L7_Nutrition
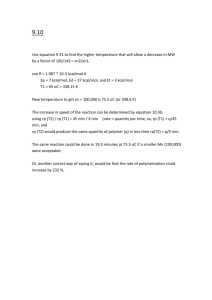
advertisement

Nutrition Support Ahmed Mayet, Pharm.D Associate Professor King Saud University Questions What medical history support that the patient is “at risk” of malnutrition? What physical findings support that the patient is “at risk” of malnutrition? Nutrition Nutrition—provides with all basic nutrients and energy required for maintaining or restoring all vital body functions from carbohydrate and fat and for building up body mass from amino acid. Malnutrition Malnutrition—extended inadequate intake of nutrient or severe illness burden on the body composition and function—affect all systems of the body. Types of malnutrition Kwashiorkor: (kwa-shior-kor) is protein malnutrition Marasmus: (ma-ras-mus) is proteincalorie malnutrition Kwashiorkor Protein malnutrition - caused by inadequate protein intake in the presence of fair to good calories intake in combination with the stress response Common causes - chronic diarrhea, chronic kidney disease, infection, trauma , burns, hemorrhage, liver cirrhosis and critical illness Clinical Manifestations Marked hypoalbuminemia Anemia Edema Muscle atrophy Delayed wound healing Impaired immune function Marasmus The patient with severe protein-calorie malnutrition characterized by calories deficiency Common severe burns, injuries, systemic infections, cancer etc or conditions where patient does not eat like anorexia nervosa and starvation Marasmus The patient with severe protein-calorie malnutrition characterized by calories deficiency Common severe burns, injuries, systemic infections, cancer etc or conditions where patient does not eat like anorexia nervosa and starvation Clinical Manifestations Weight loss Reduced basal metabolism Depletion skeletal muscle and adipose (fat) stores Decrease tissue turgor Bradycardia Hypothermia Risk factors for malnutrition Medical causes Psychological and social causes Medical causes (Risk factors for malnutrition) Recent surgery or trauma Sepsis Chronic illness Gastrointestinal disorders Anorexia, other eating disorders Dysphagia Recurrent nausea, vomiting, or diarrhea Pancreatitis Inflammatory bowel disease Gastrointestinal fistulas Psychosocial causes Alcoholism, drug addiction Poverty, isolation Disability Anorexia nervosa Fashion or limited diet Consequences of Malnutrition Malnutrition places patients at a greatly increased risk for morbidity and mortality Longer recovery period from illnesses Impaired host defenses Impaired wound healing Impaired GI tract function Cont: Muscle atrophy Impaired cardiac function Impaired respiratory function Reduced renal function mental dysfunction Delayed bone callus formation Atrophic skin International, multicentre study to implement nutritional risk screening and evaluate clinical outcome “Not at risk” = good nutrition status “At risk” = poor nutrition status Results: Of the 5051 study patients, 32.6% were defined as ‘atrisk’ At-risk’ patients had more complications, higher mortality and longer lengths of stay than ‘not at-risk’ patients. Sorensen J et al ClinicalNutrition(2008)27,340 349 International,multicentre study to implement nutritional risk screening and evaluate clinical outcome ClinicalNutrition(2008)27,340e349 Resting metabolism (% of normal) Metabolic Rate Major burn Sepsis Trauma Partial starvation Total starvation 180 160 140 120 100 Normal range 80 60 0 10 20 30 Days 40 50 Long CL, et al. JPEN 1979;3:452-6 Protein Catabolism Major burn Trauma Sepsis Partial starvation Total starvation Nitrogen excretion 30 25 20 15 10 Normal range 5 0 0 10 20 30 40 Days Long CL. Contemp Surg 1980;16:29-42 Answer (medical history) What medical history support that the patient is “at risk” of malnutrition? Nausea Abdominal pain Diarrhea Loss of appetite Weight loss Answer (physical finding) Cont; What physical findings support that the patient is “at risk” of malnutrition? Pale Lethargic Muscle wasting cachecxia Edematous Hypotensive Tachycardia Burses and patichiae on the limbs Question What biochemical, anthropometric, indirect calorimetric, and other testes are suggesting that your patient is malnourish? Cont: The initial assessment of nutritional status requires a careful History Physical examination Laboratory and other tests Laboratory and other tests Weight BMI Fat storage Somatic and visceral protein Standard monogram for Height and Weight in adult-male Height Small Frame Medium Frame Large Frame 4'10" 102-111 109-121 118-131 4'11" 103-113 111-123 120-134 5'0" 104-115 113-126 122-137 5'1" 106-118 115-129 125-140 5'2" 108-121 118-132 128-143 5'3" 111-124 121-135 131-147 5'4" 114-127 124-138 134-151 5'5" 117-130 127-141 137-155 5'6" 120-133 130-144 140-159 5'7" 123-136 133-147 143-163 5'8" 126-139 136-150 146-167 5'9" 129-142 139-153 149-170 5'10" 132-145 142-156 152-173 5'11" 135-148 145-159 155-176 6'0" 138-151 148-162 158-179 Percent weight loss 50kg x 2.2 = 110 lbs Small frame 129 lbs – 110 lbs = 19 lbs 19/129 x 100 = 15% Medium frame 139 lbs – 110 lbs = 29 lbs 29/139 x 100 = 20% Severe weight lost Time Significant Weight Loss (%) Severe Weight Loss (%) 1 week 1-2 >2 1 month 5 >5 3 months 7.5 >7.5 6 months 10 >10 Laboratory and other tests Weight BMI Fat storage Somatic and visceral protein Average Body Mass Index (BMI) for Adult Classification BMI (kg/m2) Underweight Normal Overweight Obesity <18.5 18.5-24.9 25.0-29.9 30.0-34.9 Moderate obesity Extreme obesity 35.0-39.9 >40.0 Our patient BMI = 16.3 kg/m2 Obesity Class I II III Laboratory and other tests Weight BMI Fat storage Somatic and visceral protein Fat Assessment of body fat – Triceps skinfold thickness (TSF) – Waist-hip circumference ratio – Waist circumference – Limb fat area – Compare the patient TSF to standard monogram Laboratory and other tests Weight BMI Fat storage Somatic and visceral protein Protein (Somatic Protein) Assessment of the fat-free muscle mass (Somatic Protein) Mid-upper-arm circumference (MAC) Mid-upper-arm muscle circumference Mid-upper-arm muscle area Compare the patient MAC to standard monogram Protein (visceral protein) Cont; Assessment of visceral protein depletion Serum albumin <3.5 g/dL Serum transferrin <200 mg/dL Serum cholesterol <160 mg/dL Serum prealbumin <15 mg/mL Creatinine Height Index (CHI) <75% Our patient has albumin of 2.2 g/dl Creatinine-height index (CHI ) [measured urinary creatinine (24hr)/ Ideal urinary creatinine for a given height] Ideal Cr = IBW x 23 mg/kg male = IBW x 18 mg/kg female CHI > 80 mild depletion CHI 60 – 80 moderate CHI < 60 severe Assuming that our patient IBW 59 kg (from chart) 990mg/ 59 kg x 23 = 73% (mild depletion) Vitamins deficiency Vitamin Vitamin Vitamin Vitamin Vitamin Bs (B1,B2, B6, B 9, B12, ) C A D K Trace Minerals deficiency Zinc Copper Chromium Manganese Selenium Iron - Clinical Sign or Symptom Nutrient General Wasted, thin Calorie - Loss of appetite Protein-calorie Skin Eczematous scaling Zinc - *Pallor Folate, iron, vitamin B12, copper Follicular hyperkeratosis Vitamin A Flaking dermatitis Protein-calorie, niacin, riboflavin, zinc *Bruising Vitamin C, vitamin K - Pigmentation changes Protein-calorie, niacin - Scrotal dermatosis Riboflavin *Our patient Neck Goiter Iodine - Parotid enlargement Protein Thorax Thoracic rosary Vitamin D Abdomen Diarrhea Niacin, folate, vitamin B12 - Distention Protein-calorie - Hepatomegaly Protein-calorie Extremities *Edema Protein, thiamine - Bone tenderness Vitamin D - Muscle wasting Protein, vitamin D, selenium Nails - *Hyporeflexia Ataxia *Spooning Transverse Thiamine Vitamin B12 Iron Protein Estimating Energy/Calorie BEE Basal Metabolic Rate (BMR) or Basal Energy Expenditure (BEE) accounts for the largest portion of total daily energy requirements Total Energy Expenditure TEE (kcal/day) = BEE x stress/activity factor BEE The Harris-Benedict equation is a mathematical formula used to calculate BEE Harris–Benedict Equations Energy calculation Male BEE = 66 + (13.7 x actual wt in kg) + (5x ht in cm) – (6.8 x age in y) Female BEE = 655 + (9.6 x actual wt in kg) + (1.7 x ht in cm) – (4.7 x age in y) A correlation factor that estimates the extent of hyper-metabolism 1.15 for bedridden patients 1.10 for patients on ventilator support 1.25 for normal patients The stress factors are: 1.3 for low stress 1.5 for moderate stress 2.0 for severe stress 1.9-2.1 for burn Calculation Our patient Wt = 50 kg, Age = 45 yrs Height = 5 feet 9 inches (175 cm) BEE = 66 + (13.7 x actual wt in kg) + (5x ht in cm) – (6.8 x age in y) =66 + (13.7 x 50 kg) + (5 x 175 cm) – (6.8 x 45) =66 + ( 685) + (875) – (306) = 1320 kcal TEE = 1320 x 1.25 (normal activity) = 1650 kcal Calorie sources Calories 60 to 80% of the caloric requirement should be provided as glucose, the remainder 20% to 40% as fat To include protein calories in the provision of energy is controversial Fluid Requirements Fluid The average adult requires approximately 35-45 ml/kg/d NRC* recommends 1 to 2 ml of water for each kcal of energy expenditure *NRC= National research council Fluid 1st 10 kilogram 2nd 10 kilogram Rest of the weight 100 cc/kg 50 cc/kg 20 to 30 cc/kg Example: Our patient 1st 10 kg x 100cc = 1000 cc 2nd 10 kg x 50cc = 500cc Rest 30 kg x 30cc = 900cc total = 2400 cc Fluid Fluid needs are altered by the patient's functional cardiac, hepatic, pulmonary, and renal status Fluid needs increase with fever, diarrhea, hemorrhage, surgical drains, and loss of skin integrity like burns, open wounds Protein Needs Protein The average adult requires about 1 to 1.2 gm/kg 0r average of 70-80 grams of protein per day Protein The initial protein goals are estimated according to the following general guidelines Protein Stress or activity level Initial protein requirement (g/kg/day) Baseline 1.4 g/kg/day Little stress 1.6 g/kg/day Mild stress 1.8 g/kg/day Moderate stress 2.0 g/kg/day Severe stress 2.2 g/kg/day Nitrogen Balance Calculation Nitrogen Balance (NB) Calculation NB is an important calculation for assessing nutritional response NB is used to evaluate the adequacy of protein intake as well as to estimate current protein requirements Calculations NB = N intake – N losses N intake = Protein intake (g/day) / 6.25gm N losses = UUN (g/day) + 4g* UUN is determined from a 24 hour urine collection *4g is a "fudge factor" to account for miscellaneous nitrogen losses Cont: Positive NB indicates an anabolic state, with a net gain in body protein Negative NB indicates a catabolic state, with a net loss of protein With adequate feeding NB 0 –5 g/day indicates moderate stress NB > –5 g/day indicates severe stress Routes of Nutrition Support The nutritional needs of patients are met through either parenteral or enteral delivery route Enteral Nutrition Enteral The gastrointestinal tract is always the preferred route of support (Physiologic) “If the gut works, use it” EN is safer, more cost effective, and more physiologic that PN Potential benefits of EN over PN Nutrients are metabolized and utilized more effectively via the enteral than parenteral route Gut and liver process EN before their release into systemic circulation Gut and liver help maintain the homeostasis of the AA pool and skeletal muscle tissue EN (Immunologic) Gut integrity is maintained by enteral feeding and prevent the bacterial translocation from the gut and minimize risk of gut related sepsis Safety Catheter sepsis Pneumothorax Catheter embolism Arterial laceration Cost (EN) Cost of EN formula is less than PN Less labor intensive Contraindications Gastrointestinal obstruction Severe acute pancreatitis High-output proximal fistulas Intractable nausea and vomiting or osmotic diarrhea Enteral nutrition (EN) Long-term nutrition: Gastrostomy Jejunostomy Short-term nutrition: Nasogastric feeding Nasoduodenal feeding Nasojejunal feeding Parenteral nutrition (PN) Peripheral Parenteral Nutrition (PPN) Total Parenteral Nutrition (TPN) Cautious use of PN: Azotemia Congestive heart failure Diabetes Mellitus Electrolyte disorders Pulmonary disease Intact food Predigested food TF = tube feeding Total Parentral Nutrition Purpose To maintain positive nitrogen balance through the intravenous administration of required nutrient such as glucose, IL, AA, electrolytes, vitamins, minerals and trace elements Patient Selection General Indications Requiring NPO > 5 - 7 days Unable to meet all daily requirements through oral or enteral feedings Severe gut dysfunction or inability to tolerate enteral feedings. Can not eat, will not eat, should not eat Special Indications (can not eat) Cont: When enteral feeding can’t be established After major surgery Pt with hyperemesis gravidarum Pt with small bowel obstruction Pt with enterocutaneous fistulas (high and low) Cont: Hyper-metabolic states: Burns, sepsis, trauma, long bone fractures Adjunct to chemotherapy Nutritional deprivation Multiple organ failure: Renal, hepatic, respiratory, cardiac failure Neuro-trauma Immaturity Calorie sources 60 to 80% of the caloric requirement should be provided as glucose, the remainder 20% to 40% as fat Calculation Our patient Wt = 50 kg, Age = 45 yrs Height = 5 feet 9 inches (175 cm) BEE = 66 + (13.7 x actual wt in kg) + (5x ht in cm) – (6.8 x age in y) =66 + (13.7 x 50 kg) + (5 x 175 cm) – (6.8 x 45) =66 + ( 685) + (875) – (306) = 1320 kcal TEE = 1320 x 1.25 (normal activity) = 1650 kcal total calculated calorie = 1650 kcal 80% from glucose 1650 x 80 =1320kcal 20% from fat (IL) 1650 x 20 = 330kcal Protein 1.2gm/kg/day 1.2 x 50 = 60 gm Protein requirement 150 kcal to 6.25 gm of protein 1650 kcal/150 x 6.25 gm = 68.8 or 70gm Glucose Cont; Maximum oxidized rate for glucose is 4 - 7mg/kg/min (adult) Exp: our patient is 50 kg 5mg x 50kg x 60min x 24 hr =360 gm 360gm x 3.4 kcal/gm = 1224 kcal Maximum cal from glucose = 1224kcal Fat emulsion Maximum recommended allowance 2.5 grams/kg/day Exp: 2.5 x 50 kg = 125 gm 125gm x 9 kcal/gm = 1125 kcal Calorie calculation Total calorie requirement = 1650 kcal calorie from glucose = 1224 kcal _______ form lipid 436 kcal Intralipid contraindications: Hyperlipdemia Acute pancreatitis Previous history of fat embolism Severe liver disease Allergies to egg, soybean oil or safflower oil Diabetic DM is not contraindication to TPN Use sliding-scale insulin to avoid hyperglycemia Administration Central PN (TPN) Central PN (TPN) is a concentrated formula and it can delivered large quantity of calories via subclavian or jugular vein only Continuous vs Cyclic Administration Continuous vs Cyclic administration It is given overnight and the patient is free during the day from the PN solution and associated administration paraphernalia (long-term care) Continuous administration is preferred in hospitalized patients as they often have fluid and electrolyte disturbances Monitoring Complications of TPN Complications Associated with PN Mechanical complication Septic complication Metabolic complication Mechanical Complication Improper placement of catheter may cause pneumothorax, vascular injury with hemothorax, brachial plexus injury or cardiac arrhythmia Venous thrombosis after central venous access Infectious Complications PN imposes a chronic breech in the body's barrier system The mortality rate from catheter sepsis as high as 15% Inserting the venous catheter Compounding the solution Care-giver hanging the bag Changing the site dressing Metabolic Complications Early complication -early in the process of feeding and may be anticipated Late complication - caused by not supplying an adequate amount of required nutrients or cause adverse effect by solution composition Iron Iron is not included in TPN solution and it can cause iron deficiency anemia Add 100mg of iron 3 x weekly to PN solution or give separately Vitamin K TPN solution does not contain vitamin K and it can predispose patient to deficiency Vitamin K 10 mg should be given weekly IV or IM if patient is on longterm TPN Thank you