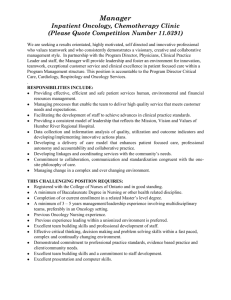
Reimbursement 2012
Bobbi Buell MBA
800-795-2633
Agenda
What’s Going On Right Now
Medicare PFS Final Rule 11-1-2011
PQRS and E-Prescribing 2012
Meaningful Use/ HIT
2012 Hospital Outpatient Prospective Payment
System Final Rule
New Payment Models
Coding 2012
Your To Do List
2
onPoint Oncology LLC
Disclaimer
Payers differ on their guidelines. Please verify coding for each payer and
claim.
All Medicare and RAC information is literally changing on a daily basis.
What is presented herein for 2012 is still being evaluated.
This is not legal or payment advice.
This content is abbreviated for Medical Oncology. It does not substitute
for a thorough review of code books, regulations, and Carrier guidance.
ICD-9-CM information is abbreviated and coders are urged to check the
tabular lists of code books for correct coding.
This information is good for the date of the information and may contain
typographical errors.
CPT is the trademark for the American Medical Association. All Rights
Reserved.
onPoint Oncology LLC
3
Medicare Physician Payment Basics
Payments are based on RVUs for each code
(WRVUs+PERVUs+MalRVUs)
RVUs are multiplied times GPCIs for your area. There is a work GPCI
floor in some areas of 1.00. (W*WGPCI+PE*PEGPCI+Mal*MalGPCI)
The Medicare conversion factor determines the overall level of Medicare
payments (W*WGPCI+PE*PEGPCI+Mal*MalGPCI) times CF = $Your
Total Allowable for your area
A formula spelled out in the Medicare statute determines the annual
update to the conversion factor and that has been a disaster.
onPoint Oncology LLC
4
SGR Update
SGR is frozen for two months. With no fix, a
5
27.4% decline.
GPCI floor is frozen for two months.
The fee schedule CF has been adjusted for
‘budget neutrality’. So, the new allowables have
nothing to do with the original one.
But, RVUs are the same.
Congress has looked at a longer fix, but expect a
fight. Probable case = 1-2 year fix.
onPoint Oncology LLC
A Little History…
Year
Medicare Acts
Conversion
1st Hour $
Drugs
Other
1991
Proposed MPFS
$30.00
$58.78
85% of AWP
Drugs now
paid at 2-3
times AWP
1993
Final MPFS
$31.00
N/A
100% of
AWP
99213 =
$31.00
1994
Cancer
Coverage
Improvement Act
$33.72 and
$32.90
N/A
100% of
AWP
Off-label use
approved;
oral cancer
drugs Part B
1996
HIPAA passed
$35.42 and
$34.63
N/A
100% of
AWP
False Claims
Act for
Medicare
1997
BBA of 1997
$36.69
N/A
95% of AWP
Oral antiemetics
passed
6
(c) onPoint Oncology LLC
A Little History
Year
Medicare Acts
Conversion
1st Hour
$
Drugs
Other
1998
None of Note
$36.69
N/A
95% of AWP or
inherent
reasonableness
LCA for
LUPRON
1999
None of Note
$34.73
N/A
95% of AWP
26 states
have off label
laws
2000
None of Note
$36.61
$61.90
95% of AWP
Drug pricing
investigated
2001
None of Note
$38.26
$62.00
95% of AWP
Aredia goes
generic
2002
Single Drug
Pricer
$36.20
N/A
95% of AWP
under SDP
Taxol goes
generic
7
(c) onPoint Oncology LLC
A Little History
Year
Medicare Acts
Conversion
1st Hour $
Drugs
Other
2003
Passed MMA
for 2004
$36.79
$59.22
95% of AWP
RACs
approved
2004
MMA
$37.34
$217.35
85% of AWP
for some
drugs
99211 denied
with drugs
2005
Demo Project $37.90
$177.61
ASP, plus 6% $130 per visit
for demo
2006
Demo Project $37.90
$172.81
ASP, plus 6%
$26 per visit
for demo
2007
PQRI
$37.90
$165.99
ASP, plus 6%
IVIG in
shortage
2008
ESAs limited
$38.09
$161.49
ASP, plus 6% 40% denial
rate on ESAs
beginning of
the year
8
(c) onPoint Oncology LLC
A Little History
Year
Medicare Acts
Conversion
1st Hour $
Drugs
2009
ARRA,
MIPPA
$36.07
$147.51 (32.1% since
2004)
ASP, plus 6%
2010
None of Note
Many
$140.72
ASP, plus 6%
PQRS/ ERx
= 4%
incentive
2011
None of Note
$33.98
$146.44
ASP, plus 6%
MUEs, Drug
Shortages
9
(c) onPoint Oncology LLC
Other
Medicare Physician Fee Schedule
PFS Final Rule 2012
11/1/2011
MPFS 2012
On November 1, 2011, the Centers for Medicare
& Medicaid Services (CMS) posted a proposed
notice for Medicare payments in the physician fee
schedule for calendar year (CY) 2012.
Here are the highlights of Rule which becomes
effective for dates of service on or after 1-1-2012.
https://www.cms.gov/PhysicianFeeSched/PFSFRN/list.asp#TopOfPage
11
onPoint Oncology LLC
Reductions Will Occur for Most Chemotherapy Administration
Codes (1 of 2)
Final 2011
CPT Code Descriptor
96401
96402
96405
96406
96409
96411
96413
96415
96416
Chemo antineopl sq/im
Chemo hormon
antineopl sq/im
Chemo
intralesional up
to 7
Chemo
intralesional
over 7
Chemo iv push
sngl drug
Chemo iv push
addl drug
Chemo iv
infusion 1 hr
Chemo iv
infusion addl hr
Chemo prolong
infuse w/pump
Final 2012
Total RVUs
MPFS
Payment
Total RVUs
MPFS
Payment*
Difference Difference
in RVUs in Payment*
2.14
$72.71
2.15
$53.04
0.47%
-27.05%
1.03
$35.00
0.99
$24.42
-3.88%
-30.21%
2.53
$85.96
2.49
$61.43
-1.58%
-28.54%
3.48
$118.24
3.55
$87.58
2.01%
-25.93%
3.32
$112.80
3.26
$80.43
-1.81%
-28.70%
1.86
$63.20
1.83
$45.15
-1.61%
-28.56%
4.31
$146.44
4.07
$100.41
-5.57%
-31.43%
0.92
$31.26
0.90
$22.20
-2.17%
-28.97%
4.75
$161.39
4.06
$100.17
-14.53%
-37.94%
Source: Centers for Medicare & Medicaid Services (CMS). Calendar Year 2012 Medicare Physician Fee Schedule Final Rule (CMS-1524-FC). Released November 1, 2011.
*These payment rates reflect the 27.4% across-the-board cut that will occur if Congress does not pass an SGR fix. Assuming Congress acts to avoid the SGR cuts, the changes in RVUs
are more reflective of the actual changes in payment rates for these codes in CY 2012.
Reductions Will Occur for Most Chemotherapy Administration
Codes (2 of 2)
Final 2011
CPT Code Descriptor
96417
96420
96422
96423
96425
96440
96446
96450
96542
Chemo iv infus
each addl seq
Chemo ia push
tecnique
Chemo ia
infusion up to 1
hr
Chemo ia
infuse each
addl hr
Chemotherapy
infusion
method
Chemotherapy
intracavitary
Chemotx admn
prtl cavity
Chemotherapy
into cns
Chemotherapy
injection
Total RVUs
MPFS
Payment
2.13
Final 2012
Total RVUs
MPFS
Payment
Difference
in RVUs
Difference
in Payment
$72.37
2.09
$51.56
-1.88%
-28.75%
3.21
$109.06
3.15
$77.71
-1.87%
-28.74%
5.16
$175.32
4.99
$119.58
-3.29%
-31.79%
2.35
$79.84
2.29
$54.88
-2.55%
-31.26%
5.29
$179.74
5.23
$125.33
-1.13%
-30.27%
21.45
$728.79
24.31
$599.76
13.33%
-17.71%
5.21
$177.02
5.58
$137.67
6.63%
-28.58%
5.85
$198.76
5.50
$135.69
-5.98%
-31.73%
3.74
$127.07
3.61
$89.06
-3.48%
-29.91%
Source: Centers for Medicare & Medicaid Services (CMS). Calendar Year 2012 Medicare Physician Fee Schedule Final Rule (CMS-1524-FC). Released November 1, 2011.
*These payment rates reflect the 27.4% across-the-board cut that will occur if Congress does not pass an SGR fix. Assuming Congress acts to avoid the SGR cuts, the changes in RVUs are
more reflective of the actual changes in payment rates for these codes in CY 2012
Multiple Procedure Payment Reduction (MPPR) Expansion
to Include Physician Interpretation
CMS finalized its proposal to expand the MPPR, which reduces payment
by 25 percent for each second and subsequent advanced imaging service
furnished during the same session to the “PC” of advanced imaging
services, which represents the physician interpretation of the image
Applies to CT, MR, and ultrasound
CMS currently applies the MPPR to the TC of the same services
CMS will consider the following MPPR policies in CY 2013 and beyond:
Apply the MPPR to the TC and PC of all imaging services (e.g., PET)
Apply the MPPR to the TC of all diagnostic tests
CPT
71250
72192
Total
Modifier Description
Global
TC
26
Global
TC
26
Ct thorax
w/o dye
Ct pelvis
w/o dye
CY 2012
Total
Physician
Transitional Malpractice
NF
Work
NF PE
RVUs
RVUs
RVUs
RVUs
6.92
1.02
5.84
0.06
5.45
0.00
5.44
0.01
1.47
1.02
0.40
0.05
6.69
1.09
5.54
0.06
5.14
0.00
5.13
0.01
1.55
1.09
0.41
0.05
CF1\
NF
Payment
$24.6712
$24.6712
$24.6712
$24.6712
$24.6712
$24.6712
$170.72
$134.46
$36.27
$165.05
$126.81
$38.24
$322.55
Current
payment
Methodology
Final
Payment
Methodology
1 x $134.46
1 x $36.27
1 x $134.46
1 x $36.27
0.5 x $126.81
1 x $38.24
$272.38
0.5 x $126.81
0.75 x $38.24
$262.82
Source: Centers for Medicare & Medicaid Services (CMS). Calendar Year 2012 Medicare Physician Fee Schedule Final Rule (CMS-1524-FC). Released November 1, 2011.
1CF = The final CY 2012 CF is $24.6712
PC = Professional Component
TC = Technical Component
MPFS 2012
Practice Expense: CMS continues for the third
year (at a 50/50 blend), the four-year phase-in of
the implementation of the American Medical
Association (AMA) Physician Practice Information
Survey (PPIS) data administered in 2007/08 for
practice expense (PE) indirect per hour rate.
Oncology is still using the AMA SMS data series.
Net year, this process of 5-year review will end
and CMS will focus on mis-valued codes. These
include 96413, 96367, and 96365.
https://www.cms.gov/PhysicianFeeSched/PFSFRN/list.asp#TopOfPage
15
onPoint Oncology LLC
MPFS 2012
Drugs
Average Manufacturers’ Price will be price substitution
for drugs where AMP is 5% or more below ASP for 2
consecutive quarters prior to the current quarter or for 3
out of the preceding 4 quarters.
This match-up will apply to BIOSIMILARS once they are
approved.
CMS emphasized that 103% of AMP will be the price
substitute if the threshold is exceeded per the
guidelines. Before implementation, 103% of AMP and
106% of ASP will be compared.
The spreadsheet used by Manufacturers will change in
2012.
https://www.cms.gov/PhysicianFeeSched/PFSFRN/list.asp#TopOfPage
16
onPoint Oncology LLC
MPFS 2012
The 72-Hour Rule (7/1/2012)
One of the most horrible parts of hospital
reimbursement is that all “related” services
within 72 hours before are bundled into the
hospital per discharge payment (MS-DRG).
CMS now proposes that, for any physician
practice that is totally owned by the
hospital or wholly-operated by the hospital,
their diagnostic procedures or related
therapeutic procedures will be impacted by
the 72 hour rule.
Professional components will be paid at the
facility (not non-facility) rate. –TC will be
denied.
All other codes will be paid at the facility rate.
Practices are responsible for billing with a –
PD Modifier, when the patient is admitted, but
this is not final until 7/1/2012. Hospitals must
notify the practice,
17
onPoint Oncology LLC
Medicare Physician Fee Schedule
PQRS and E-Prescribing
2012
PQRS 2012
The PQRS will pay bonuses equal to a 0.5%
bonus for reporting years in 2012 through 2014.
This is for all fee schedule services, excludes
drugs, labs, and DME.
In 2015, providers who don't participate in PQRS
will suffer a payment decrease. Beginning in
2015, EPs who do not satisfactorily report
Physician Quality Reporting System measures
will be subject to payment adjustments
2015: -1.5% payment adjustment
2016 and beyond: -2% payment adjustment
19
onPoint Oncology LLC
MPFS 2012
PQRS Changes (Proposed)
CMS is making an effort to consolidate PQRS reporting
with ARRA HIT incentives for Quality Indicator Reporting.
Time frame—a six month reporting period (7/1/201212/31/2012) will only be available for Measures Groups
through a Registry. All other reporting must be for the
full twelve-month period.
Consolidates current Group Practice options to one
Group Practice Reporting Option (GPRO) that is defined
as 25 or more eligible professionals.
18 measures may be reported under this option.
CMS will ‘suggest’ appropriate beneficiaries for reporting.
Practices must go through a self-nomination process.
20
onPoint Oncology LLC
PQRS Changes 2012
Measures
26 additional new measures, including 6 for cancer
44 CQM measures that are now reportable to get
the ARRA HIT incentive (“Meaningful Use”)
10 measures groups for reporting, none of which
are related to cancer
Reporting/HIT
EHR submission of PQRS data either through a
submission vendor or through a qualified EHR
system. These must be certified by PQRS..
Can report your CQMs for MU either by attestation
or by EHR through a portal or direct from your EHR.
21
onPoint Oncology LLC
New Cancer Measures 2012
New Individual Measures for 2012 PQRS
Measure
Developer
Consensus Status
Reporting Mechanism
CAP
N/A
Claims, Registry
Image Confirmation of
Successful Excision of
Image–Localized Breast
Lesion
ASBS
N/A
Claims, Registry
Preoperative Diagnosis of
Breast Cancer
ASBS
N/A
Claims, Registry
Sentinel Lymph Node Biopsy
for Invasive Breast Cancer
ASBS
N/A
Registry
AAD
N/A
Registry
Measure Title
Immunohistochemical (IHC)
Evaluation of HER2 for
Breast Cancer Patients
Biopsy Follow-up
Source: Centers for Medicare & Medicaid Services (CMS). Calendar Year 2012 Medicare Physician Fee Schedule Final Rule (CMS-1524-FC). Released November 1, 2011.
PQRS = Physician Quality Reporting System
CAP = College of American Pathologists
ASBS= American Society of Breast Surgeons
AAD= American Academy of Dermatology
Why Participate?
Performance will be the basis for payment in the
near future
Physician Compare beginning in 2013
http://www.medicare.gov/find-a-doctor/provider-
search.aspx
23
onPoint Oncology LLC
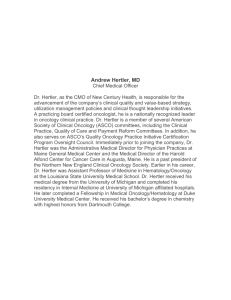
Physician Compare Website
“Physician Compare for 2011 includes information
about physicians and other professionals who
participated in the Physician Quality Reporting
System. It does not yet contain physician and
eligible professional performance information. We
expect to have performance information on
Physician Compare starting in 2013. This will be for
services those providers furnished to Medicare
beneficiaries during 2012.”
24
onPoint Oncology LLC
Physician Compare Website
25
onPoint Oncology LLC
PQRS Resources
See on CMS Web Site
Frequently Asked Questions
Supplemental education materials
National Provider Calls
Special Open Door Forums
QualityNet Help Desk
http://www.cms.hhs.gov/PQRI/36_HelpDeskSupport
.asp#TopOfPage
7:00 a.m. - 7:00 p.m. CST at 866-288-8912 or
qnetsupport@sdps.org
26
onPoint Oncology LLC
E-Prescribing – Penalties
2012 – 1% reduction
2013 – 1.5% reduction
2014 – 2% reduction
2011 Individual EPs must have :
report at least 10 electronic prescriptions to avoid penalty for
2012. Reporting period 1/1/11 – 6/30/11 (processed by 7/31);
report at least 25 electronic prescriptions to avoid penalty for
2013. Reporting period 1/1/11 – 12/31/11.
27
E-Prescribing 2012
Reporting Year
Report 10
Encounters
Report 25
Encounters
2011
No penalty in 2012
No penalty in 2013
2012
No penalty in 2013
No penalty in 2014
2013
No penalty in 2014
No penalty in 2015
https://www.cms.gov/PhysicianFeeSched/PFSFRN/list.asp#TopOfPage
28
onPoint Oncology LLC
E-Rx Reporting
For successful claims-based reporting in 2012, a
single code should be reported (numerator)
G8553 – At least one prescription created during the
encounter was generated and transmitted electronically
using a qualified e-Rx system
Must be on the same claim (denominator)–90801,
90802, 90804, 90805, 90806, 90807, 90808, 90809,
90862, 92002, 92004, 92012, 92014, 96150, 96151,
96152, 99201, 99202, 99203, 99204, 99205, 99211,
99212, 99213, 99214, 99215, 99304, 99305, 99306,
99307, 99308, 99309, 99310, 99315, 99316, 99324,
99325, 99326, 99327, 99328, 99334, 99335, 99336,
99337, 99341, 99342, 99343, 99344, 99345, 99347,
99348, 99349, 99350, G0101, G0108, G0109
29
onPoint Oncology LLC
eRx Incentive Payment
eRx incentive is percentage of all Medicare fee
schedule charges (not including drugs) based on EP’s
TIN/NPI.
2011, 2012 – 1%
2013 – 0.5%
EPs have until February 28, 2012 to submit CY 2011
claims to show they qualify.
30
eRx Incentive Payment
May report through:
Claims submissions.
Qualified Registry – (Some registries qualify for both PQRS
and eRx). Check CMS website for list of registries. Currently
2010 list available:
http://www.cms.gov/PQRI/Downloads/Qualified_Registries_Ph
ase4_eRxPQRI_06282010_FINAL.pdf
Qualified EHR – Check CMS website for list.
http://www.cms.gov/PQRI/Downloads/QualifiedEHRVendorsfor
the2011PhysicianQualityReportingandeRx121310.pdf
31
eRx – Penalties
Penalty Exceptions:
Individual EPs
EP who is not a physician, NP or PA as of June 30, 2012
EP who does not have 100 cases in applicable codes through 6/30/2012
Physician is unable to electronically prescribe due to local, state, or federal law
or regulation (e.g., state law prohibits e-Prescribing of controlled substances)
Hardship Exception:
Hardship Exception Codes: Use G8642 (practice in rural area without high speed
internet access) or G8643 (practice in area without available pharmacies for eprescribing).
Groups
Third and fourth exceptions above also apply to GPRO
Must go to the CMS web site to register exceptions by
6/30/2012
32
EHR and eRx: Integration & Penalties
If an EP gets an EHR incentive in 2011 and 2012, can
still get eRx 2012 penalty
E-prescribing measures are different
E-prescribing system requirements are different
If an EP gets an eRx incentive in 2011 and 2012, can
still get eRx penalty
Reporting periods for incentive and penalty are
different
For individual EPs (not groups) reporting
requirements are different.
33
E-Prescribing MPFS 2012
Changes include:
Use same coding requirements for the program in
2012.
Establish GPRO reporting requirements to be the
same as PQRS—25 or more eligible professionals.
Modifies the requirements of the program to allow
usage of either a qualified e-prescribing system or
using a certified EHR system to prescribe.
Reporting choices—only one per year-- include:
34
EHR (2 submissions per year)
Registry (2 submissions per year)
Claims
onPoint Oncology LLC
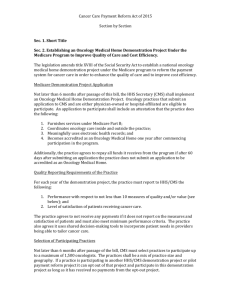
Medicare & Medicaid
EHR Incentive Programs
How Much Are the Incentives?
• Medicare Incentive Payments Detail
•
Columns = first calendar year EP receives a payment
• Rows = Amount of payment each year if continue to meet requirements
CY 2011
CY 2013
CY2014
CY 2015
and later
CY 2011
$18,000
CY 2012
$12,000
$18,000
CY 2013
$8,000
$12,000
$15,000
CY 2014
$4,000
$8,000
$12,000
$12,000
CY 2015
$2,000
$4,000
$8,000
$8,000
$0
$2,000
$4,000
$4,000
$0
$44,000
$39,000
$24,000
$0
CY 2016
TOTAL
36
CY 2012
$44,000
onPoint Oncology LLC
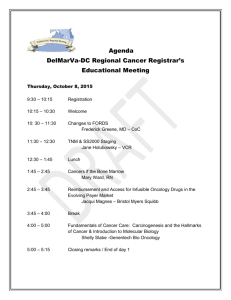
How Much Are the Incentives?
• Medicaid Incentive Payments Detail
•
•
Columns = first calendar year EP receives a payment
Rows = Amount of payment each year if continue to meet requirements
CY 2011
CY 2012
CY 2013
CY 2014
CY 2015
CY 2011
$21,250
CY 2012
$8,500
$21,250
CY 2013
$8,500
$8,500
$21,250
CY 2014
$8,500
$8,500
$8,500
$21,250
CY 2015
$8,500
$8,500
$8,500
$8,500
$21,250
CY 2016
$8,500
$8,500
$8,500
$8,500
$8,500
$21,250
$8,500
$8,500
$8,500
$8,500
$8,500
$8,500
$8,500
$8,500
$8,500
$8,500
$8,500
$8,500
$8,500
$8,500
CY 2017
CY 2018
CY 2019
CY 2020
CY 2021
TOTAL
37
CY 2016
$8,500
$63,750
onPoint Oncology LLC
$63,750
$63,750
$63,750
$63,750
$63,750
What is Meaningful Use?
• Meaningful Use is using certified EHR technology
to
• Improve quality, safety, efficiency and reduce health
•
•
•
•
disparities
Engage patients and families in their health care
Improve care coordination
Improve population and public health
All the while maintaining privacy and security
• Meaningful Use mandated in law to receive
incentives
38
onPoint Oncology LLC
A Conceptual Approach to Meaningful Use
Improved
outcomes
Advanced
clinical
processes
Data capture
and sharing
39
onPoint Oncology LLC
What You Need to Participate
• All providers must:
• Register via the EHR Incentive Program website---you need
to do this to be exempt from E-prescribing penalties, if the
EP did not report.
• Be enrolled in Medicare FFS, MA, or Medicaid (FFS or
managed care)
• Have a National Provider Identifier (NPI)
• Use certified EHR technology
http://healthit.hhs.gov/certification
• Medicaid providers may adopt, implement, or upgrade in their first
year
• All Medicare providers and Medicaid eligible hospitals
must be enrolled in PECOS, when this is required.
40
onPoint Oncology LLC
Websites
• Get information, tip sheets and more at CMS’ official
website for the EHR incentive programs:
http://www.cms.gov/EHRIncentivePrograms
• Eligibility
• Meaningful Use
• Medicaid State Information
• Educational Materials
• National CMS Listserv:
http://www.cms.gov/EHRIncentivePrograms/65_CMS_EHR_Listserv.
asp
• Frequently Asked Questions:
http://www.cms.gov/EHRIncentivePrograms/95_FAQ.asp
• Registration for the EHR Incentive Programs:
http://www.cms.gov/EHRIncentivePrograms/20_RegistrationandAttes
tation.asp
41
onPoint Oncology LLC
Educational Materials
www.cms.gov/EHRIncentivePrograms/55_EducationalMaterials.asp
Resources Available: Meaningful Use Calculator, Incentive Program Timelines,
Webinars, Eligibility Flow Chart and Interactive Tool, CMS ListServe, and more
42
onPoint Oncology LLC
Fee Schedule Changes to MU Incentive
For 2012
Reporting of Clinical Quality Measures (CQMs):
Attestation as it is today
Overlap PQRS with HIT Incentives
o Can delay your HIT incentive
o You may submit two ways:
• Through a portal
• Directly from an approved (by PQRS) EHR
43
onPoint Oncology LLC
2012 Medicare Hospital Outpatient
Prospective Payment System (OPPS):
Final Rule
Increase in Threshold to Determine Whether Drugs
are Paid Separately
Medicare uses two methods to pay for drugs and biologicals in the
hospital outpatient setting:
Bundled: Payment for products with a per dose cost under a specified
threshold are included in payment for administration or associated services
Separately Paid: Payment for products with a per dose cost above the
specified threshold are paid separately
CMS increased the packaging threshold for CY 2012 from $70 to $75
Products with estimated per day costs at or below the threshold are
bundled, while those with estimated costs above the threshold are
separately paid
This is less than the $80 threshold CMS proposed
The packaging threshold for CY 2012 is $75 per day
(an increase of $5 per day from the CY 2011 threshold)
Source: Source: Centers for Medicare & Medicaid Services (CMS). Calendar Year 2012 Outpatient Prospective Payment System Final Rule (CMS1525 FC). Released November 1, 2011.
Payment for Most Drugs and Biologics at ASP + 4, a
Decrease from ASP + 5
For CY 2012, CMS will reimburse drugs and biologics
as follows:
• Drugs and biologics eligible for pass-through*
payment: ASP + 6 percent
• Non-pass-through specified covered outpatient
drugs (SCOD): ASP + 4 percent
* Pass-through status is assigned to new products with costs that are “not insignificant” and stays in
effect for at least 2 years but no more than 3 years
Source: Source: Centers for Medicare & Medicaid Services (CMS). Calendar Year 2012 Outpatient Prospective Payment System Final Rule (CMS-1525 FC). Released November 1, 2011.
ASP = Average Sales Price
Payment Increase for Qualifying Cancer
Hospitals
Cancer hospitals receive:
The full difference for covered outpatient services under the OPPS
and the pre-BBA amount – in other words, they are “held harmless”
A transitional outpatient payment (TOP) to ensure that their payment
under the OPPS is not less than it was prior to BBA implementation
Per ACA, CMS will increase in payments to the 11 qualifying
cancer hospitals in CY2012
CMS will examine each cancer hospital’s data at cost report
settlement to determine its payment-to-cost ratio (PCR) and, if it is
below the weighted average PCR for other OPPS hospitals (target
PCR; 0.91 for CY 2012), it will receive a payment adjustment to
make the hospital’s PCR equal the target PCR
Most cancer hospitals will no longer qualify for Transitional
Outpatient Payments (TOPs) as a result of the increased payments
received under the proposed cancer hospital payment adjustment
CMS estimates an overall 9.5 percent increase in payments for
these hospitals as a result of these changes
Source: Source: Centers for Medicare & Medicaid Services (CMS). Calendar Year 2012 Outpatient Prospective Payment System Final Rule (CMS-1525 FC). Released November 1, 2011.
ACA = Affordable Care Act
Key Highlights of CY 2012 Quality Measures
CMS did not add any new measures to the Hospital Outpatient Quality Data Reporting Program (HOP
QDRP) program for CY 2012
Providers that do not satisfactorily report quality data during CY 2012 will continue to incur a two percent reduction in
their annual payment update for CY 2013:
Reduced
conversion factor
$68.62
Full, proposed
conversion
factor $70.02
The agency will continue its established process of adding measures to the HOP QDRP program for
three years of payment determinations, rather than one
In 2013, CMS will retain the 15 existing HOP QDRP measures from CY 2012
In 2014 ,CMS will retain all measures from CY 2013 and finalized three of the nine proposed
measures for CY 2014
Additional oncology-specific measures are being considered for 2015 and subsequent years:
Cancer Care (hormonal therapy, biopsies)
Chemotherapy
Colonoscopy and endoscopy
Source: Source: Centers for Medicare & Medicaid Services (CMS). Calendar Year 2012 Outpatient Prospective Payment System Final Rule (CMS-1525 FC). Released November 1, 2011.
New Payment Models
49
onPoint Oncology LLC
A Number of Factors Have Led to a Need for
Payment Reform
Misaligned Payment: Based on Volume
Lack of Information: Few Incentives for Care
Coordination
Variable Treatment: Patients Receive Suboptimal Care
Rising Costs: Increased Burden on
Purchasers
Current Efforts to Improve Quality and Reduce Costs
Focus Primarily on Enhancing the FFS Model
Current Efforts
Future Efforts
Pay-for-Reporting and
Pay-for-Performance
Payment Reform
Incentives, in addition to feefor-service payments, for
reporting performance
measures or achieving
specified quality standards
Introduction of new
payment models, including
bundled and global
payments
CMS physician and hospital quality pay-forreporting programs
Private payer pay-for-reporting programs
(e.g., Aetna, BlueCross BlueShield, United)
CMS = Centers for Medicare and Medicaid Services
FFS = Fee-for-service
Payment Reform Is Unlikely to Be a “One-SizeFits-All” Approach: Market Variables
Payment reform paradigms need to be
developed, tested, and analyzed on a
case-by-case basis, as their effects can
vary significantly across provider
organizations, conditions, and settings
Several variables must be
considered when instituting a new
payment policy:
Settings of care (full vs. partial
bundle)
Delivery system infrastructure
Market (e.g., numerous integrated
delivery systems)
Provider organization type
Existing payment infrastructure
Disease condition (chronic vs.
acute)
Associated area of medicine
Different Payment Systems Are
Appropriate for Certain Conditions and
Address Unique Cost and Quality Issues
High
Acute Episode
Payment
Amount of
Variation
in Cost
Per
Episode
Examples:
Hip Fractures,
Labor & Delivery
Year-Long Episode
Payment
+
Acute Episode
Payment
Examples:
Heart Disease,
Back Pain
Fee for Service
Year-Long Episode
Payment
Examples:
Immunizations,
Simple Injuries
Examples:
COPD, CHF
Low
Low
Variation in Frequency of
Episodes Per Condition
COPD = Chronic Obstructive Pulmonary Disease
CHF = Congestive heart failure
Source: Center for Healthcare Quality and Payment Reform. “Which Healthcare Payment System is Best?”. Available at
http://www.chqpr.org/downloads/WhichPaymentSystemisBest.pdf /
High
As an Alternative to Fee-for-Service, Payers
Use a Variety of Payment Reform Approaches
Bundled
Episode
Global
Scope of
payment
Payment for a tightlylinked set of services
provided by one or a
small number of providers
(e.g., Medicare’s hospital
inpatient DRG system)
Payment for all/most
services delivered by
related providers for a
time-delimited “episodeof-care” (e.g., hip
replacement surgery and
rehab)
Payment for all/most
services delivered by
related providers to a
heterogeneous population
(e.g., Medicare’s Medicare
Advantage program)
Drugs
No universal approach to including drugs in the payment amount
Potential
Value/Cost
Savings
Focuses on improving
efficiency and not
exceeding budgeted
payment amount
DRG = Diagnosis-related group
Promotes provider
collaboration to better
coordinate care and
reduces duplication of
services
Makes spending more
predictable and allows for
implementation of
population healthoptimizing interventions
Public Programs Have Demonstrated Interest in
New Payment Models
Bundled Payments for Care
Improvement Initiative1
Payment Model
Design of the
Payment
Bundled
Payment
4 payment model options: 1) Retrospective
Acute Care Hospital Stay Only; 2)
Retrospective Acute Care Hospital Stay
plus Post-Acute Care; 3) Retrospective
Post-Acute Care Only ; 4) Prospective
Acute Care Hospital Stay Only
Disease Areas of Proposed by applicants
Focus
Medicare ESRD
Bundled Payment2
Bundled
Payment
Medicare Acute Care Episode
Demonstration3
Bundled
Payment
Single unit of payment for
most services and drugs in
dialysis facilities; physician
services excluded
Episode of care payment for
physician services pertaining to the
inpatient stay for Medicare fee-forservice beneficiaries
ESRD
Specified cardiovascular and/or
orthopedic procedures
Implementation
Model 1 could start as early as 1st quarter
2012. The other models do not have start
dates yet
Began January 1, 2011,
Began in 2009 and will end in 2012
with full implementation by
January 1, 2014
Quality
Incentives
Proposed by applicants and to be
approved by CMS
2% payment reduction for
facilities that do not meet
quality standards
Exact payment incentive amounts
vary by site and demo agreement
with CMS
CMS has not yet developed an oncology-focused payment model, but may consider looking into this
in the future, as cancer is a high cost disease area for the Medicare program
CMS = Centers for Medicaid and Medicare Services
ESRD = End-stage renal disease
1) Centers for Medicare & Medicaid Innovation, Bundled Payments for Care Improvement Initiative . Available at: http://www.innovations.cms.gov/documents/payment-care/Request_for_Applications.pdf
2) CMS, ESRD proposed rule, Available at: http://www.gpo.gov/fdsys/pkg/FR-2010-08-12/pdf/2010-18466.pdf
3) CMS. Medicare Acute Care Episode Demonstration, Available at: http://www.cms.gov/DemoProjectsEvalRpts/downloads/ACE_web_page.pdf .
PCMHs Could Be a Potential New Payment and Delivery
Model for Oncology Services and Drugs
Model Description
PCMHs focus on integrated care delivery for patients
and serve to improve communication between
various care providers
Care management, use of evidence-based care
guidelines, and patient engagement and education
are hallmarks of the PCMH model
While there are many PCMHs in existence, their role
and structure continue to evolve
Evidencebased
Medicine
“Whole”
Patient Care
Disease
Management
and Care
Coordination
Health
Information
Technology
Patient
Role of Oncologist
Few PCMHs are specialty-focused and, only one that
is oncology-focused has received recognition1
In most PCMHs, the oncologist serves as a “neighbor
to the PCMH” and is an external, contracted entity
The oncologist may develop a care plan for the
patient with the providers within the PCMH
Continuity of
Care Services
Healthcare
Team
1) American College of Physicians, Payment Methods for the PCMH, Available at: http://www.acponline.org/about_acp/chapters/ri/pch09_houy.pdf.
PCMH = Patient-Centered Medical Home
ACOs Could Be a Potential New Payment and Delivery Model
for Oncology Services and Drugs
Model Description
An ACO is an entity and a related
set of providers that agree jointly to
be held accountable for the cost
and quality of care delivered to a
defined patient population
ACOs must have a formal legal
structure with a governing board
responsible for measuring and
improving performance
Different Structures
ACO Model 1
IPA or
Primary
Care
Physician
Groups
ACO Model 2
ACO Model 3
MultiSpecialty
Group
Hospital
Medical Staff
Organization
(MSO) or
Physician
Hospital
Organization
(PHO)
Specialty
Groups
Hospital
Role of Oncologist
Oncologists are likely to be formal
ACO participants because of their
close relationship with patients
Oncologists also may play a role in
ACO governance
ACO = Accountable Care Organization
IPA = Independent Practice Association
Hospital
ACO Model 4
Integrated
Delivery
System
Medicare Shared Savings Program Final Rule
Program Overview
Snapshot
Program Design:
FFS + Shared
Savings
Sector:
Public/Private
Size: CMS expects
50-270 ACOs to
participate
Start Date: Will
begin accepting
applications
January 1, 2012
Status: Final Rule
Released October
20, 2011
Sponsor: CMS
Design: The Medicare Shared Savings Program, which promotes the formation
and operation of ACOs, is projected to begin January 1, 2012
» CMS finalized 33 quality measures for the first year; providers must meet
performance standards to be eligible for savings
» CMS will assign beneficiaries to an ACO based on where the patient
receives a plurality of primary care services from primary or non-primary care
physicians
– This change from the proposed rule allows the inclusion of specialists
in the assignment of beneficiaries to an ACO
Payment for Drugs and Services
Providers continue to receive FFS payments and are eligible to receive payments
for shared savings if the ACO meets certain performance standards and cost
savings; ACOs may choose between two tracks:
» An upside-only ACO model that will be eligible to share up to 50% of any
Medicare savings below its benchmark
» A two-sided ACO model that will be eligible to share up to 60% of any
Medicare savings below its benchmark or be required to repay any spending
above its benchmark
Drug reimbursement does not change; however cost shifting to drugs covered
under the pharmacy benefit or therapeutic substitution might occur
Source: Centers for Medicare and Medicaid, Medicare Shared Savings Program Final Rule Available at:
http://www.ofr.gov/OFRUpload/OFRData/2011-27461_PI.pdf
Coding and Billing 2012
Multiple Layers of Audits – Federal Medicare
RAC
MAC
Incorrectly
Billed Claims
Processing Errors
X
X
X
X
X
X
X
PSC/ZPIC
CERT
MAC Billing
Audits
59
Medical
Necessity
X
X
X
Office of Audit
Services
Audits
Annual Work
Plan Projects
X
X
Large $ Items
X
X
onPoint Oncology LLC
Incorrect
Payment
Amounts
Non-covered
Services
Incorrectly
Coded
Services
Duplicate
Services
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
Don’t Be Caught
Unaware……...
Be Prepared!
60
onPoint Oncology LLC
ICD-9-CM
10/1/2011
For more see…http://www.cdc.gov/nchs/icd/icd9cm_addenda_guidelines.htm
This for Cancer Practices and Clinics only
61
onPoint Oncology LLC
ICD-9-CM New Codes 10/1/2011
154.2 Malignant neoplasm of anal canal
173.10 Unspecified malignant neoplasm of the
skin of the lip
173.01 Basal cell carcinoma of the skin of the lip
173.02 Squamous cell carcinoma of skin of the lip
173.09 Other specified malignant neoplasm of the
skin of the lip
62
onPoint Oncology LLC
ICD-9-CM New Codes 10/1/2011
173.10 Unspecified malignant neoplasm of the
eyelid, including the canthus
173.11 Basal cell carcinoma of the eyelid,
including the canthus
173.12 Squamous cell carcinoma of skin of the
eyelid, including the canthus
173.19 Other specified malignant neoplasm of the
eyelid, including the canthus
63
onPoint Oncology LLC
ICD-9-CM New Codes 10/1/2011
173.20 Unspecified malignant neoplasm of the
skin of the ear and the external auditory canal
173.21 Basal cell carcinoma of the skin of the ear
and the external auditory canal
173.22 Squamous cell carcinoma of skin of the
ear and the external auditory canal
173.29 Other specified malignant neoplasm of the
skin of the ear and the external auditory canal
64
onPoint Oncology LLC
ICD-9-CM New Codes 10/1/2011
173.30 Unspecified malignant neoplasm of the
skin of other and other unspecified parts of the
face
173.31 Basal cell carcinoma of the skin of other
and other unspecified parts of the face
173.32 Squamous cell carcinoma of skin of other
and other unspecified parts of the face
173.39 Other specified malignant neoplasm of
other and other unspecified parts of the face
65
onPoint Oncology LLC
ICD-9-CM New Codes 10/1/2011
173.40 Unspecified malignant neoplasm of the
scalp and skin of neck
173.41 Basal cell carcinoma of the skin of the
scalp and skin of neck
173.42 Squamous cell carcinoma of skin of the
scalp and skin of neck
173.49 Other specified malignant neoplasm of the
scalp and skin of neck
66
onPoint Oncology LLC
ICD-9-CM New Codes 10/1/2011
173.50 Unspecified malignant neoplasm of skin of
trunk, except scrotum
173.51 Basal cell carcinoma of skin of trunk,
except scrotum
173.52 Squamous cell carcinoma of skin of trunk,
except scrotum
173.59 Other specified malignant neoplasm of
skin of trunk, except scrotum
67
onPoint Oncology LLC
ICD-9-CM New Codes 10/1/2011
173.60 Unspecified malignant neoplasm of skin of
the upper limb, including shoulder
173.61 Basal cell carcinoma of skin of the upper
limb, including shoulder
173.62 Squamous cell carcinoma of skin of the
upper limb, including shoulder
173.69 Other specified malignant neoplasm skin
of the upper limb, including shoulder
68
onPoint Oncology LLC
ICD-9-CM New Codes 10/1/2011
173.70 Unspecified malignant neoplasm of skin of
lower limb, including hip
173.71 Basal cell carcinoma of skin of lower limb,
including hip
173.72 Squamous cell carcinoma of skin of lower
limb, including hip
173.79 Other specified malignant neoplasm skin
of lower limb, including hip
69
onPoint Oncology LLC
ICD-9-CM New Codes 10/1/2011
173.80 Unspecified malignant neoplasm of other
specified sites of the skin
173.81 Basal cell carcinoma of other specified
sites of the skin
173.82 Squamous cell carcinoma of other
specified sites of the skin
173.89 Other specified malignant neoplasm of
other specified sites of the skin
70
onPoint Oncology LLC
ICD-9-CM New Codes 10/1/2011
173.90 Unspecified malignant neoplasm of
unspecified sites of the skin
Malignant neoplasm of the skin, NOS
173.91 Basal cell carcinoma of skin, site
unspecified
173.92 Squamous cell carcinoma of skin, site
unspecified
173.99 Other specified malignant neoplasm of
skin, site unspecified
71
onPoint Oncology LLC
ICD-9-CM New Codes 10/1/2011
284.11 Antineoplastic chemotherapy induced
pancytopenia
284.12 Other drug induced pancytopenia
284.19 Other pancytopenia
286.52 Acquired hemophilia
286.53 Antiphospholipid antibody with hemorrhagic
disorder
286.59 Other hemorrhagic disorder due to intrinsic
circulating anticoagulants, antibodies, or inhibitors
Antithrombinemia
Antithromboplatinemia
Etc.
72
onPoint Oncology LLC
ICD-9-CM New Codes 10/1/2011
996.88 Complications of stem cell transplant
999.32 Bloodstream infection due to Central
Venous Catheter
999.33 Local infection due to Central Venous
Catheter
999.34 Acute infection following transfusion,
infusion, or injection of blood and blood products
73
onPoint Oncology LLC
ICD-9-CM New Codes 10/1/2011
999.41 Anaphylactic reaction due to
74
administration of blood and blood products
999.42 Anaphylactic reaction due to vaccination
999.49 Anaphylactic reaction due to other serum
999.51 Other serum reaction due to
administration of blood and blood products
999.52 Other serum reaction due to vaccination
999.59 Other serum reaction due to other serum
V58.68 Long-term (current) use of
biphosphonates
onPoint Oncology LLC
CPT Changes 2012
Changes to Observation Codes (99218-99220)
for time.
38232: Bone marrow harvesting for
transplantation: autologous
77424-77425: Intra-operative radiation treatments
75
onPoint Oncology LLC
CPT Changes—Infusion Coding
Changes to Preamble—not much of it is new, but
just further explained.
96360-96379, 96401-96402, 96409-96425, 96521-
96523 are not to be reported by a PHYSICIAN in a
facility setting.
EM should be appended with -25 with 9636096549, if separately identifiable office or other
outpatient EM is performed.
76
onPoint Oncology LLC
CPT Changes-Infusion Coding
INITIAL INFUSION
Do not report an initial infusion due to a re-start of
an intravenous line, an IV rate requiring 2 lines for
implementation, or for accessing the port of a
multiple lumen catheter.
The difference in time and effort in providing this
second IV is using an initial code with -59. Example
96365, 96365-59.
77
onPoint Oncology LLC
CPT Changes—Infusion Coding
SEQUENTIAL INFUSIONS
All sequential infusions need to those of a new
substance/drug. The one exception is that facilities
(HOSPITALS) may report sequential infusions of
the same drug using 96376, if infusions are more
than 30 minutes apart.
CONCURRENT INFUSIONS
Clarified better that 96368 is not time-based and
can only be reported once per day.
Clarified that it is the infusion of a NEW substance/
drug.
78
onPoint Oncology LLC
CPT Changes—Infusion Coding
Multiple Infusions of the SAME DRUG
Must be over 30 minutes as has been true since
2006 (2005 for Medicare)
The sequential or subsequent infusions of the
SAME drug should be reported based on the time of
the infusion using the applicable add-on code.
Example—A hospital patient is given a one-hour infusion
every eight hours in 24 hours. 96365 is used for the initial
infusion with 96366 is reported twice for the second and
third infusions.
HYDRATION codes should not be used in a ‘keep
open’ situation or as a free flowing IV during a
chemotherapeutic or therapeutic infusion.
79
onPoint Oncology LLC
CPT Changes-New Patient
More clarification of what a new patient is
A new patient is one who has not received
professional services from the same EXACT
specialty and subspecialty in the same group
practice in the last three years.
Professional services are face-to-face services.
80
onPoint Oncology LLC
HCPCS 2012--Added
Plus, HCPCS Code. J0897 – Injection, denosumab, 1 mg
81
onPoint Oncology LLC
HCPCS 2012-Changes
82
onPoint Oncology LLC
HCPCS 2012--Changes
S0353
Cancer treatment plan initial
TREATMENT PLANNING AND CARE COORDINATION MANAGEMENT
FOR CANCER INITIAL TREATMENT
ADD
I
4/1/12
S0354
Cancer treatment plan change
TREATMENT PLANNING AND CARE COORDINATION MANAGEMENT
FOR CANCER ESTABLISHED PATIENT WITH A CHANGE OF REGIMEN
ADD
I
4/1/12
S-codes are Not paid by Medicare
Usually used by the Blues
Check with your payer before using
83
onPoint Oncology LLC
Other Important Deadlines
HIPAA 5010 1/1/2012
Advanced Imaging Accreditation 1/1/2012
ICD-10-CM 10/1/2013
84
onPoint Oncology LLC
Medicare Implementation of 5010 – Common Edits and
Enhancement Module (CEM)
Standardized Claim Editing
One set of edits per line of business
Consistent editing
Consistent results
Standardized Error Handling
TA1
999
277CA
Receipt, Control and Balancing
Claim Number Assignment
Medicare Implementation 5010
Changes to core processing system
Increase quantity from 999.9 to 9999.9
NPI validation
NDC detail
Room for ICD-10
Medicare Secondary Payer (MSP) balancing edits
90 day compliance extension, but does not mean
you do not have to be on board
Pharmacy billing for drugs provided “incident to”
a physician service
MM 7397, revised 12/16/11
“Pharmacies, suppliers and providers may not bill
Medicare Part B for drugs dispensed directly to a
beneficiary for administration “incident to” a physician
service…. These claims will be denied.”
"Pharmacies may not bill Medicare Part B for drugs furnished
to a physician for administration to a Medicare beneficiary.
When these drugs are administered in the physician's office to
a beneficiary, the only way these drugs can be billed to
Medicare is if the physician purchases the drugs from the
pharmacy.”
Pharmacy billing for drugs provided “incident to”
a physician service
Effective and implementation dates have been
changed from January 1, 2012 to January 1,
2013
http://www.cms.gov/Transmittals/downloads/R2368
CP.pdf
Your To Do List… Right Now
Notice all 5010 problems and get them fixed.
Ascertain your vendor’s plan for Meaningful Use
89
for implementation in 2012.
Understand the PQRS and EHR relationship in
2012.
Make sure have a compliance plan in place.
Audits are one way health reform is financed!!!
Don’t think you do not have to prepare for ICD10…it will be here before you know it…
Participate in the struggle—can you afford
another cut or even a hold?
onPoint Oncology LLC
CAN Web Site
The latest news
Forms
Regulations
Newsletters
Presentations
http://can.communityoncology.org
90
onPoint Oncology LLC
CONTACT INFO
Contact
bbuell@covad.net
bobbibuell1@yahoo.com
800-795-2633
Newsletter is free!
Go to our website: http://www.onpointoncology.com
onPoint Oncology LLC
91
THANK YOU FROM ONPOINT ONCOLOGY LLC!
onPoint Oncology LLC
92