IAEA Training Material on Radiation Protection in Radiotherapy
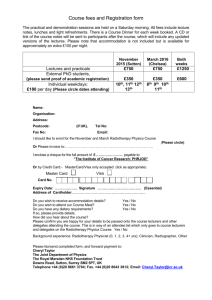
advertisement

IAEA Training Material on Radiation Protection in Radiotherapy Radiation Protection in Radiotherapy Part 7 Design of Facilities and Shielding Rationale In radiotherapy, a potentially lethal dose of radiation is delivered to patients. In order to avoid misadministration and exposure of other individuals (staff, visitors, general public) a radiotherapy facility must be appropriately designed. Shielding is an essential part of this design process. Radiation Protection in Radiotherapy Part 7, lecture 1: Facility design 2 Contents Lecture 1: Design of a radiotherapy facility components of a radiotherapy department design criteria Lecture 2: Shielding general considerations external beam radiotherapy brachytherapy Radiation Protection in Radiotherapy Part 7, lecture 1: Facility design 3 Objectives - on completion, participants should Understand the underlying principles for the design of a radiotherapy facility Be familiar with the safety requirements for the design of radiotherapy facilities including interlocks, maze design and warning signs. Be able to calculate the shielding thickness required for a particular barrier Radiation Protection in Radiotherapy Part 7, lecture 1: Facility design 4 IAEA Training Material on Radiation Protection in Radiotherapy Radiation Protection in Radiotherapy Part 7 Design of Facilities and Shielding Lecture 1: Facility Design Objectives of lecture 1 Be familiar with components of a radiotherapy department Understand the basic layout and design features of a radiotherapy department Radiation Protection in Radiotherapy Part 7, lecture 1: Facility design 6 Contents of lecture 1 1. Components of a radiotherapy department 2. Departmental planning and layout 3. Design considerations Radiation Protection in Radiotherapy Part 7, lecture 1: Facility design 7 1. Components of a typical radiotherapy department Diagnostic facilities (CT, MRI, …) Simulator Mouldroom Treatment planning External beam treatment units Brachytherapy equipment Clinic rooms, beds, ... Radiation Protection in Radiotherapy Part 7, lecture 1: Facility design 8 Components of a Radiotherapy Department Outpatient areas Diagnostics Clinics Therapy Radiation Protection in Radiotherapy Inpatient areas Oncology ward Brachytherapy Non-patient areas Part 7, lecture 1: Facility design 9 Radiotherapy is typically part of a large hospital Use of other services: Diagnostics Nuclear Medicine Maintenance Domestic/kitchen In patients/nursing Administration Radiation Protection in Radiotherapy Part 7, lecture 1: Facility design 10 Areas not directly related to patient care Offices Workshops (physics, electronics, mechanics) Storage Teaching Research Radiation Protection in Radiotherapy Part 7, lecture 1: Facility design 11 Areas not directly related to patient care which need to be considered from a radiation protection point of view Offices Workshops (physics, electronics, mechanics) Storage (including isotopes) Teaching Research Radiation Protection in Radiotherapy Part 7, lecture 1: Facility design 12 Workshops Physics workshop/lab: need to consider check sources for dosimetric equipment Radiation Protection in Radiotherapy Part 7, lecture 1: Facility design 13 Storage areas for sources Hotlab Source preparation area for interim storage of sources Decay lab - decay of radioactive material (e.g. 192-Ir) prior to disposal Radiation Protection in Radiotherapy Part 7, lecture 1: Facility design 14 Research Many different possibilities for radiation protection problems: students participating in research and observation of practice (training?) after hours work (confined spaces? Should there be more than one researcher?) labs including radiobiological research ethics - see part 9 on medical exposure Radiation Protection in Radiotherapy Part 7, lecture 1: Facility design 15 Components of the outpatient area Reception area Clinic rooms - new patients and review Waiting area Diagnostics - e.g. CT scanner, simulator, dark room Treatment units - e.g. 60-Co, linacs, superficial/orthovoltage, HDR brachytherapy Treatment planning including mould room Dosimetry, physics and electronics labs Office space and storage (!) Radiation Protection in Radiotherapy Part 7, lecture 1: Facility design 16 Flow chart for patient treatment... Radiation Protection in Radiotherapy Part 7, lecture 1: Facility design 17 Flow chart for data Radiation Protection in Radiotherapy Part 7, lecture 1: Facility design 18 Quick task Please try to follow a patient through the components on the previous slide. Label the components from 1 to 7 in the order as the data of a particular patient would be acquired and processed Outpatient data flow Radiation Protection in Radiotherapy Part 7, lecture 1: Facility design 20 2. Layout of a department Planning should include all components and allow for growth Easy access is required for patients and ambulance - patient may be transported by wheelchair or on a trolley bed Typically a radiotherapy department is part of a larger hospital complex - access must be ensured, in particular to: diagnostics (X Ray, nuclear medicine) oncology clinic and beds Radiation Protection in Radiotherapy Part 7, lecture 1: Facility design 21 Layout example Radiation Protection in Radiotherapy Part 7, lecture 1: Facility design 22 Components of a brachytherapy section Different layout and components for high dose-rate (HDR) brachytherapy similar to external beam usually outpatient facility low dose-rate (LDR) or pulsed dose-rate (PDR) in-patient procedure treatment room in a ward Nucletron HDR unit Radiation Protection in Radiotherapy Part 7, lecture 1: Facility design 23 Patient flow in brachytherapy Treatment decision Ideal plan - determines source number and location Implant of sources or applicators in theatre Localization of sources or applicators (typically using X Rays) Treatment plan Commence treatment Radiation Protection in Radiotherapy Part 7, lecture 1: Facility design 24 Components of a brachytherapy suite in the ward Operating theatre for placement of sources or applicators Diagnostic facility to localize sources Shielded room - consider manual and remote afterloading Dosimetry and physics area Source preparation may be required (e.g. 192-Ir wire cutting) Source storage - include also case of emergency Nurse station with patient intercom Radiation Protection in Radiotherapy Part 7, lecture 1: Facility design 25 Transport issues Ideally, all these components should be close together - good departmental planning can ensure this. In practice, often these components are far apart from each other leading to the need for patient transport (sources or applicators can move!) or transport of radioactive material through the hospital Radiation Protection in Radiotherapy Part 7, lecture 1: Facility design 26 Designation of areas Public Supervised operator console Controlled treatment rooms brachytherapy source storage and preparation Radiation Protection in Radiotherapy Part 7, lecture 1: Facility design 27 Supervised Areas BSS Appendix I.24. “Registrants and licensees shall designate as a supervised area any area not already designated as a controlled area but where occupational exposure conditions need to be kept under review even though specific protection measures and safety provisions are not normally needed.” Radiation Protection in Radiotherapy Part 7, lecture 1: Facility design 28 Controlled areas BSS appendix I.22.: “In determining the boundaries of any controlled area, registrants and licensees shall take account of the magnitudes of the expected normal exposures, the likelihood and magnitude of potential exposures, and the nature and extent of the required protection and safety procedures.” Radiation Protection in Radiotherapy Part 7, lecture 1: Facility design 29 Quick task Please identify the areas on the handout of the departmental plan which should be controlled or supervised Radiation Protection in Radiotherapy Part 7, lecture 1: Facility design 31 Controlled and supervised areas Access restrictions Require warning signs Monitoring of staff Interlocks where appropriate Written procedures Radiation Protection in Radiotherapy Part 7, lecture 1: Facility design 32 Planning and lay-out When planning a new facility assumptions must be clearly stated Plan for the future - consider expansions and increase in workload Megavoltage treatment rooms are typically in the basement It is usually best to place bunkers together to use common walls Size matters - bunkers should be generous Radiation Protection in Radiotherapy Part 7, lecture 1: Facility design 33 Advantage of large bunker Distance is effective shielding Consider special treatments such as TBI Need storage space for accessories and patient immobilisation Allows for future upgrades of equipment (FAD 80 ---> 100cm) and increases in shielding Radiation Protection in Radiotherapy Part 7, lecture 1: Facility design 34 Treatment bunkers require lots of storage space for patient treatment aids... Radiation Protection in Radiotherapy Part 7, lecture 1: Facility design 35 More design criteria: Make use of landscape features (e.g. built bunkers into a hill) and consider adjacent buildings Positioning the control room and the equipment within so that staff have a good view of the treatment room access corridors entrance to the treatment room Radiation Protection in Radiotherapy Part 7, lecture 1: Facility design 36 …before planning and shielding Check and document all assumptions Verify them with authorities and colleagues Plan size and workload of the facility be conservative, the design should be adequate for the next 20 year including room for expansion Radiation Protection in Radiotherapy Part 7, lecture 1: Facility design 37 Typical assumptions for planning a new facility 4000 new cases of cancer per year per million population 50% will require radiotherapy at some stage 400 to 500 cases per megavoltage unit per year ...may depend on local conditions Radiation Protection in Radiotherapy Part 7, lecture 1: Facility design 38 Design considerations: External Beam Radiotherapy Placement of the treatment unit Primary beam direction Operator location Surrounding areas - should have low occupancy Costs can be reduced if the design is good for extension is usually much larger than for allowing for expansion already during the building phase Radiation Protection in Radiotherapy Part 7, lecture 1: Facility design 39 Typical megavoltage room layout Radiation Protection in Radiotherapy Part 7, lecture 1: Facility design 40 Design criteria: External Beam treatment area clear signs are required in areas leading to treatment units patient and visitor waiting areas should be positioned so that patients are unlikely to enter treatment areas accidentally patient change areas should be located so that the patient is unlikely to enter a treatment area accidentally shielding/maze/doors discussed later Radiation Protection in Radiotherapy Part 7, lecture 1: Facility design 41 Megavoltage Room Is a door needed? Door interlocks Protocol for closing the door and activating radiation Door interlocks Radiation warning signs are needed Radiation Protection in Radiotherapy Part 7, lecture 1: Facility design 42 Radiation Safety in Radiotherapy the possibility of accidental exposure can be minimised by measures such as positioning the control room and the equipment within so that staff have a good view of the treatment room access corridors entrance to the treatment room Radiation Protection in Radiotherapy Part 7, lecture 1: Facility design 43 Control area Spacious Patient monitor Clear view of surrounding area Control of access to bunker Radiation Protection in Radiotherapy Part 7, lecture 1: Facility design 44 Radiation Safety in Radiotherapy the possibility of accidental exposure can be minimised by measures such as positioning clear signs in areas leading to treatment units patient and visitor waiting areas so that they are unlikely to enter treatment areas accidentally patient change areas so that the patient is unlikely to enter a treatment area accidentally Radiation Protection in Radiotherapy Part 7, lecture 1: Facility design 45 A note on ventilation This should be reviewed for high energy accelerators > 15 MeV There may be a build up of ozone and induced radioactive Oxygen-15 and Nitrogen-13 10 air changes per hour or greater should be satisfactory Radiation Protection in Radiotherapy Part 7, lecture 1: Facility design 46 Other irradiation units for external beam radiotherapy Simulator and CT scanner - design of rooms similar to the design of a diagnostic radiology facility. This is dealt with in the course on diagnostic radiology Protons, neutrons, pions,… beyond the scope of the present course Superficial/orthovoltage units Radiation Protection in Radiotherapy Part 7, lecture 1: Facility design 47 Superficial/orthovoltage treatment room Radiation Protection in Radiotherapy Part 7, lecture 1: Facility design 48 Some comments The movement of the X Ray tube may be restricted to prevent the primary beam from hitting areas which are not sufficiently shielded A lead glass window is typically sufficient for viewing - its integrity must be checked Radiation Protection in Radiotherapy Part 7, lecture 1: Facility design 49 Brachytherapy Source assembly area may be required A secure storage area for the source safe and source transfer procedures may be required In room area monitor HDR Principles are similar to megavoltage unit Radiation Protection in Radiotherapy Part 7, lecture 1: Facility design 50 Design criteria: HDR treatment rooms The design of these rooms follow similar guidelines to those of accelerator rooms Maze and door must typically be included Similar interlocks to those used in accelerator rooms are required Radiation Protection in Radiotherapy Part 7, lecture 1: Facility design 51 HDR room design Some centres use accelerator rooms for HDR brachytherapy treatment. This practice has some disadvantages: Usually not enough space for diagnostic equipment for source localization Time pressure - the next external beam radiotherapy patient is scheduled Difficulties in predicting what assumptions shall be used for shielding calculations Radiation Protection in Radiotherapy Part 7, lecture 1: Facility design 52 HDR room design (example) Radiation Protection in Radiotherapy Part 7, lecture 1: Facility design 53 Brachytherapy Low Dose Rate Usually in a ward Manual/Afterloading Safety of sources Staff/visitors Remote afterloading Door interlocks Shielding could also be incorporated in the bed. This reduces cost and increases patient anxiety - it is typically better to shield the room Shielding issues Radiation Protection in Radiotherapy Part 7, lecture 1: Facility design 54 Design criteria: LDR brachytherapy in the ward Typically some shielding is required Avoid treating more than one patient in a single room - this leads inevitably to additional unnecessary does to the patient(s) and most likely to staff Use rooms at the end of the ward, preferably on outside walls Consider adjacent room use (could a storage space turn into an office?) Radiation Protection in Radiotherapy Part 7, lecture 1: Facility design 55 An additional note on department planning... CT MR Archive HIS / RIS Portal Imaging LiteBox Image Image Not DICOM All Image SS, Plan, Image SS, Plan, Dose Image, SS, Plan Image Image, SS, Plan Simulator Virtual Sim. Radiation Protection in Radiotherapy Record All LiteBox Image Plan LiteBox TPS Review St. Treatment Part 7, lecture 1: Facility design 56 Message... A radiotherapy department is a complex environment It relies heavily on data transfer patient, machine and process data This affects also patient and staff safety!!! Planning must include allowance for computerization and networking Radiation Protection in Radiotherapy Part 7, lecture 1: Facility design 57 3. Design considerations Treatment rooms Shielding/door/maze - discussed in next lecture Interlocks Emergency off buttons Warning signs Beam on/off indicator Radiation Protection in Radiotherapy Part 7, lecture 1: Facility design 58 Interlocks the possibility of accidental exposure can be minimised by measures such as room interlocks involving (possibly as a combination) door gate light beams audible alarm Radiation Protection in Radiotherapy Part 7, lecture 1: Facility design 59 Emergency off buttons: where should they go? Radiation Protection in Radiotherapy Part 7, lecture 1: Facility design 60 Suggested solution Radiation Protection in Radiotherapy Part 7, lecture 1: Facility design 61 Warning signals There should be a visible signal when radiation is being produced at the entrance of the maze, control area and in the treatment room There should be an audible signal in the treatment room just prior to radiation being produced Radiation Protection in Radiotherapy Part 7, lecture 1: Facility design 62 Brachytherapy wards design features Require radiation monitor at the door to avoid patient leaving the room with sources in place Manual afterloading: Warning signs required Remote afterloading: Interlocks at the entrances should cause the sources to retract if someone enters the room (if it is an automatic afterloading system) Area monitor Radiation Protection in Radiotherapy Part 7, lecture 1: Facility design 63 Summary Careful planning of a new radiotherapy facility or any extensions helps to optimize protection (and save costs) There are many features of a radiotherapy treatment area which must be considered including interlocks and warning signs Radiation Protection in Radiotherapy Part 7, lecture 1: Facility design 64 Where to Get More Information IAEA TECDOC 1040 parts 1, 5, and 6 of the course Radiation Protection in Radiotherapy Part 7, lecture 1: Facility design 65 Any questions? Question: Consider that you would like to submit an application for authorization of the use of radiation for radiotherapy. What information would a regulator need in such an application ? Some information required Drawings to scale - including: direction of north exact position of the equipment location of doors and windows ducts or other penetrations through a wall relevant identification of rooms (number) cross sections (above and below?) exact distances where relevant Indications of adjacent areas/buildings Radiation Protection in Radiotherapy Part 7, lecture 1: Facility design 68 Cross sections are helpful What is down under here??? (this MUST be stated) Radiation Protection in Radiotherapy Part 7, lecture 1: Facility design 69 Information required (cont.) Any features affecting radiation safety Indication of radiation protection measures: emergency off buttons monitors safe for sources Shielding - normal in walls and additional (see next section…) Radiation Protection in Radiotherapy Part 7, lecture 1: Facility design 70 Acknowledgements John Drew, Westmead Hospital Sydney Radiation Protection in Radiotherapy Part 7, lecture 1: Facility design 71