examination and treatment. In meeting with the Chief Area Dental Officer for the Western Isles, who has a specific interest in supporting and caring for patients with a learning disability, it became clear that the dental department has already identified clients with a learning disability as a priority care group. The access to a flagging of needs within the dental system has been identified and as described earlier this is in the process of development. The dental services will facilitate access to everyone who wishes to have access and is at present in the final stages of developing an oral health improvement programme which will be delivered in home and care establishments. The vision for the service has been described as helping individuals who have no contact at present into regular routine care programmes. The department is also developing 27 an information structure which will inform individuals about the regular and out of hours service provision and how this differs for example between Stornoway and the more remote Island of Barra. Admission/Discharge Policy The project is currently collaboratively working with the GP involved in developing the LES and Senior Ward Manager from acute services, with input also from the local LD nurses. We are reviewing (with permission) the NHS Lothian document, Caring for Adults Patients 16+ with Learning Disabilities within a General Hospital Setting Policy. This document outlines principles and procedures for the management of patients with a learning Disability in the acute setting, in particular the areas of Elective and Emergency Admission Theatre and recovery Referral to Outpatients Core Principles for admission of a patient with a learning Disability Basic Risk Assessment Information about our local LD services. In order to fully implement this policy several ( Appendix 4) subsequent change improvements have to be met across systems, tracking and patient pathways. These changes are ongoing at present. The Senior Charge Nurse for Acute Services is continuing the implementation as the project draws to a close. Health Improvement Work The Collaborative linked Health Promotion Department and The local Sports Council and Scottish Disability Sport in a joint working towards facilitating the delivery of inclusive sport for people with a disability. Training in UK disability Inclusion, Boccia Leaders Course and Introducing athletics for people with a disability was delivery to key sports staff across the Western isles in advance of the event. The event was held in June 2013 – over 70 people attended the event held at the Lewis Sports Centre and it was open to all participants, parents families, carer, teachers and club coaches. The day consisted ‘Come and try’ practical sessions – allowing adapted access to sports such as golf, boccia, new age kurling, climbing, archery and dry side kayaking and sailing boat demonstration which proved very popular. Over 40 participants during the day expressed an interest in disability sailing becoming available across the Western Isles. 28 Learning Disability and Physical Activity Action Plan.docx There is new representation of the national Riding for the Disabled Group now based in the Western Isles and this opportunity was used to raise the profile of this valuable resource. The funding was also provided as an initial contribution to the purchase of adaptation equipment for inclusive sport and physical activity. This day enabled people who do not routinely access sports to discuss their access issues directly with the key stakeholders. Distat – Distress Assessment tool – http://disdattool.wordpress.com/about/ It was recognised within the LD project that current practice across NHS Western Isles incorporated only a linear pain rating scale of 0 – 10. Observational pain scales were researched and the Disdat assessment tool was considered best practice within the Health Inequalities network and specialist LD practice. This assessment tool is suitable for use in patients with brain injury, dementia, learning disability, stroke, palliative care and paediatrics. The project linked in with the authors NHS Tyne and Weir (Northumberland)of the assessment tool for authorities to be granted. This was processed through the Quality Improvement Board and training sessions were arranged for staff led by NHS Tyne and Weir Northumberland for clarification re approach and use. This is now included in the LD awareness session during orientation and link role members support its implementation into practice. Adapted nutritional scoring System The Health Inequalities Network meetings identified a strand of work in The State Hospital Carstairs related to assessing the nutritional scoring for people with a learning Disability and Mental Health Condition. (Appendix 5) It was recognised that patients with a Learning Disability were more likely to have an increase in their weight on admission to hospital. The package for training and the associated documentation were purchased for use across the Western Isles. A trial is being set in the elderly care/dementia ward at Western Isles Hospital and the assessment tool is available from the dietetics department for use with the patients with mental health and learning disabilities accessing general care facilities. Sensory Integration training Paediatric Occupational Therapy Services highlighted educational needs gaps which directly impacted on quality outcomes for children with sensory integration and processing difficulties. 29 Sensory Processing Disorder is a condition in its own right – however many children with autism spectrum disorder or learning disabilities also present with this condition. Funding was allocated through the project for the initial module of sensory integration training, and this has now been matched within the department by funding being made available for the next two modules to be completed. This has now been undertaken and the approach has been offered to children over the summer 2013 with evaluation of progress and outcomes. Healthy Eating , Healthy Living NHS Greater Glasgow and Clyde have launched an easy read toolkit for diet and nutrition education which includes all training and cooking session materials/film clips and guidance. Collaboration with Health Promotion, Dietetics and the Learning Disabilities nurse has identified that this new material addresses a gap in our current accessible materials. The implementation focus includes multi sector involvement across many community and third sector settings and is ongoing. Project Product Table Available in main report Figure 1 References and Bibliography References 1. Journal of Pediatric Psychology . (2000). Everyday pain responses in children with and without developmental delays . Journal of Paediatric Psychology . 25 (301), 8. 2. Symons FJ, Shinde SK, Gilles E. (2008) Perspectives on pain and intellectual disability. Journal of Intellectual Disability Research. 52(Pt 4), 275-7. 3. Emerson E, Hatton C. (2007). The mental health of children and adolescents with intellectual disabilities in Britain. British Journal of Psychiatry. 191, 493-99. 4. Doody GA, Johnstone EC, Sanderson TL, Cunningham-Owens DG, Muir WJ. (1998) ‘Pfropfschizophrenie’ revisited: Schizophrenia in people with mild learning disability. British Journal of Psychiatry. 173, 145-53. 30 5. Amiet C, Gourfinkel-An I, Bouzamondo A, Tordjman S, Baulac M, Lechat P, et al. (2008) Epilepsy in autism is associated with intellectual disability and gender: evidence from a meta-analysis. Biological Psychiatry. 64, 577-82. 6. Branford D, Bhaumik S, Duncan F. (1998) Epilepsy in adults with learning disabilities. Seizure 7:473-77. 7. Matthews T, Weston N, Baxter H, Felce D, Kerr M. (2008) A general practice-based prevalence study of epilepsy among adults with intellectual disabilities and of its association with psychiatric disorder, behaviour disturbance and carer stress. Journal of Intellectual Disability Research. 52 163-73. 8. Kerr M, Bowley C. (2001) Evidence-based prescribing in adults with learning disability and epilepsy. Epilepsia. 42 (Suppl.1), 44-45. 9. Kerr M, Bowley C. (2001) Multidisciplinary and multiagency contributions to care for those with learning disability who have epilepsy. Epilepsia. 42 (Suppl.1), 55-56. 10. Blaney A, Hanlon P, Judge K and Muirie J (Eds) (2002) Health inequalities in the new Scotland, Public Health Institute for Scotland, Glasgow. 11. NHS Scotland (2004) The health needs assessment report: people with learning disabilities in Scotland, NHS Scotland. 12. Scottish Government UK. (2008). The report of the Ministerial Task Force on Health Inequalities. Equally Well. Available: http://www.scotland.gov.uk/Publications/2008/06/25104032/0 Last accessed 06/06/13. 13. Adult Support and Protection Act 2007 http://www.legislation.gov.uk/asp/2007/10/contents 14. Mental Health Scotland Act (2003) http://www.legislation.gov.uk/asp/2003/13/ 15.The Equality Act (2010) http://www.legislation.gov.uk/ukpga/2010/15/contents 16. The Adult with Incapacity Act(2000) http://www.scotland.gov.uk/Topics/Justice/law/awi 17. Best Practice Statement – February 2008 Promoting access to Healthcare for people with a learning disability – guide to frontline NHS staff. NHS Quality Improvement Scotland. 18. Emerson, E. Baines,S. (2010) Health Inequalities and People with Learning Disabilities in the U.K: 2010. Department of Health. Improving Health and Lives: Learning Disabilities Observatory. 19. Mencap – London:Mencap,2007Death by Indifference. 20 Michael J, Healthcare for all: Report of the Independent Inquiry into Access to Healthcare for People with Learning Disabilities. London: Independent Inquiry into access to Healthcare for people with Learning disabilities, 2008 21. Scottish Government (2002) Promoting Health, Supporting Inclusion: The National Review of the Contribution of all nurses and Midwives to the Care and Support of People with learning disabilities, available on line http://www.scotland.gov.uk/Publications/2002/07/15072/8572 31 22. Scottish Government (2000) The Same as You: A review of services for people with learning disabilities, available on line http://www.scotland.gov.uk/Resource/Doc/1095/0001661.pdf 23. Scottish Government (2003) Fatal Accident Inquiry: Roderick Donnet ,available on line http://www.scotcourts.gov.uk/opinions/donnet.html http://www.scotcourts.gov.uk/opinions/cb12_02.html 24. Scottish Goverment (2003) Fatal Accident Inquiry: James Maughland , available on line http://www.scotcourts.gov.uk/opinions/cb12_02.html 25. 74 Lives and counting – Mencap Report – A progress Report 5 years on (2012) http://www.mencap.org.uk/74deaths 26. Autism Strategy for Scotland, Scottish Government , Glasgow 2012 http://www.scotland.gov.uk/Resource/Doc/361926/0122373.pdf 27. Keys to Life – Improving Quality of life for people with Learning Disabilities. Scottish Government June 2013 http://www.scotland.gov.uk/Publications/2013/06/1123 Bibliography NHS Quality Improvement Scotland (2006) Best practice statement. Promoting access to healthcare for people with a learning disability – a guide for frontline staff, NHS QIS, Edinburgh. NHS Quality Improvement Scotland (2004) Improving the health of people with a learning disability: An introduction to quality indicators for learning disabilities, NHS QIS, Edinburgh. Helping People Help Themselves – A review of the evidence considering whether it is worthwhile to support self – management May 2011. The Health Foundation Inspiring Improvement. ‘The same as you?’ 2000-12 Evaluation of progress from the perspectives of people with learning disabilities and family carers. Scottish Government. Edinburgh 2012. Glover, G. Emerson, E.(2012) Filling the Data Gaps. Progress in information about the Health Needs of people with Learning Disabilities. Department of Health 32 Goldbart, J. Caton, S. (July 2010) Communication and People with the most complex needs: what works and why this is essential. Reseach Institute for Health and Social Change Manchester Metropolitan University. MENCAP National CAMHS Support Service. Tackling Stigma. A Practical Toolkit Bringing together guideance, best practice examples, case studies, resources and literature to help tackle stigma associated with children’s and young people’s mantal health. Pote, H. And Goodban, David. (June 2007) A Mental health care pathway for children and young people with learning disabilities – A resource pack for service planners and practitioners. Death By Indifference Acutely Ill Patients in Hospital (2007)– Recognition of and response to acute illness in adults in hospital. July 2007 Nice clinical guideline 50 Developed by the Centre for Clinical Practice at NICE. London. Heslop, P. Blair,P. Fleming, P. Hoghton, M. Marriott,A. Russ,L. Confidential Inquiry into premature deaths of people with Learning Disabilities. CIPOLD – (2013) Appendices Appendix 1 – Primary care Work Primary care input 2013 - LEARNING DISABILITIES Background The success of the LD LES in 2011/12 has highlighted the interest in the needs of this vulnerable group of patients in the Western Isles. Feedback included comments regarding the issue of Incapacity across the Western Isles in both primary and secondary care. The requirement to protect patients by ensuring that treatment and intervention is appropriate and proportional has been raised as an area for further development. Building on the success of the LD LES the following outlines a proposal to raise awareness of Incapacity as it relates to the Learning Disabilities population. 33 The obvious knock on effects of this awareness raising for other vulnerable groups (e.g. Dementia patients) will also be of benefit to the population of NHSWI and the broad cohort of patients affected will undoubtedly act as a strong incentive to ensure engagement. The LES has allowed Practices to use an electronic template which will enable collection of data. It is hoped that this will help guide and plan services around unmet health needs. The project aims to capture this data and help practices use the information they have gathered to the benefit of their patients. This work will enable practices look at their systems and environments for patients to ensure thie facilitates attendance and best care. There is a need to support carers and parents of patients with Learning Disabilities through a multidisciplinary approach. This is particularly true around the transition to adult services. The Learning Disability services need to liaise with CNES and the third sector for this. The project would aim to strengthen these links and improve access to information and support for patients/carers through the Learning Disability Community Nurses, North Harris Medical Practice and the Learning Disability Partnership. Aspects Preparatory work for project: o design of presentation o research into IT systems/recall o examples of good practice with appointments/practice environment o Easy-Read format letters and information for NHS WI Develop a programme of education and support in association with the LD nursing staff to take to primary and community care staff. Programme to be taken to individual practices (10 practices) o Presentation (KB/LD) o Review of IT system for call/ recall (KB/KB?) o Review of environment / appointments/ clinic set up to help develop systems that match the ideal environment for patients with LD (LD) o Case presentation and case reviews (KB/LD) o Anticipatory Care Planning Develop a programme of education and support to take to the rotating junior medical staff on a sustainable basis o Presentation (KB) 34 Post-visit work o Compile report for individual practices with suggestions for ongoing work o Compilation of report for NHSWI Mental Health and Learning DIsability Services to present findings in terms of referrals to various services and unmet needs Liaison with Council services and voluntary sector to strengthen links for community learning disability services Time Commitment Development of 1ry/2ry care programme as outlined above: 16 sessions Delivery of programme across 1ry care NHSWI: 15 sessions (to include travel) Delivery of programme across 2ry care: 3 sessions Post-visit work and liaison with other services: 8 sessions Duration Programme to be delivered within 12 months (January 1st 2013- January 1st 2014) with a clear understanding that there is a commitment to use the capital investment by April 2013. Kirsty Brightwell November 2012 35 Appendix 2 LD Link Role Descriptor Departmental Learning Disabilities, Autism and Safeguarding Vulnerable Adults. Link Practitioner Role Description Role Purpose Learning Disabilities link personnel will be a department based champion for learning disabled patients. They will promote best practice around the care and treatment of patient with a Learning disability during their time in that particular department. To act as an resource, disseminate information and be the advocate for patients with a learning disability, and or Autism Spectrum Disorder that access services in that area. To act as a resource to other staff within their unit for safeguarding adult issues. The role represents a prestigious self development opportunity by enabling their department to meet the unique needs of learning disabled patients thus ensuring that practise is robust and of a high standard. Individual departmental champions will become part of a network that supports continuous professional development. Key Duties and Responsibilities To disseminate and cascade updated information about learning disabilities and/or Autism Spectrum Disorder and Safeguarding. Ensuring all staff are aware of the learning disability and safeguarding resources available at local level. To contribute towards the area/department compliance with the Equality Act (2010) Raising awareness of what constitutes a reasonable adjustment. To encourage the participation of the uptake of staff to complete the e learning training packages available for safeguarding vulnerable adults and learning disability and Aspergers. 36 To be involved in developing as required accessible information relevant to their area. To signpost other staff to the resources available to support the development of accessible information e g photo symbols bank – Health Education Resource Centre, easy health website. Act as patients advocate and support colleagues to understand and use the approaches contained within the; o Adults with Incapacity Act Scotland (2000) www.scotland.gov.uk/Topic/Justice/law/awi o Mental Health Care and Treatment Act 2003 www.scotland.gov.uk/Publications/2004/01/18753/31686 o Adult Support and Protection Act 2007 www.scotland.gov.uk/Topics/Health/care/adult-care-and-support To understand barriers to communication and act as a resource to staff for using alternative methods or tools of communication, and refer onwards for specialist support. Eg speech therapist. To assist staff to identify risks for patients with a learning disability, maintaining effective communications within the departmental team on best practice and developments which NHSWI is making to meet the needs of this patient group. Promote the safety and well being of patients who have a learning disability, staff and other visitors to the department. Reporting appropriately any identified obstacles, issues around delivery of effective care. To have an active understanding of Adult Support and Protection – Western Isles Multi-agency Procedures. Health Promotion Policy Appendix 3 Health_Promotion_Le arning_Disabilityfinal_draft_2[1].doc 37 Hospital Policy Draft Appendix 4 Version 6.docx Adapted Nutritional Scoring System - Appendix 5 Scan-to-Me from rnp0026734b8961.wi.scot.nhs.uk 2013-09-16 120312.pdf 38