Self Management of Pain
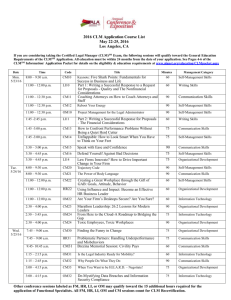
advertisement

Level 2 Pain Training Self Management and Chronic Pain 7th January 2016 Fife Integrated Pain Management Service Ros Standish, Occupational Therapist & Dr Alice Wells, Clinical Psychologist Schedule What is self-management? Over-activity rest cycle and pacing Exercise, Relaxation and Sleep 15 mins Break (2.45pm) Barriers to self Management Behaviour Change Case Discussions and questions FIPMS Questionnaires and Feedback (4pm) Wagner’s chronic care model Wagner E H Chronic Disease Management : What will it take to improve care for Chronic Illness?: Effective Clinical Practice 1998 1:2-4 What is Self Management? http://www.paintoolkit.org/tools http://www.paintoolkit.org/tools Group discussion •What previous experience do you have of introducing/using self management with patients? •What health conditions would self management be important for? •What does self management involve for the patient? •What does it require from the health professional? What is self-management? Life with a long term condition: the person’s perspective Interactions with the service: planned or unplanned Problem solving: Time limited consultation/s providing motivational support Care planning: A system of regular scheduled appointments, providing proactive structured support Care pathways: providing specific interventions NB : People may also be accessing a wide variety of other support e.g. from within their communities Taken from the Health Foundation, Inspiring Improvement: Improving Outcomes by Helping People Take Control. Self-management All patients with chronic illness make decisions and engage in behaviours that affect their health People are experts in their experience of their own condition Health outcomes depend to a significant degree on the day to day decision and activities that people with chronic conditions make and undertake to manage their condition Biopsychosocial Model Psycho & social part relates to the person as a human being e.g. can you look the knee and ignore the person… Social, cultural, personal dimensions interact with pain mechanisms Understanding that each individual experiences pain differently and it is actually hard how to determine how any individual will react Self-management: The Evidence “is likely to work best when implemented as part of wider initiatives to improve care through educating practitioners, applying best evidence, and using technology, decision aids and community partnerships effectively.” (The Health Foundation, 2011) Self-management: Why is it important? 80% to 90% of all care for people with LTC is undertaken by patients themselves and their families. Patients with chronic pain often find medicine and surgery does little to help their condition Self-management: Why is it important in chronic pain? Reported benefits of self management include: Fewer pain flare-ups Increased sense of control Less stress and improved mood Improved relationships Return to previously enjoyed activities Self-management in Chronic Pain Can include: - Information on their condition - Introducing self-management - Psycho-education on stress and pain management - Cognitive Behavioural Therapy and Acceptance & Commitment Therapy - Exercise and Relaxation - Preparation for Flare-ups – Have a plan! - Creating communication with the client to get an understanding of their pain management expectations and barriers. Acceptance Understand your condition Flare ups Pacing / Activity Management Sleep The Pain Self Management Jigsaw Medications Exercise Pain Self Management Jigsaw Goal setting Unhelpful thinking Relaxation The overactivity-rest cycle http://www.paintoolkit.org/tools The overactivity-rest cycle In the long term Good day Bad day Usual activity levels Introducing Pacing and Activity Management • Recognising the over-activity rest cycle • Awareness of habits – “I’ve just always done it that • • • • way” Tendency to push to complete perhaps because finds it unsatisfactory to not finish Encouragement to listen to signs of needing to stop “Could you do the same again tomorrow?” – promoting consistency and sustainability Is it worth it? Values driven activity 5 Pacing Principles Finding your baselines – what time can I spend on an activity before any increase in pain. Planning – plan activities through out the day and including relaxation and rest breaks. Prioritising – what has to be done vs. what can wait Involving others – delegate if able Incorporating gentle graded exercise Over Activity Rest Cycle V Pacing Pacing/graded functional activity Movement/Function can occur without increase in pain Movement/Function in a comfortable range Brain thinks “ Situation Better, threat less” Wind down, pain less No longer need red alert Key messages on activity management • • • • Everyone has choices about the activities they wish to pursue. Pacing is a way to manage chronic pain on a daily basis and requires some acceptance of their limitations. Activities important to them can also be accommodated even if this leads to flare-ups. Its about managing activity in a way that works for the individual and helps to maintain their quality of life. Some specific strategies Exercise Encourage regular gentle exercise (e.g. swimming, walking) Make it a part of everyday activities – reminding the need to pace and plan all daily activities Many don’t think they can do it based on: Past experience Fears and beliefs Motivation Education, benefits and de-conditioning Active Options 2 Small manageable goals Downwards spiral Pain increases Avoid activities Do less Lose fitness Pain on less effort Lose more fitness Do less Pain on minimal effort Upward Spiral Return to other activities Reduce fear Try something different Increase confidence Feel stronger Try something you enjoy Feel in control by not flaring up Pain on minimal effort Sleep Vicious cycle Sleep hygiene Time to unwind Regular bedtime- 8 hours before your alarm will ring the next day Avoid stimulants Lights out as soon as you are in bed If you do not fall asleep within about ½ hour, get out of bed and relax in another room until you feel tired again. Repeat this step as often as you need to. Some specific strategies Relaxation Pain is influenced by emotional and social factors e.g. stress. Relaxation exercises calm your mind, reduce stress hormones in your blood, relax your muscles, and elevate your sense of well-being. Relaxation isn’t just watching TV… Diaphragmatic breathing Progressive muscular relaxation Guided imagery or visualisation Mindfulness Visit www.moodcafe.co.uk or http://stepsforstress.org/ for relaxation exercises and CD 15 minute break What are barriers to Self Management? Group discussion (10 mins) •What barriers have you encountered? •What barriers might you expect to encounter? Barriers to self-management • Hurt and harm beliefs Ask: – What do they think is happening inside their body? – Why do they think they experience symptoms? • Pain education - weaken the grip of pain with knowledge and understanding to allow patient to rationalise and reason their symptoms • Gently challenge their beliefs e.g. Is that knee older than the other? Does the spine not crumble on a good day – would an XR/MRI look different on a bad day than the day before? Barriers to self-management Depression Persistent low mood and hopelessness Patient may not see the point in self-management Poor motivation and enjoyment Patient may be unable to motivate themselves to change their behaviour and sustain any changes Disrupted self-care Affected concentration and memory Patient may be unable to take in and/or remember selfmanagement advice Barriers to self management Unhelpful thinking styles Black & white thinking Catastrophising - Assumption that the worst is happening and will continue to happen Rumination -strongest predictor of poor prognosis Education Challenge assumptions Graded exposure Groups Barriers to self-management Locus of Control “the extent to which individuals believe that they can control events that affect them” Internal vs external An external locus of control would influence an individual’s adoption of self-management Barriers to self-management Fear avoidance Ask: What do they think would happen if....? And what would that mean? Observation- do they use their hands to lean on things? Pain education Graded exposure approach to exercise Groups Downwards spiral & mood Pain increases Avoid activities Do less Lose fitness Pain on less effort Lose more fitness Do less Pain on minimal effort Barriers to Self Management Expectation of Roles Roles of the patient Role of the carer Role of the Health Professionals Role of Others Barriers to self-management Resources vs demands Self-efficacy and health behaviour change Transtheoretical or “Stages of Change” model Increasing motivation and exploring ambivalence Communication is key: Understand the patient by listening 1. ‘Why do you think you have chronic pain?’ 2. ‘What does your pain mean to you from your point of view? 3. ‘How has the pain impacted on your life from your point of view?’ 4. ‘What would be important things for you to work on?’ 5. ‘What do you think would help?’ Increasing motivation and exploring ambivalence Education Validation/understanding patient Evoking change talk (motivational interviewing) Encourage Small steps Increasing motivation and exploring ambivalence What would you like to see different about your current situation? What makes you think you need to change? What will happen if you don’t change? How can I help you get past some of the difficulties you are experiencing? If you were to decide to change, what would you have to do to make this happen? INFORMATION Book Prescription Scheme Maintenance Exercise Classes and Active Options 2 Web Sites: http://www.knowledge.scot.nhs.uk/pain/nhs- boards/nhs-fife.aspx www.chronicpainscotland.org www.painassociation.com www.painconcern.org.uk (Airing Pain Project ) www.paintoolkit.org www.moodcafe.co.uk Acceptance Understand your condition Flare ups Pacing / Activity Management Sleep The Pain Self Management Jigsaw Medications Exercise Pain Self Management Jigsaw Goal setting Unhelpful Thinking Relaxation STRUCTURE OF SERVICES HOW AND WHEN TO REFER Who are we and where do we fit in? How do I access the Chronic Pain Management Service? Who should I refer? Who should I not refer What should I do for my patients before referral? Kaiser Permanente Model Secondary Care Complex patients Primary Care RIVERS Program Less complex patients Mostly musculoskeletal pain Chronic Pain Patients Cared for in General Practice / Self-Care/ CPPN HOW DO I REFER? Referrals should be sent to: Pain Clinic (FIPMS), QMH Patients are triaged centrally to most appropriate branch of service. Triage is influenced by referral letter, HADS score ,PSEQ coping skills indicator and patient information from questionnaire. Fife’s Pain Service Patient requiring Pain Management -Referred by GP/ Physio/ Other Jan 2012 Central Point of referral Pain Clinic QMH Questionnaire sent to patient to be returned within 2 weeks Questionnaire/ Referral letter triaged to intervention depending on complexity Less complex: Primary Care More complex: Secondary Patients attend information session x 2 CONSULTANT Physio Pre-assessment NEW Community Pharmacy Med review clinics Pharmacy Appt One to one appts Joint Assessment NURSE- PHYSIO – OT- Psychology RIVERS 5 weeks ( Exercise & Education & Medication Review)- Group of 10- 12 pts 4/5 venues across FIFE ‘Keeping Afloat’ exercise class Kingdom Pain Management Programme 10-12 weeks :2 venues across Fife Voluntary Sector Maintenance- Pain Association Scotland/ Pain Concern/