ICF-CY
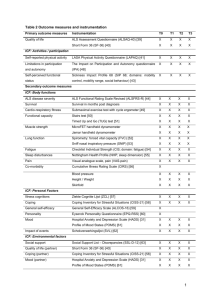
advertisement

Classifying childhood disability with the ICF-CY: from function to context Rune J. Simeonsson, Ph.D.,MSPH University of North Carolina, Chapel Hill Don J. Lollar, Ed.D. U.S. Centers for Disease Control and Prevention Priority of documenting childhood disability: 1915 • “ during the third or fourth month, the most important acquisition being the power of balancing the head on the shoulders; the absence of this power at this stage was one of the earliest signs of mental deficiency” (Forsyth, 1915, British Medical Journal, p. 535) Overview • Present overview of ICF version for children and youth (ICF-CY) • Identify different uses of the ICF-CY • Review guidelines for coding • Illustrate coding applications for different uses Clinical Educational Data management Statistical/ Research • Identify continuing issues in the implementation of the ICF-CY ICF-encompassing adult functioning Body Functions & Structures Activities & Participation Environmental Factors Functions Capacity Barriers Structures Performance Facilitators Need for ICF-CY Functioning, Activities, Participation & Environments different from those of adults Why is there a need for an ICF for children & youth? • Nature and form of functioning in children different from that of adults • Main volume of ICF lacking precursors of adult characteristics • Child as a “moving target” in classification of function • Indicators of functional risk factors crucial for prevention and early intervention • ICF version for children and youth provides continuity of documentation in transitions from child to adult services Chronology • 1996-2001- Children’s task force on development of ICF • 2001- Development of ICF-CY commissioned (WHOFIC, Washington, DC) • 2002-2005- Convening of WHO work group in various venues (Africa, Europe, North America, Asia) • 2003- First draft of ICF-CY delivered to WHO • 2004-2005- Collection of field trial data • 2005- Revision of ICF-CY Chronology • 2005- Meeting with WHO to finalize ICF-CY • 2005- Preparation and submission of evidence document to WHO • 2005-Submission of 2nd draft to WHO • 2005- Review of 2nd draft by experts & original writers • 2006-Final revisions/ ICFCY photo contest • 2006- Anticipated publication Guidelines for development of the ICF-CY • Development of ICF-CY guided by relevant research and theory • Structure ICF main volume maintained • Inclusion/exclusion criteria expanded • New content added to unused codes at 4, 5 and 6 character level • Formats to highlight applications relevant to children Central concepts from theory and research guiding ICF-CY development • Development and Disablement as parallel processes- • Changes in functions, activities and participation of child reflecting: Role of environment (transactional model) Child in context (Ecological systems theory) Development (Similar sequence/similar structure) Behavioral Regulation & organization Mediating role of Temperament/behavioral style Timing and maturation (Developmental delay) Development of the ICF-CY Expansions- New codes- 4 New codes- 5 New codes- 6 New codesTotal I, E BF 14 4 13 2 33 BS 0 1 2 4 7 A&P EF 66 21 77 4 168 19 2 8 0 29 Total 99 28 100 10 237 ICF-CY: New BF codes • Manual dominance b1473 • Lateral dominance b1474 • Reception of gestural language b16703 • Expression of gestural language b16713 • Growth maintenance function b560 • Onset of menstruation b6503 • Acquiring learning Acquiring information Acquiring language b132 b133 ICF-CY: representative new content (e.g. A/P codes) • • • • • • • • Learning through actions and playing d131 Acquiring language d133 Acquiring concepts d134 Following routines d2300 Adapting to changes in daily routine d2304 Adapting to changes in time demands d2305 Managing one’s time d2306 Managing one’s own behavior d235 • • • • Caring for the nose d5205 Indicating need for urination d53000 Indicating need for defecation d53010 Indicating need for eating d5500 • ICF-CY: environmental factors codes • Drink e1102 • Products and technology for play e1271 • Products and technology for personal indoor and outdoor mobility transportation e120 • Products and technology for communication • Special education & training e125 e586 General coding rules: annex 2 ICF A. Select an array of codes to form an individual’s profile B. Code relevant information- always in the context of a known or presumed health condition C. Code explicit information- the basis for coding must be explicit information D.Code specific information- code at the most specific level possible (1, 3, 4 or 5 character levels) Criteria for qualifiers Form of Qualifier ICF Manual (problem= ICF-CY (std dev value< mean Rating/ 0-none ( 0-4%) 0-none (5-24%) 1-mild scale of difficulty in %) Descript./ 1-mild and/or % of population with problem) <-1.0 sd (68%) -1. -1.5sd (22%) Stand.dev 2-moderate (25-49%) 2-moderate1.5-2.5 sd (6%) % of difficulty 3-severe % of population (50-95%) 3-severe 2.5-3.0 sd (3.0%) 4-complete (96-100%) 4-complete 3+sd (1.0%) Ethical guidelines in use of ICF: annex 6 • Respect and confidentiality Respect inherent value and autonomy of individual Never use to label individuals Use with full knowledge, cooperation and consent of person or advocate ICF codes treated confidentially • Clinical use of the ICF Explain purpose to individual or advocate Opportunity for individual or advocate to participate ICF used holistically (limitation in physical/social context) • Social uses of ICF information Used in collaboration with individuals or advocates ICF information use toward social policy- change ICF not used to deny rights Recognize individual differences Classification applications of ICF-CY • A common, universal language shared across disciplines and service settings • A taxonomy for documentation of child functioning in: assessment intervention outcome measurement • A framework for specifying the Child, the Environment and the Interaction in child- environment interaction ICF-CY: documenting Child-Environment Interaction Child Physical and Mental function & structure Environment Availability & accessibility of physical, social, & psychological elements ICF-CY: documenting Child-Environment Interaction <--Interaction Child Body Function and Body Structure (intact- impaired) Participation (Full to restricted) Activity (Complete to limited ) Environmental Factors (Barriers Facilitators) Classification applications of ICF-CY • Standard for documentation of child rights-UN Convention on the Rights of the Child • Framework for integrating interdisciplinary work • Profiling functions for planning individualized interventions • Documenting clinical features of childhood health conditions & diagnoses • Resource in data management • Intervention and outcome markers in education • Variables for statistical and research work ICF: Framework for interdisciplinary work Health Condition (disorder/disease) Body Structures & Functions Participation (participation restriction) Activities (activity limitation) Environmental Factors Personal Factors ICF-CY: General steps in coding • 1. Define the information available for coding and identify whether it relates to the domain of Body Functions, Body Structures, Activities/Participation or Environmental Factors. • 2. Locate the chapter (4-character code) within the appropriate domain most closely corresponding to the information to be coded. • 3. Read the description of the 4-character code and attend to any notes related to the description. • 4. Review any inclusion or exclusion notes that apply to the code and proceed accordingly. ICF-CY: General steps in coding • 5. Determine if the information to be coded is consistent with the 4-character level or if a more detailed description at the 5- or 6-character code should be examined. • 6. Proceed to the level of code that most closely corresponds to the information to be coded. Review the description and any inclusion or exclusion notes that apply to the code. • 7. Select the code and review available information for assigning a value for the universal qualifier that defines the extent of the impairment, functional limitation, participation restriction (0=no impairment/difficulty to 4= complete impairment/difficulty or environmental barrier (0=no barrier to 4=complete barrier) or facilitator (0=no facilitator to+ 4=complete facilitator) ICF-CY: General steps in coding • 8. Assign the code with the qualifier at the 2nd -, 3rd - or 4th-item level. For example, d115.2 (moderate difficulty in listening). • 9. Repeat steps 1-8 for each manifestation of function or disability of interest for coding and where information is available • 10. Parents and consumers may participate in the process by completing age-appropriate inventories that allow specific areas of functional concern to be highlighted, but before full evaluations and codes are provided by professionals or a team of professionals. Case: 10 year old boy • T is a ten-year-old boy who was referred to a clinic for an evaluation after experiencing pervasive academic difficulties in the previous two years of school. On the basis of observation, it is clear that he has significant problems in concentration on academic tasks and is highly distractible. His parents report that T is “on the go” all the time and doesn’t seem to listen. According to his parents and teachers he has difficulty keeping still for any length of time in tasks at home and at school. At the present time, this means that he has trouble completing assigned work in the classroom. Case: 10 year old boy He has particular difficulties remembering material he has studied. He is currently failing all of his academic classes and his performance in reading and writing is at the second grade level. He also shows difficulties adjusting to social situations involving other children. At school as well as at home, T’s teacher and parents are concerned about his high level of activity and the fact that he doesn’t seem to be able to think before he acts. This is evident in his social behavior when he fails to wait for his turn in games and sports and at home when he rides his bicycle into a busy street without looking. Case: 10 year old boy • A number of different interventions have been tried to help T perform in the classroom, but these have not resulted in improved performance. While the family has been reluctant to consider medication, T was recently seen by his pediatrician and Ritalin has been prescribed for his high level of activity. In conjunction with the medication trial, the school is designing an education support plan. Case: 14 year old • J is a 14 year-old girl living with her parents in a small town. She has severe asthma which was detected at a very young age. In addition to heightened response to specific allergens, J’s asthmatic attacks are also triggered by exercise, cold air and when she feels anxious. These attacks last 1-2 hours and occur several times a week. She is currently prescribed a bronchodilator and is to use a nebulizer prophylactically. In the last year, however, J is often inconsistent in following the medication regimen with the result that acute episodes are occurring more frequently. Case: 14 year old • From the time she was enrolled in a preschool program to the present, J’s school attendance has been marked by frequent absences. The result has been that her achievement has been consistently poor, and while she has not failed any grades she is falling farther and farther behind her peers. At the present time, she is in the eighth grade in the local middle school. Because of frequent absences, J has not developed a consistent group of friends at school. Case: 14 year old • Further, because exercise triggers acute episodes, she has not participated in the physical education program at school and is not engaged in any other regular physical activity. A result is that she has experienced a significant weight gain in the last year. J reports feeling different from others increasingly isolated from her peers. Her parents are becoming very concerned about her physical and emotional health and are seeking consultation from their medical doctor. ICF-Cy application: profile dimensions of childhood disability • 10-year old Child • 14 year old Child Clinical applications: clarification of assessment and diagnosis • Differentiate characteristics within a diagnosis- • Differentiate characteristics of children with the same or different diagnosis- • Address disconnect between diagnostic information and the nature of intervention • Selection of relevant variables for documentation of child outcomes Clinical application: possible features characterizing child • Child with: • impairment in social function d710.3 basic interpersonal interactions D750.2 informal social relationships D760.3family relationships • impairment in communication d310.2 communicating with – receiving spoken messages d315.4 communicating with – receiving nonverbal messages d330.4 speaking d335.3 producing nonverbal messages • restricted, repetitive stereotypic behavior pattern b7653 Stereotypies and mannerisms Clinical application; clarifying DSM-IV-TR diagnosis • 299.0 Criteria for Autistic disorder • A. Total of 6 items from three domains impairment in social function (2+ items) impairment in communication (1+) restricted, repetitive stereotypic behavior pattern (1+) • B. Delayed/abnormal functioning <3 yrs in one of three areas: social interaction, language, symbolic play • C. Rule out Rett syndrome or Childhood Disintegrative Disorder. Clinical application: possible features characterizing child • Child with problems of attention B1400.3 sustaining attention B1402.4 dividing attention D110.3 watching D115.3 listening D160.4 focusing attention • problems of undertaking and completing task B1641.3 organization and planning B1646.3 problem solving D2100.3 undertaking a single task d2102.4 undertaking a single task independently d2201.3 completing multiple tasks Clinical application: possible features characterizing child • Child with problems of regulating activity & behavior B1304.3 impulse control B127.4 regulation of behavior B1470.3 psychomotor control D2301.3 managing daily routine D2303.4 managing one’s own activity level D4153.3 maintaining a sitting position D7202.2 regulating behaviors within interactions D7204.3 maintaining social space D820.4 school education Clinical application: clarifying DSM-IVTR diagnosis Criteria for ADHD- Inattention : Six or more of the following- manifested often • Inattention to details • Difficulty sustaining attention • Seems not to listen • Fails to finish tasks • Difficulty organizing • Avoids tasks requiring sustained attention • Loses things • Easily distracted • Forgetful Clinical application: clarifying DSM-IV TR diagnosis Criteria for ADHD Impulsivity/Hyperactivity : Six or more of the following- manifested often • Impulsivity • Hyperactivity • Difficulty awaiting turn • Inappropriate running/ climbing • Blurts out answer before • Fidgets • Unable to stay seated question is finished (restlessness) • Interrupts or intrudes upon • Difficulty engaging in leisure others activities quietly • On the go • Talks excessively Educational application: manual for special education *Manual for use of ICF for children and youth with disabilities *Edited and written by National Institute of Special Education Japan, Approved by WHO Educational application: framing intervention outcomes Activities •Improvement in school functioning; •d166 reading •d170 writing •d172 calculating •d160 focusing attention •d175 solving problems •d310 communicating •d330 speaking Participation •Improvement in personal functioning; & social relationships -D880 play -D350 conversation -D710 interpersonal relationships -D7504 relating with peers -D7604 family relationships Educational applications: documenting progress of functional outcomes • Gradient of change: reduction of severity level within code (e.g. regulating behaviors within interaction) • d7202.4 --> d7202.2 • ( complete-> moderate level) • Hierarchy of change: moving from lower level code to higher level code • (undertaking simple task) d2100.2 • • (undertaking complex task) d2101.2 Data management application • Use of the ICF and sample d-Codes to describe health-related data elements are recommended in the U.S. Department of Education’s Early Intervention Data Handbook (Version 1.0). • http://www.ideadata.org/ • EarlyInterventionDataHandbook.asp EI DATA HANDBOOK • PURPOSE: to provide guidance for record information systems and collection of data on early intervention services • A reference book- to promote common language- does not constitute federal requirement • USE: gathering information about infants and toddlers with disabilities for service decisions, program management, research, policy analysis and program evaluation SAMPLE ICF d-CODES IN EI DATA HANDBOOK d160 d1750 d329 d330 d349 d4103 d4104 d435 d440 d445 d450 d4550 d465 d530 Focusing attention Solving simple problems Communicating-Receiving Information Speaking Communication Sitting Standing Moving objects with lower extremities Fine hand use Hand and arm use Walking Crawling Moving around using equipment Toileting Assessment inventory in Early intervention • Early intervention program for children birth to 3 in Georgia • Adaptation of 0-3 questionnaire developed for field trials of ICF-CY • Selected codes from Activities/Participation and Environmental Factors • Very favorable response by parents to format and developmental content • Resulted in raised awareness of environmental factors not considered previously Statistical & research applications • Established inter-rater reliability in assigning ICF codes: children with disabilities using existing developmental measures (Ogonowski, et al., 2004); and children with special health care needs structured interview (Kronk, et al., 2005) • ICF framework for setting goals for children with speech impairments (McLeod & Bleile, 2004). Statistical & research applications: Canadian national survey data • Measuring chronic health conditions and disability in children in Canadian national survey data (McDougall & Miller, 2003). • Review of 4 disability and 5 health surveys for extent of coverage of health conditions (ICD-10) and disability (impairment, activity and participation restrictions- ICF) • Two independent reviewers Statistical & research applications: Canadian national survey data Extent of coverage of domain Disability Surveys Health Surveys Health conditions 67% 39% Impairments 50% 55% Activities/ Participation 64% 84% Environmental Factors 60% 68% Statistical & research applications: Canadian national survey data • Participation and Activity Limitation Survey and National Longitudinal Survey for Children and Youth provided best coverage of ICF activity limitations • PALS provided most comprehensive coverage of need for/use of Assistive technology • Areas of limited coverage in surveys: Mental functions and some body functions; Personal care and domestic life; natural environment changes, attitudes and policies. Research application: joint use of ICF and ICD-10 to code reasons for eligibility in early intervention • What is the nature and prevalence of functional characteristics of young children (< 3 years) in early intervention ? • Lack of information due to the fact that existing eligibility data assigned children to 3 general categories (developmental delay, established medical conditions, risk status) • Data drawn from National Early Intervention Longitudinal Study (NEILS) a weighted sample of children and families from the time they enter early intervention through at least kindergarten. NEILS Enrollment Sample • Information collected on 5,668 children • Descriptors accompanying the child’s eligibility status were coded • 445 different classification entries were organized under 4 categories and 29 subcategories • An average of 1.5 descriptors provided for each child (range 1 -11) Algorithm for NEILS coding system Classification A conceptual framework with 4 major categories (I-IV) and 29 sub-categories (A-BB): I. Impairment of body functions or structure (A-H) II. Limitations of activity or performance (I-P) III. Diagnosed health conditions (Q-X) IV. Environmental factors (Y-BB) Method: Descriptors on enrollment forms were coded to the closest ICD-10 or ICF codes ICF: Framework for NEILS coding system CATEGORY III: Health Condition (disorder/diseaseICD dx) CATEGORY I: Body Structures & Functions CATEGORY II: Activities (activity limitation) CATEGORY IV: Environmental Factors CATEGORY II: Participation (participation restriction) Personal Factors Distribution of descriptors (%) assigned to ICD-10 and ICF codes CATEGORY Coded to ICD Coded to ICF Total= 385 Total=58 I. Body function -structure 23.0% 5.9% II. Activity 0.4% 2.0% III. Health 56.6% 3.2% IV. 6.3% 2.0% limitations conditions Environment Distribution of ICD codes (N=385) in NEILS coding system • Chapter % • Infection 1.62 • Neoplasms 1.08 • Metabolic 10.54 • % • Genitourinary 0.08 • Congenital 45.68 • Injuries 1.62 15.13 • Social risk 2.16 • Circulatory 6.49 • V-codes 5.95 • Digestive 5.14 • Nervous system Distribution of ICF (N=58) codes in NEILS coding system • Domain % • Body/mental function 37.3 • Body structures 27.1 • Activities/Participation 22.0 • Environmental factors 13.6 Distribution of descriptors (%) assigned to codes by category* (>100% given multiple descriptors/child) CATEGORY Percent of sample I. Body function -structure 71.8% II. Activity 9.5% III. Health 37.0% IV. 4.8% limitations conditions Environment ICF-CY: further work • Mapping of existing instruments to ICF-CY domains and codes • Development of ICF-CY based screening instruments • Development of assessment measures compatible with ICF-CY • Introduction of ICF-CY codes into surveys • Introduction of ICF-CY codes into information systems • Education and training of field Revisiting a priority • “..classification is serious business. Classification can profoundly affect what happens to a child. It can open doors to services and experiences the child needs to grow in competence, to become a person sure of his worth, and appreciate the worth of others, to live with zest and to know joy”. • (Classification of Children, Hobbs, 1975; The futures of children, Hobbs, 1975)