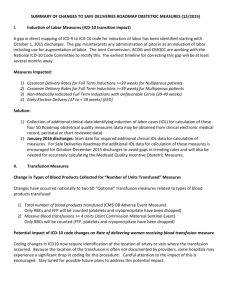
NYHIMA 2014 Annual Conference:
ICD-10 Data Analytics That Help Focus CDI
Physician Training and CDI Staff Efforts
June 3, 2014
Presented By:
Kim Charland, BA, RHIT, CCS
Senior Vice President Clinical Innovation
Panacea Healthcare Solutions, Inc.
Disclaimer
•
•
•
•
•
•
Panacea Healthcare Solutions, Inc. has prepared this seminar using official Centers for Medicare and
Medicaid Services (CMS) documents and other pertinent regulatory and industry resources. It is designed to
provide accurate and authoritative information on the subject matter. Every reasonable effort has been made
to ensure its accuracy. Nevertheless, the ultimate responsibility for correct use of the coding system and the
publication lies with the user.
Panacea Healthcare Solutions, Inc., its employees, agents and staff make no representation, warranty or
guarantee that this information is error-free or that the use of this material will prevent differences of opinion
or disputes with payers. The company will bear no responsibility or liability for the results or consequences of
the use of this material. The publication is provided “as is” without warranty of any kind, either expressed or
implied, including, but not limited to, implied warranties or merchantability and fitness for a particular purpose.
The information presented is based on the experience and interpretation of the publisher. Though all of the
information has been carefully researched and checked for accuracy and completeness, the publisher does
not accept any responsibility or liability with regard to errors, omissions, misuse or misinterpretation.
Current Procedural Terminology (CPT ®) is copyright 2013 American Medical Association. All Rights
Reserved. No fee schedules, basic units, relative values, or related listings are included in CPT. The AMA
assumes no liability for the data contained herein. Applicable FARS/DFARS restrictions apply to government
use.
CPT® is a trademark of the American Medical Association.
Copyright © 2014 by Panacea Healthcare Solutions, Inc. All rights reserved.
– No part of this presentation may be reproduced in any form whatsoever without written permission from
the publisher
– Published by Panacea Healthcare Solutions, Inc., 287 East Sixth Street, Suite 400, St. Paul, MN,
55101
3
© 2014 Panacea Healthcare Solutions, Inc.
Today’s Agenda
•
•
•
•
•
Why ICD-10 Data Analytics?
Case Studies: ICD-10 Data Analytics Results
Top ICD-10 Diagnosis Documentation Concepts
Top ICD-10 Procedure Documentation Concepts
About 16-Months To Go……..Were Do We
Focus?
4
© 2014 Panacea Healthcare Solutions, Inc.
WHY ICD-10 DATA
ANALYTICS?
Why ICD-10 Data Analytics?
• Use Your Data To Create Education Material:
– Identify documentation gaps
– Classify your gaps into DRGs, documentation
diagnosis and procedure concepts, specialty, and
Physician
– Develop tools to aid Physicians
– Education Program – General Sessions / Reporting,
Specialty Sessions, One-on-One Sessions
6
© 2014 Panacea Healthcare Solutions, Inc.
Why ICD-10 Data Analytics?
ICD10monitor’s Talk Ten Tuesday Poll
June 25, 2013
Question
When is your organization planning to do its
coding data analytics to assess potential revenue
risk?
Percent
A:
We already have
25%
B:
By the end of 2013
39%
C:
Beginning of 2014
13%
D:
We are not doing it
9%
E:
What is data analytics?
14%
7
© 2014 Panacea Healthcare Solutions, Inc.
Why ICD-10 Data Analytics?
ICD10monitor’s Talk Ten Tuesday Poll
Repeated poll on May 20, 2014
Question
When is your organization planning to do its
coding data analytics to assess potential revenue
risk and develop focused documentation
education?
Percent
A:
We already have
38%
B:
Sometime in 2014
34%
C:
By June of 2015
12%
D:
We are not doing it
9%
E:
What is data analytics?
6%
8
© 2014 Panacea Healthcare Solutions, Inc.
Financial
ICD10monitor’s Talk Ten Tuesday Poll
July 2, 2013
Question
What financial impact results has your data
analytics revealed?
Percent
A:
Potentially less reimbursement under ICD-10
14%
B:
Potentially more reimbursement under ICD-10
5%
C:
Potentially remaining revenue neutral
17%
D:
Still have not done
50%
E:
Not applicable to my organization
14%
9
© 2014 Panacea Healthcare Solutions, Inc.
Financial
ICD10monitor’s Talk Ten Tuesday Poll
Repeated poll on February 25, 2014
Question
What financial impact results has your data
analytics revealed?
Percent
A:
Potentially less reimbursement under ICD-10
16%
B:
Potentially more reimbursement under ICD-10
6%
C:
Potentially remaining revenue neutral
19%
D:
Still have not done
38%
E:
Decided not to do it
2%
F:
Not applicable to my organization
19%
10
© 2014 Panacea Healthcare Solutions, Inc.
Why ICD-10 Data Analytics?
ICD10monitor’s Talk Ten Tuesday Poll
October 1, 2013
Question
With one year to go, what is your biggest risk area
for not being ready on October 1st, 2014?
Percent
A:
Claims submission
6%
B:
Payment / cash flow
13%
C:
Coding staff training / productivity
20%
D:
Physician documentation
47%
E:
System / software / tool updates
14%
11
© 2014 Panacea Healthcare Solutions, Inc.
Why ICD-10 Data Analytics?
ICD10monitor’s Talk Ten Tuesday Poll
October 29, 2013
Question
How engaged are your Physicians overall with ICD- Percent
10?
A:
High
4%
B:
Moderate
30%
C:
Low
44%
D:
None, they want another delay
9%
E:
Not applicable
13%
12
© 2014 Panacea Healthcare Solutions, Inc.
Why ICD-10 Data Analytics?
ICD10monitor’s Talk Ten Tuesday Poll
February 4, 2014
Question
When it comes to engaging Physicians at your
facility, are you customizing training that fits their
specialties?
Percent
A:
Yes we are taking this approach
61%
B:
We are considering this approach
13%
C:
We have not determined our approach
9%
D:
No we are not taking this approach
4%
E:
Not applicable
13%
13
© 2014 Panacea Healthcare Solutions, Inc.
Why ICD-10 Data Analytics?
ICD10monitor’s Talk Ten Tuesday Poll
September 10, 2013
Question
Do you have a CDI program?
Percent
A:
Yes, we’ve had it for years
50%
B:
Yes, we’ve recently set it up
16%
C:
No, but we are going to set it up
11%
D:
No and we don’t plan to
7%
E:
Not applicable
16%
14
© 2014 Panacea Healthcare Solutions, Inc.
Why ICD-10 Data Analytics?
ICD10monitor’s Talk Ten Tuesday Poll
September 17, 2013
Question
Is your Clinical Documentation Program (CDIP)
reviewing for ICD-10 yet?
Percent
A:
Yes
37%
B:
Not yet but planning to before end of 2013
16%
C:
Not yet but planning to start in 2014
17%
D:
We don’t have a CDIP
12%
E:
Not applicable
18%
15
© 2014 Panacea Healthcare Solutions, Inc.
CASE STUDY ICD-10 DATA
ANALYTICS RESULTS
Case Study ICD-10 Data Analytics
Results
• Perform an ICD-10 Documentation Audit to
assess the completeness of Physician
documentation to support ICD-10 code
assignment by natively coding in ICD-10.
(Inpatient, Outpatient and Physician records
were included).
• Perform an ICD-9 MS-DRG Validation Audit to
ensure that the estimated MS-DRG financial
impact is based on a correct ICD-9 starting MSDRG.
17
© 2014 Panacea Healthcare Solutions, Inc.
Case Study ICD-10 Data Analytics
Results
• Identify gaps and opportunities that are specific
to your documentation in ICD-10.
• Identify financial opportunities and risks based
upon MS-DRG assignment. (MS-DRG Grouper
v31 was used for the MS-DRG ICD-9 and MSDRG ICD-10 calculations)
18
© 2014 Panacea Healthcare Solutions, Inc.
Inpatient Case Study ICD-10 Data
Analytics Results
• Inpatient Case Study 1:
– IPPS Hospital
– 162 Med/Surg and 12 Specialty Beds
– 9,896 Annual Inpatient Discharges
• Audit Specifics:
– 400 inpatient charts were natively coded in ICD-10
– A data analytic tool was used to identify claims with potential
moderate to high risk based upon GEMS (General Equivalency
Maps) and a proprietary software alga rhythm
– Included a balance of top Physicians identified by the software
– Diagnoses and procedures that reflect high volume for potential
financial impact
– Included a balance of top MS-DRGs
19
© 2014 Panacea Healthcare Solutions, Inc.
Inpatient Case Study 1: Inpatient I-9 to ICD-10
MS-DRG Shift Estimated Financial Impact
MS-DRG Shift Change
Reason
# of Changes
Identified
% of Claims
Change
Estimated
Financial Impact
Principal Diagnosis Causing
DRG Shift
22
5.5%
($2,470)
Secondary Diagnosis Causing
DRG Shift
45
11.25%
($25,258)
Principal Procedure Causing
DRG Shift
36
9%
($25,010)
Principal Diagnosis and
Procedure Causing DRG
Shift
1
0.25%
$4,466
Incomplete Physician
Documentation
5
1.25%
($3,987)
Total Estimated Financial
Impact
109
($52,259)
20
© 2014 Panacea Healthcare Solutions, Inc.
Inpatient Case Study 1:
ICD-10 Diagnosis Coding Statistics
• A total of 4,564 ICD-10-CM diagnosis codes
were coded:
ICD-10 Reason Code
Number of
Codes
Percent
Specified code in ICD-10 assigned
3,527
77.3%
Unspecified code in ICD-10
assigned
1,027
22.5%
10
<1%
Could not be coded in ICD-10
21
© 2014 Panacea Healthcare Solutions, Inc.
Inpatient Case Study 1:
ICD-10 Procedure Coding Statistics
• A total of 693 ICD-10-PCS procedure codes
were coded:
ICD-10 Reason Code
Number of
Codes
Percent
670
96.7%
Unspecified code in ICD-10
assigned
3
<1%
Could not be coded in ICD-10
20
2.9%
Specified code in ICD-10 assigned
22
© 2014 Panacea Healthcare Solutions, Inc.
Inpatient Case Study ICD-10 Data
Analytics Results
• Inpatient Case Study 2:
– IPPS Hospital
– 235 Med/Surg and 75 Specialty Beds
– 20,137 Annual Inpatient Discharges
• Audit Specifics:
– 400 inpatient charts were natively coded in ICD-10
– A data analytic tool was used to identify claims with potential
moderate to high risk based upon GEMS (General Equivalency
Maps) and a proprietary software alga rhythm
– Included a balance of top Physicians identified by the software
– Diagnoses and procedures that reflect high volume for potential
financial impact
– Included a balance of top MS-DRGs
23
© 2014 Panacea Healthcare Solutions, Inc.
Inpatient Case Study 2: Inpatient I-9 to ICD-10
MS-DRG Shift Estimated Financial Impact
MS-DRG Shift Change
Reason
# of Changes
Identified
% of Claims
Change
Estimated
Financial Impact
Principal Diagnosis Causing
DRG Shift
33
8%
($35,139)
Secondary Diagnosis Causing
DRG Shift
32
8%
($38,917)
Principal Procedure Causing
DRG Shift
46
12%
$8,076
Principal Diagnosis and
Procedure Causing DRG
Shift
2
0.5%
$5,680
3
0.8%
$763
Incomplete Physician
Documentation caused the
MS-DRG shift
Total Estimated Financial
Impact
113
($59,537)
24
© 2014 Panacea Healthcare Solutions, Inc.
Inpatient Case Study 2:
ICD-10 Diagnosis Coding Statistics
• A total of 5,329 ICD-10-CM diagnosis codes
were coded:
ICD-10 Reason Code
Number of
Codes
Percent
Specified code in ICD-10 assigned
4,173
78.3%
Unspecified code in ICD-10
assigned
1127
21.1%
Not able to code in ICD-10
29
0.5%
25
© 2014 Panacea Healthcare Solutions, Inc.
Inpatient Case Study 2:
ICD-10 Procedure Coding Statistics
• A total of 1,333 ICD-10-PCS procedure codes
were coded:
ICD-10 Reason Code
Specified code in ICD-10 assigned
Unspecified code in ICD-10
assigned
Number of
Codes
Percent
1,284
96.3%
49
3.7%
26
© 2014 Panacea Healthcare Solutions, Inc.
Inpatient Case Study ICD-10 Data
Analytics Results
• Inpatient Case Study 3:
– IPPS Hospital
– 88 Med/Surg and 12 Specialty Beds
– 5,419 Annual Discharges
• Audit Specifics:
– 100 inpatient charts were natively coded in ICD-10
– A data analytic tool was used to identify claims with potential
moderate to high risk based upon GEMS (General Equivalency
Maps) and a proprietary software alga rhythm
– Included a balance of top Physicians identified by the software
– Diagnoses and procedures that reflect high volume for potential
financial impact
– Included a balance of top MS-DRGs
27
© 2014 Panacea Healthcare Solutions, Inc.
Inpatient Case Study 3: Inpatient I-9 to ICD-10
MS-DRG Shift Estimated Financial Impact
MS-DRG Shift Change
Reason
# of Changes
Identified
% of Claims
Change
Estimated
Financial Impact
Principal Diagnosis Causing
DRG Shift
10
10%
$7,796
Secondary Diagnosis Causing
DRG Shift
9
9%
($16,685)
Principal Procedure Causing
DRG Shift
8
8%
$26,971
Incomplete Physician
Documentation caused the
MS-DRG shift
2
2%
$0
Total Estimated Financial
Impact
29
$18,082
28
© 2014 Panacea Healthcare Solutions, Inc.
Inpatient Case Study 3:
ICD-10 Diagnosis Coding Statistics
• A total of 1,209 ICD-10-CM diagnosis codes
were coded:
ICD-10 Reason Code
Number of
Codes
Percent
Specified code in ICD-10 assigned
989
82%
Unspecified code in ICD-10
assigned
220
18%
29
© 2014 Panacea Healthcare Solutions, Inc.
Inpatient Case Study 3:
ICD-10 Procedure Coding Statistics
• A total of 200 ICD-10-PCS procedure codes
were coded:
ICD-10 Reason Code
Specified code in ICD-10 assigned
Unspecified code in ICD-10
assigned
Number of
Codes
Percent
193
97%
7
3%
30
© 2014 Panacea Healthcare Solutions, Inc.
Physician Case Study ICD-10 Data
Analytics Results
• Physician Case Study 1:
– OPPS Hospital
– 36 Hospital-based Clinics
• Audit Specifics:
– 290 physician encounters (original plan was 600)
– Diagnosis focus only
– A data analytic tool was used to identify claims with potential
primary code movement based upon GEMS (General
Equivalency Maps) and a proprietary software alga rhythm
– Include a balance of top Physicians identified by the software
– Include a sample of high volume specialties identified by the
software
– Include “unspecified” codes
31
© 2014 Panacea Healthcare Solutions, Inc.
Physician Case Study 1:
ICD-10-CM Physician Audit Results
• 967 ICD-10 diagnosis codes were coded:
ICD-10 Reason Code
Percent
Specified code in ICD-10 assigned
63%
Unspecified code in ICD-10 assigned
36%
Could not be coded in ICD-10
1%
© 2014 Panacea Healthcare Solutions, Inc.
Physician Case Study 1:
Physician Trends by ICD-10-CM Chapter
• Chapters with the highest percentage of specified
codes:
Chapter
Infectious Disease
Injuries and Poisoning
Factors Influencing
Health Factors (Z-Codes)
ICD-10-CM
Specified
Code
83%
84%
88%
© 2014 Panacea Healthcare Solutions, Inc.
Specialties
Impacted
FP
FP
Endo, FP, IM, Pulm,
Rheum
Physician Case Study 1:
Physician Trends by ICD-10-CM Chapter
• Chapters with the lowest percentage of specified
codes:
Chapter
Skin
Neurology
Respiratory
Mental Health
Obstetrics
ICD-10-CM
Specified Code
37%
42%
43%
45%
50%
© 2014 Panacea Healthcare Solutions, Inc.
Specialties
Impacted
FP, IM
FP, IM, Sleep
FP, IM, Pulmonology
FP, IM, Psych
OB
Physician Case Study1:
Physician ICD-10-CM Trends by Specialty
Specialty
Pulmonology
Endocrinology
Cardiology
Obstetrics
Family Practice
Rheumatology
Internal Medicine
Sleep Medicine
Psychiatry
Percentage
Specified
83%
80%
78%
67%
62%
61%
57%
44%
30%
© 2014 Panacea Healthcare Solutions, Inc.
TOP ICD-10 DIAGNOSIS
DOCUMENTATION CONCEPTS
ICD-10-CM Diagnosis Concept 1: Sepsis
• Background: In ICD-9-CM, two codes are required to
report the diagnosis of sepsis (septicemia, 038.9 and
sepsis 995.91 or severe sepsis, 995.92 dependent upon
with or without organ dysfunction). An additional code is
also assigned for septic shock (severe sepsis). In ICD10, a diagnosis of sepsis unspecified is assigned as
A41.9. An additional code is assigned for severe sepsis
or an associated acute organ dysfunction noted. Severe
sepsis is classified as with or without septic shock.
• Specialties Most Affected: Hospitalist, Internal
Medicine, Infectious Disease
37
© 2014 Panacea Healthcare Solutions, Inc.
ICD-10-CM Diagnosis Concept 1: Sepsis
• Finding: The review showed sufficient documentation of
sepsis present in about half of the records reviewed.
• Recommendation: In ICD-10, the physician must still
continue to document the disorder of sepsis, as well as
acute organ dysfunction (severe sepsis) if applicable.
Documentation of septic shock is still needed if
appropriate. The causative organism along with the
source of the sepsis such as pneumonia, urinary tract
infection, cellulitis, post-procedural ,etc. needs to be
documented as well. Sepsis should also be clearly
documented regarding present on admission status.
38
© 2014 Panacea Healthcare Solutions, Inc.
ICD-10-CM Diagnosis Concept 2:
Neoplasm
•
Background: Although ICD-10 allows for an unspecified site, the code
set expands malignant neoplasms of most body organs/systems to
specific sites requiring documentation of the specific site and laterality.
•
Specialties Most Affected: Hospitalist, Internal Medicine, Oncology
•
Finding: Neoplasm documentation was not sufficient in some of the
records reviewed to be able to code to a specific location of the
neoplasm, most notably colon, stomach, lung, kidney, bladder and
breast.
•
Recommendation: The provider must document the specific location
of the neoplasm as well as the laterality--primary or metastatic. In ICD10 many of the organs have been expanded to include more specific
locations within that organ. For example, lung has been expanded to
include the laterality and region (upper/middle/lower) for the neoplasm.
39
© 2014 Panacea Healthcare Solutions, Inc.
ICD-10-CM Diagnosis Concept 3: Anemia
• Background: The coding guidelines for anemia have been
revised for ICD-10.
– ICD-10 Guideline, Chapter 2 c. 1: When the admission is for
management of the anemia associated with malignancy or a
chronic disease, and the treatment is only for the anemia, the
diagnosis code for the malignancy or chronic disease is
sequenced as the principal diagnosis followed by the appropriate
code for the anemia.
– ICD-9 Guideline not present in ICD-10: If anemia in neoplastic
disease and anemia due to antineoplastic chemotherapy are
both documented, assign codes for both conditions.
– ICD-10: Anemia due to chemotherapy and anemia in neoplastic
disease have excludes 1 notes.
40
© 2014 Panacea Healthcare Solutions, Inc.
ICD-10-CM Diagnosis Concept 3: Anemia
• Specialties Most Affected: Hospitalist, Internal Medicine,
Oncology, Hematology
• Finding: The MS-DRG assignment is revised for those patients
admitted due to anemia of chronic disease. Clarification is needed
regarding anemia due to chemotherapy vs. anemia due to
neoplastic disease due to the excludes 1 note.
• Recommendation: Documentation by the physician is needed to
clearly state the specificity of the anemia, such as anemia due to
neoplasm or chronic kidney disease. The specificity of the anemia
is essential for appropriate code assignment.
41
© 2014 Panacea Healthcare Solutions, Inc.
ICD-10-CM Diagnosis Concept 4:
Thrombocytopenia
• Background: As in ICD-9, thrombocytopenia can be further
specified such as primary, secondary, idiopathic, due to drugs,
etc.
• Specialties Most Affected: Hospitalist, Internal Medicine,
Hematology
• Findings: Many of the records reviewed did not contain the
specificity of the thrombocytopenia.
• Recommendation: Providers should document the
specificity of thrombocytopenia to appropriately classify this
disorder. The specificity of thrombocytopenia may be
considered a CC status diagnosis.
42
© 2014 Panacea Healthcare Solutions, Inc.
ICD-10-CM Diagnosis Concept 5:
Diabetes
•
Background: ICD-10 has expanded its diabetes mellitus to include
combination codes which include the manifestation; therefore, coding
multiple codes is no longer required. However, documentation of the
manifestation is required to select the principal diagnosis. Diabetes noted
as out of control, poorly controlled, or inadequately controlled denotes
diabetes with hyperglycemia.
•
Specialties Most Affected: Hospitalist, Internal Medicine
•
Finding: The review showed that most diabetes codes were documented
appropriately. There were a few in which the documentation could have
been more specific.
•
Recommendation: Providers should continue to document the type of
Diabetes as Type I or Type 2 and the specific manifestations. Diabetic
ulcers require additional documentation to identify the depth of the ulcer
(e.g., breakdown of skin, fat). Physicians should continue to document
hyper- and hypoglycemia.
43
© 2014 Panacea Healthcare Solutions, Inc.
ICD-10-CM Diagnosis Concept 6:
Malnutrition
• Background: As in ICD-9 malnutrition can be further
specified to the degree such as mild, moderate, or
severe protein-calorie malnutrition.
• Specialties Most Affected: Hospitalist, Internal
Medicine
• Finding: Many of the records reviewed only had
documentation of unspecified malnutrition.
• Recommendation: Malnutrition should be specified to
the appropriate degree such as mild, moderate, or
severe protein-calorie with or without marasmus and/or
kwashiorkor. The specificity of malnutrition can affect the
MCC/CC status of this diagnosis.
44
© 2014 Panacea Healthcare Solutions, Inc.
ICD-10-CM Diagnosis Concept 7:
Drug Dependence
• Background: Drug dependence in ICD-10 is no longer
classified as unspecified, continuous or episodic use.
Drug dependence is specified with disorders such as
intoxication, mood, psychotic, sleep, etc. Remission
status is still a classification. Drug dependence,
uncomplicated, such as opioid, is now considered a CC
status diagnosis. Drug use and abuse are also now
separately identified.
• Specialties Most Affected: Hospitalist, Internal
Medicine, Psychiatry
45
© 2014 Panacea Healthcare Solutions, Inc.
ICD-10-CM Diagnosis Concept 7:
Drug Dependence
• Finding: Many of the records reviewed were related to
opioid dependence and triggered MS DRG status
changes due to the CC status change.
• Recommendation: Documentation by the physician
should clearly note the specific drug and classification of
use, abuse, dependence, or in remission. Also any
associated disorders should be clearly noted. The
specificity of use, abuse, dependence, or remission may
affect the CC status of the diagnosis.
46
© 2014 Panacea Healthcare Solutions, Inc.
ICD-10-CM Diagnosis Concept 8:
Depression/Major Depressive Disorder
• Background: Documentation for depressive disorders in
ICD-10 requires inclusion of the type of episode (recurrent,
in remission, or single episode), degree of severity (mild,
moderate, severe) and with psychotic features if applicable.
If in remission, the provider must state “in remission” as this
cannot be inferred. If the patient is in remission, the
provider must also state whether it is partial or full
remission. Depression not otherwise specified is now
classified as major depressive disorder, single episode.
• Specialties Most Affected: Hospitalist, Internal Medicine,
Emergency Medicine, Psychiatry
47
© 2014 Panacea Healthcare Solutions, Inc.
ICD-10-CM Diagnosis Concept 8:
Depression/Major Depressive Disorder
• Finding: The review showed that many of the depression
codes did not provide the type, severity or status of the
depression.
• Recommendation: The provider should document the
type of depression, single vs. recurrent, degree of severity,
and document if associated conditions and/or complications
are present. If the patient is in remission, this must be
documented and cannot be inferred. Major depressive
disorder, single, with at least mild severity is considered a
CC status diagnosis. Major depressive disorder, recurrent,
is also considered a CC status diagnosis.
48
© 2014 Panacea Healthcare Solutions, Inc.
ICD-10-CM Diagnosis Concept 9:
Myocardial Infarction
• Background: There have been coding guideline changes
associated with myocardial infarction diagnosis and the physician
must provide specificity as to the site, type, and age of the
myocardial infarction. There are changes to the subsequent AMI
coding guideline in ICD-10. A code for subsequent AMI is to be
used when a patient has suffered a new AMI within a four week time
period of the initial AMI.
• ICD-10 Guideline, Chapter 9 e. 1): For encounters occurring while
the myocardial infarction is equal to, or less than, four weeks old,
including transfers to another acute setting or a post-acute setting,
and the patient requires continued care for the myocardial infarction,
codes from category I21 may continue to be reported.
49
© 2014 Panacea Healthcare Solutions, Inc.
ICD-10-CM Diagnosis Concept 9:
Myocardial Infarction
• Specialties Most Affected: Hospitalist, Internal Medicine,
Cardiology
• Finding: The review showed that many of the records had
adequate documentation of the age of the MI as well as location.
• Recommendation: Recommend that documentation of the
myocardial infarction continue to be specified as to the site, type and
date of the acute infarction. This would also include patients that
are transferred to this hospital so that the correct coding can be
applied based on the coding guideline change. It is recommended
that documentation of AMI continue to be specific as to the type of
acute or subsequent acute, and clearly document the date of the
AMI so the coding professional can determine if this is a new AMI,
an AMI within the four week period, including transfers, and the
patient requires continue care, or a new AMI within the four week
time period from an initial AMI.
50
© 2014 Panacea Healthcare Solutions, Inc.
ICD-10-CM Diagnosis Concept 10:
Atrial Fibrillation
• Background: Atrial fibrillation has been expanded in ICD-10 to
include the type of atrial fibrillation. The new documentation
elements include paroxysmal, persistent, and chronic.
• Specialties Most Affected: Hospitalist, Internal Medicine,
Cardiology
• Finding: Many of the records reviewed did not contain
documentation of the type of atrial fibrillation.
• Recommendation: Providers should review new documentation
elements for category I48, Atrial Fibrillation. To code a specified
code, documentation should include chronic, persistent or
paroxysmal. Persistent atrial fibrillation is considered a CC status
diagnosis.
51
© 2014 Panacea Healthcare Solutions, Inc.
ICD-10-CM Diagnosis Concept 11:
Hypertension
•
Background: Hypertension as identified in ICD-9 is classified as either
accelerated/malignant or benign. In ICD-10 the classification will only
consist of one code and include both benign and accelerated/malignant.
Accelerated/malignant is now considered a non-essential modifier and no
longer a CC status diagnosis.
•
Specialties Most Affected: Hospitalist, Internal Medicine, Cardiology,
Emergency Medicine
•
Finding: A few of the records reviewed contained documentation of
accelerated/malignant hypertension which is no longer recognized as a CC
status diagnosis.
•
Recommendation: Providers should be encouraged to continue to
document the type of hypertension as determined during the treatment of
the patient. If there is a cause and effect relationship with hypertension and
other disorders such as heart disease or cardiorenal disease these should
continue to be documented as well.
52
© 2014 Panacea Healthcare Solutions, Inc.
ICD-10-CM Diagnosis Concept 12:
Heart Block
•
Background: As in ICD-9, the specificity and degree of the heart block
should be clearly documented. AV block type II is no longer considered a
CC status diagnosis in ICD-10. However, there is a classification change in
ICD-10 regarding bundle branch blocks with fascicular block that may result
in a CC status diagnosis.
•
Specialties Most Affected: Hospitalist, Internal Medicine, Cardiology
•
Findings: As a result of the coding change, a record was found to have a
CC status change with the AV block type II no longer being a CC.
•
Recommendation: Documentation of heart block specificity such as
atrioventricular, bundle branch, bifascicular, etc. should be clearly noted
along with the degree such as first, second, third, etc. for accurate and
complete code assignment. The specificity of the heart block may affect the
MS DRG assignment in ICD-10 coding.
53
© 2014 Panacea Healthcare Solutions, Inc.
ICD-10-CM Diagnosis Concept 13:
Congestive Heart Failure
•
Background: Like in ICD-9, in order to code congestive heart failure to the
highest level of specificity, providers must document whether the heart
failure is left ventricular, systolic, diastolic or combined. In addition, the
documentation should state acute, chronic or acute on chronic. ICD-10 has
a combination code for congestive heart failure noted as systolic, diastolic
or combined. A secondary code of congestive heart failure is no longer
required as congestive is considered a non-essential modifier with the
specificity.
•
Specialties Most Affected: Hospitalist, Internal Medicine, Cardiology,
Emergency Medicine
•
Findings: Many of the records reviewed contained documentation as to
the type of acuity of congestive heart failure.
•
Recommendation: Providers should continue to document the acuity
(acute, chronic or acute on chronic) and type (diastolic, systolic or
combined) of heart failure. Also linking any related or underlying conditions
such as hypertensive heart disease or cardiomyopathy is also needed.
54
© 2014 Panacea Healthcare Solutions, Inc.
ICD-10-CM Diagnosis Concept 14:
Pulmonary Embolism/Acute Cor Pulmonale
• Background: Pulmonary embolism has been expanded in ICD-10
to now include the option of this condition with acute cor pulmonale
as a combination code. The type of embolism such as septic or
saddle should also be documented as well. If the pulmonary
embolism is a complication of a procedure, clear documentation of
this relationship needs to be noted.
• Specialties Most Affected: Hospitalist, Internal Medicine, Surgery,
Cardiology
• Findings: Acute cor pulmonale was documented on a few of the
records and with the conversion to ICD-10 coding the acute
condition is now classified with pulmonary embolism rather than
classified separately.
55
© 2014 Panacea Healthcare Solutions, Inc.
ICD-10-CM Diagnosis Concept 14:
Pulmonary Embolism/Acute Cor Pulmonale
• Recommendation: Providers should continue to clearly identify the
acuity of the pulmonary embolism (acute, chronic or history of) as
well as the acuity of cor pulmonale (acute or chronic).
Documentation of the underlying cause of the pulmonary embolism
is necessary and if the embolism is a complication of a procedure,
the cause and effect must be clearly noted. The MS DRG is
affected due to the principal diagnosis of acute cor pulmonale and
pulmonary embolism if specified as a complication of a procedure.
56
© 2014 Panacea Healthcare Solutions, Inc.
ICD-10-CM Diagnosis Concept 15:
Cerebral Infarction
• Background: ICD-10 has greatly expanded the category of
cerebral infarctions to include the exact site of the infarction,
laterality and whether or not it is a thrombosis, an embolism ,or
hemorrhage that has caused the infarction.
• Specialties Most Affected: Hospitalist, Internal Medicine,
Neurology
• Findings: A few of the records review did contain documentation of
the exact site of the cerebral infarction.
• Recommendation: Providers should continue to document the
exact site of the cerebral infarction (vertebral, carotid, basilar,
cerebral etc.), laterality, the specific vessel in which the infarction
occurred and whether or not it is thrombotic, embolic ,or
hemorrhagic in nature.
57
© 2014 Panacea Healthcare Solutions, Inc.
ICD-10-CM Diagnosis Concept 16:
COPD/Bronchitis/Asthma
•
Background: ICD-9 has multiple codes to reflect COPD noting if the
patient is in acute exacerbation, whether it is due to other obstruction
conditions and if the disorder is associated with bronchitis, asthma
emphysema, etc.
•
Bronchitis has been expanded to facilitate identification of secondary
disease processes, specific manifestations or associated complications in
ICD-10. Chronic bronchitis can also be further defined to include specificity
such as asthmatic, obstructive, purulent, etc.
•
ICD-10 expands asthma to include severity (mild, moderate and severe) as
well as intermittent or persistent. New guidelines now require an additional
code for tobacco use and/or exposure, if applicable.
•
Specialties Most Affected: Hospitalist, Internal Medicine, Pulmonary,
Pediatrics, Emergency Medicine
58
© 2014 Panacea Healthcare Solutions, Inc.
ICD-10-CM Diagnosis Concept 16:
COPD/Bronchitis/Asthma
• Findings: Many of the records reviewed did not state whether
the patient was in acute exacerbation or any other type of
obstructive condition with the documentation of COPD.
• Many of the bronchitis codes reviewed did not contain the
specificity needed to be able to code further than unspecified
bronchitis in ICD-10. Chronic bronchitis was documented but no
further specificity as to whether it was obstructive, asthmatic, etc.
• Many of the records reviewed did not specify the severity of the
asthma.
59
© 2014 Panacea Healthcare Solutions, Inc.
ICD-10-CM Diagnosis Concept 16:
COPD/Bronchitis/Asthma
• Recommendation: Providers should continue to clearly document
the type of obstructive disease with the diagnosis of COPD and if
the patient is in acute exacerbation.
• Providers should continue to document the causative organism
(when known) for acute bronchitis so that further classification can
be coded. Chronic bronchitis should be further specified, if known,
to include asthmatic, obstructive, purulent, etc.
• Providers should document severity and state intermittent or
persistent as well as any exacerbation or status asthmaticus.
Additionally, tobacco use or exposure is now a required
documentation element for asthma if applicable.
60
© 2014 Panacea Healthcare Solutions, Inc.
ICD-10-CM Diagnosis Concept 17:
Hepatitis/Hepatic Encephalopathy
•
Background: As in ICD-9, codes for hepatitis in ICD-10 specify whether
the condition is acute or chronic and whether it is with or without hepatic
coma.
•
Hepatic encephalopathy has been expanded in ICD-10 to include acuity
(acute/chronic) and whether it is with or without coma.
•
Specialties Most Affected: Hospitalist, Internal Medicine, Gastroenterology
•
Findings: Some of the records reviewed did not have documentation of
whether the hepatitis was acute or chronic. The type of hepatitis (A, B, C)
was documented. Some of the records did not document the acuity or if the
patient was with or without coma.
•
Recommendation: Providers should continue to document the type of
hepatitis as well as the acuity of this condition. Providers should also
continue to document the type of encephalopathy and include the acuity
and if it is with or without coma. The specificity of with or without coma
affects the MCC/CC status of this diagnosis.
61
© 2014 Panacea Healthcare Solutions, Inc.
ICD-10-CM Diagnosis Concept 18:
Skin Ulcer
•
Background: ICD-10 coding for decubitus/pressure ulcer diagnosis is
identified by one combination code which specifies the site of the ulcer and
the stage of the ulcer instead of two codes that were needed in the ICD-9
classification.
•
Specialties Most Affected: Hospitalist, Internal Medicine, Surgery
•
Findings: Some of the records reviewed did not specify the depth or type
of breakdown that was present on non-pressure ulcers..
•
Recommendation: Providers must document the specific type, site and
stage of the pressure ulcers. Distinct documentation of the present on
admission status must also accompany any type of pressure ulcer
documentation as this can be considered a hospital acquired condition.
With non-pressure ulcers, documentation must include the location of the
ulcer, laterality and the level of involvement to include breakdown of skin,
with fat layer exposed, with necrosis of muscle and with necrosis of bone.
62
© 2014 Panacea Healthcare Solutions, Inc.
ICD-10-CM Diagnosis Concept 19:
Chronic Kidney Disease
•
Background: As in ICD-9, chronic kidney disease can be further specified
as stage 1 through 5 or end stage renal disease. If hypertension is also
specified, an additional code is assigned for hypertensive chronic kidney
disease.
•
Specialties Most Affected: Nephrology, Internal Medicine, Hospitalist,
Urology
•
Findings: Many of the records reviewed did not have the stage of the
chronic kidney disease documented.
•
Recommendation: Physician documentation should be specific to identify
the stage of the chronic kidney disease or end stage renal disease. The
stage of chronic kidney disease or end stage renal disease reflects the
severity of this disorder. The stage of chronic kidney disease can also affect
the MCC/CC status of the diagnosis.
63
© 2014 Panacea Healthcare Solutions, Inc.
ICD-10-CM Diagnosis Concept 20:
Urinary Retention
• Background: Urinary retention in I-10 now includes if it is drug
induced. The additional code for adverse effect, if applicable, to
identify the drug is also coded.
• Specialties Most Affected: Hospitalist, Internal Medicine, Urology
• Findings: The records reviewed did not document the type of
urinary retention.
• Recommendation: Physician documentation should include the
specificity of urinary retention such as due to hyperplasia of the
prostate, psychogenic, organic or drug induced. The additional code
to identify the drug for adverse effect, if applicable, should also be
documented.
64
© 2014 Panacea Healthcare Solutions, Inc.
TOP ICD-10 PROCEDURE
DOCUMENTATION CONCEPTS
ICD-10 Procedure Concept 1:
Debridement
• Background: Excisional debridement of skin and subcutaneous
tissues in ICD-10 is classified as separate body systems vs. the
same classification when compared to ICD-9 coding. The body part
is also site specific and includes laterality of right and/or left when
applicable. There are also approach options for the subcutaneous
tissues and qualifier of diagnostic, if appropriate.
• Specialties Most Affected: Surgery, Wound Care, Hospitalists,
Emergency Medicine, Internal Medicine
• Findings: Some of the records reviewed did not contain
documentation as to whether the debridement was excisional or
non-excisional, to what level of tissue was debrided and site where
the debridement took place.
66
© 2014 Panacea Healthcare Solutions, Inc.
ICD-10 Procedure Concept 1:
Debridement
• Recommendation: Physician documentation for debridement
must be specific to the body system involved (skin,
subcutaneous tissue, fascia, muscle, bone, etc.) and to the
specific body part undergoing the debridement procedure. The
approach must be noted as to whether it is open or percutaneous
per the ICD-10 definitions. Laterality of right or left is also
necessary. If the procedure is diagnostic in nature this needs to
be documented as well. The specificity of the procedure can
affect the MS DRG assignment.
67
© 2014 Panacea Healthcare Solutions, Inc.
ICD-10 Procedure Concept 2:
Incision & Drainage
•
Background: ICD-10 has separate body systems for skin and
subcutaneous tissue. Along with specifying the depth of the incision, the
specific body part (scalp, face, ear, neck, chest, back, abdomen, buttock,
perineum, genitalia, arm, hand, leg, foot, nail, breast, nipple) and the
laterality of that body part must be documented.
•
Specialties Most Affected: Surgery, Emergency Medicine, Hospitalists,
Internal Medicine
•
Findings: Some of the records reviewed did not contain the depth of
incision.
•
Recommendation: Physician documentation will need to specify the depth
of the incision, the specific body part (skin vs. subcutaneous tissue),
laterality and if any drainage device was left in place to adequately code
these procedures in ICD-10. The specificity of the procedure can affect the
MS DRG assignment.
68
© 2014 Panacea Healthcare Solutions, Inc.
ICD-10 Procedure Concept 3:
Amputation
•
Background: ICD-10 classifies amputation to the root operation of
“Detachment” and further defines the body part in which the amputation is
being performed on. Laterality and the level of the procedure being
performed and noting whether the amputation is of a high, mid or low in
nature is important in classifying these procedures.
PCS Reference Manual: Upper arm and upper leg
– Qualifier 1 High: Amputation at the proximal portion of the shaft of the
humerus or femur
– Qualifier 2 Mid: Amputation at the middle portion of the shaft of the
humerus or femur
– Qualifier 3 Low: Amputation at the distal portion of the shaft of the
humerus or femur
69
© 2014 Panacea Healthcare Solutions, Inc.
ICD-10 Procedure Concept 3:
Amputation
• Specialties Most Affected: Orthopedics, Vascular Surgery
• Findings: Some of the records reviewed did not contain the
level of the amputation and could not be coded due to this
missing documentation.
70
© 2014 Panacea Healthcare Solutions, Inc.
ICD-10 Procedure Concept 4:
Banding of Esophageal Varices
• Background: ICD-10 is specific to the objective or root operation of
the procedure, body part and device along with the approach for the
procedure of EGD with banding of esophageal varices.
• Specialties Most Affected: Gastroenterology
• Findings: Two MS DRG changes were identified as a result of this
procedure.
• Recommendation: Continue to document the objective or root
operation of the procedure (i.e., occlusion), approach, body system
and body part of lower vein, esophageal, and device (band). This is
currently considered a procedure that affects MS DRG assignment.
Also reference AHA Coding Clinic 4th Quarter 2013, page 112 – 113
for details.
71
© 2014 Panacea Healthcare Solutions, Inc.
ICD-10 Procedure Concept 5:
AV Fistula Thrombectomy
• Background: ICD-10 is specific to the section or general type of the
procedure, body system, objective or root operation of the
procedure, body part, approach, device and qualifier for the
procedure for thrombectomy of AV fistula.
• Specialties Most Affected: Vascular Surgery
• Findings: The artery or vein that the procedure was being
performed in was not documented.
• Recommendation: Specific documentation is needed to describe
the thrombectomy procedure of the AV fistula to include
thrombectomy of the artery/vein involved. The specific artery such
as brachial or radial, and/or vein such as basilica or brachial is also
required. Laterality of right and left is also specified in the body part.
72
© 2014 Panacea Healthcare Solutions, Inc.
ICD-10 Procedure Concept 6:
Revision of Joint Replacement
•
Background: Revision of joint procedures in ICD-10 now require two
codes, one for the removal of the previous prosthesis material and one
for the replacement. The approach, laterality, specific component, and
substitute material along with the specificity of it being cemented or
uncemented are now required.
•
Specialties Most Affected: Orthopedics
•
Findings: The documentation of the type material inserted was not
able to be located.
•
Recommendation: Physician documentation must include the specific
joint components being replaced, laterality, approach, substitute
materials and whether these components are cemented or
uncemented. The joint procedures currently can cause movement in
the ICD-10 MS DRG assignment; however, it appears to be an error in
the grouping logic.
© 2014 Panacea Healthcare Solutions, Inc.
73
ICD-10 Procedure Concept 7:
Bowel Procedures
• Background: In ICD-10, procedures on the bowel now must include
the specific portion of the bowel that the procedure is being
performed on. For the large bowel this would include the specific
parts of sigmoid, ascending colon, descending colon, transverse
colon, rectum, etc. For the small bowel this would include the
specific parts of jejunum, duodenum, ileum, etc. Documentation
must also include whether all (resection) or a portion of the body
part (excision) is being removed as the root operation is different
depending on all or a portion of the specified bowel. Documentation
of the approach is also needed to know whether it was open,
percutaneous endoscopic, etc.
• Specialties Most Affected: Surgery
74
© 2014 Panacea Healthcare Solutions, Inc.
ICD-10 Procedure Concept 7:
Bowel Procedures
• Findings: The documentation of the specific area in which the
procedure was being performed was not readily identifiable in all
cases reviewed.
• Recommendation: Physician documentation must be specific
as to which portion of the small or large bowel the procedure is
being performed on, whether all or a portion of the bowel is being
removed and the approach of the procedure. The specific site of
the procedure in the large or small bowel may have an effect on
the MS DRG assignment for the case.
75
© 2014 Panacea Healthcare Solutions, Inc.
ICD-10 Procedure Concept 8:
Lysis of Adhesions
• Background: In ICD-9, lysis of adhesions was represented by one
procedure code, i.e. intestine. In ICD-10 this procedure is now
coded to the specific location of the adhesions and the number of
code possibilities has dramatically increased. The physician also
needs to document the approach that was taken to correctly code
these procedures.
• Specialties Most Affected: Surgery, Gynecology
• Findings: The documentation of the specific area in which the
procedure was performed was present in most of the records
reviewed.
• Recommendation: Physician documentation must be specific for
the location of the lysis of adhesions so that the appropriate
procedure can be coded. The approach should also be
documented. This procedure may affect the MS DRG assignment.
76
© 2014 Panacea Healthcare Solutions, Inc.
ICD-10 Procedure Concept 9:
PTCA
• Background: Coding guidelines have changed in ICD-10 for the
coding of PTCA procedures. ICD-9 referenced the number of
coronary vessels treated. ICD-10 guidelines now specify the
number of sites treated rather than the name or number of arteries.
• ICD-10-PCS Guideline, B4.4: The coronary arteries are classified
as a single body part that is further specified by number of sites
treated and not by name or number of arteries. Separate body part
values are used to specify the number of sites treated when the
same procedure is performed on multiple sites in the coronary
arteries.
77
© 2014 Panacea Healthcare Solutions, Inc.
ICD-10 Procedure Concept 9:
PTCA
•
•
•
Examples: Angioplasty of two distinct sites in the left anterior descending
coronary artery with placement of two stents is coded as Dilation of
Coronary Arteries, Two Sites, with Intraluminal Device.
Angioplasty of two distinct sites in the left anterior descending coronary
artery, one with stent placed and one without, is coded separately as
Dilation of Coronary Artery, One Site with Intraluminal Device, and Dilation
of Coronary Artery, One Site with no device.
Specialties Most Affected: Cardiology
Findings: The documentation of the number of sites treated was present in
most of the records reviewed.
Recommendation: Physician documentation needs to describe the details
of the procedure performed as well as the number of site treated and the
types of stents inserted. Panacea recommends a dictated procedure note
in addition to the signed catheterization procedure log.
78
© 2014 Panacea Healthcare Solutions, Inc.
ICD-10 Procedure Concept 10:
Coronary Arteriogram
•
Background: ICD-10 requires the coding of the type of contrast material
used to be included into the code selection.
•
Specialties Most Affected: Cardiology
•
Findings: Documentation of the type of contrast was present on the heart
catheterization log but was not adequately documented to know what type
of contrast (high or low osmolar) was administered. An internet search had
to be performed to know whether this was high or low osmolar contrast to
code these procedures correctly.
•
Recommendation: Documentation should be evaluated to determine how
to easily have the coding professional be able to know whether high or low
osmolar contrast was administered without an impact on coding productivity
as this is now a required component of the code.
79
© 2014 Panacea Healthcare Solutions, Inc.
ICD-10 Procedure Concept 11:
Bronchoscopy
• Background: ICD-10 is specific to the section or general type of
the procedure, body system, objective or root operation of the
procedure, body part, approach, device and qualifier for
bronchoscopy with procedures such as biopsy, BAL, removal of
mucous plug, etc.
• Specialties Most Affected: Pulmonology
• Findings: MS DRG changes were noted in the review as a
result of mucous plug being removed as well as BAL procedures.
80
© 2014 Panacea Healthcare Solutions, Inc.
ICD-10 Procedure Concept 11:
Bronchoscopy
• Recommendation: Physician documentation is critical to
describe the multiple procedures performed during bronchoscopy
such as biopsy of bronchus or lung, BAL, removal of mucous
plug, etc. The site specificity of each procedure performed, such
as bronchus or lung, upper or lower, or right or left is essential to
accurately code all procedures performed. The objective or root
operation of each procedure can be described as excision,
drainage or extirpation to denote multiple procedures performed
during the bronchoscopy procedure. The specific procedures
performed can affect the MS-DRG assignment.
81
© 2014 Panacea Healthcare Solutions, Inc.
ICD-10 Procedure Concept 12:
Obstetrical Procedures
•
Background: ICD-10 is specific to the section or general type of procedure,
body system, objective or root operation of the procedure, body part,
approach, device and qualifier for manual removal of retained placenta and
for repair of obstetrical lacerations. Procedures performed on the products
of conception are coded to the Obstetrics section.
•
Specialties Most Affected: Obstetrics
•
Findings: DRG changes were noted when the removal of a retained
placenta was performed or when the patient had a 3rd or 4th degree perineal
laceration repaired during delivery.
•
Recommendation: Documentation by the physician should include the
approach used, via natural or artificial opening or with an endoscope, for the
extraction of the retained products of conception and the repair of
obstetrical lacerations. Currently these are considered procedures that
affect the MS-DRG assignment.
82
© 2014 Panacea Healthcare Solutions, Inc.
ICD-10 Procedure Concept 13:
Central Line
• Background: ICD-10 is specific to the section or general type of the
procedure, body system, objective or root operation of the
procedure, body part, approach, device and qualifier for the
placement of a central line.
• Specialties Most Affected: Internal Medicine, Hospitalist
• Findings: ICD-10 requires coding where the catheter tip resides.
This was very difficult to locate in many of the records in which
central lines were placed.
• Recommendation: Physician documentation must include where
the catheter tip resides such as superior vena cava, right atrium,
subclavian vein and the approach that was used to place the device.
The site specificity can affect the MS DRG assignment. Reference
AHA Coding Clinic Third Quarter 2013, page 18.
83
© 2014 Panacea Healthcare Solutions, Inc.
ICD-10 Procedure Concept 14:
EGD with Biopsy
• Background: ICD-10 is specific to the section or general type of the
procedure, body system, objective or root operation of the
procedure, body part, approach, device and qualifier for the EGD
with biopsy procedure.
• Specialties Most Affected: Gastroenterology
• Findings: The site of the biopsy in the esophagus was not
documented.
• Recommendation: The documentation should specify the exact
location of the biopsy procedure performed such as upper, middle,
lower or esophagogastric junction. Continue to document the
approach of the procedure.
84
© 2014 Panacea Healthcare Solutions, Inc.
ICD-10 Procedure Concept 15:
Suture of Skin/Tissue
•
Background: ICD-10 has separate body systems for skin and
subcutaneous tissue vs. the same classification when compared to
ICD-9 coding. The body part is also site specific and includes laterality
of right and/or left when applicable. There are also approach options as
well.
•
Specialties Most Affected: Emergency Medicine, General Surgery,
Hospitalist, Internal Medicine
•
Findings: The specific depth of the tissue repaired was not
documented.
•
Recommendation: It is essential that the documentation is specific to
the depth of tissue being repaired such as skin, subcutaneous, fascia,
muscle, etc. along with the specific body site of the repair documented.
Repair of the subcutaneous tissue and/or fascia can affect the MS DRG
assignment.
85
© 2014 Panacea Healthcare Solutions, Inc.
ABOUT 16-MONTHS TO
GO……..WHERE DO WE FOCUS?
Working With Physicians
• Address medical record documentation from an
EHR perspective (what is and isn’t needed
anymore, update bylaws)
• Address discharge summary and operative note
writing
• All reporting of coded data is impacted by
Physician documentation (documentation is not
just for ICD-10)
87
© 2014 Panacea Healthcare Solutions, Inc.
Working With Physicians
• Incomplete documentation means unspecified ICD10-CM diagnosis codes (potential non-payment
related to medical necessity)
• Potentially unable to code ICD-10-PCS procedure
codes
• Address quality scores with Physician and how
documentation impacts their scores (SOI and ROM)
– “what’s in it for them”
• Physician quality scores impact patient’s decisions
for where they chose to get their healthcare
88
© 2014 Panacea Healthcare Solutions, Inc.
CDI Program Tips
• Live communication vs. electronic queries – what do your
Physicians prefer? (Workstations on wheels)
• Friendly competition among Physicians is good, post I-10
clarification results
• Decide on what you are going to “query” for ICD-10 as
queries will increase (unspecified vs specified diagnosis
codes)
• Procedures will need to be added to the query process
• Communication of queries to HIM Coding staff will be
imperative so HIM does not repeat what has already been
done – a single universal query work list that is accessible by
CDI and HIM
89
© 2014 Panacea Healthcare Solutions, Inc.
CDI Program Tips
• Identify top I-10 queries and track by Physician – track
improvement and post results
– Type of clarification/query
– Physician
– Response type
– Financial impact
• If a Physician does not respond to a query after two attempts
– contact your Physician Advisor
• Report at Medical Staff meetings
• Formal bi-weekly calls with Physician Advisor
90
© 2014 Panacea Healthcare Solutions, Inc.
CDI Program Tips
• Clinical Documentation Improvement Program
– Staffing and productivity
• One CDS for every 1,900 annual discharges
– Historically just DRG-based payers, moving to all
patients
– Work flow / responsibilities
– Tools / reporting
– Assess query rates as they will increase (procedure
queries now)
– Physician involvement
91
© 2014 Panacea Healthcare Solutions, Inc.
In Summary……….
• Work with Physicians on “Documentation” in
general…….QUALITY
• Address EHR templates that can assist
Physicians
• Physician documentation tools
• Physician Advisor
• CDI Role
• What Will You Query For?
• CDI Reporting
92
© 2014 Panacea Healthcare Solutions, Inc.
Thank You and Questions
?????
© 2014 Panacea Healthcare Solutions, Inc.
93