File
advertisement

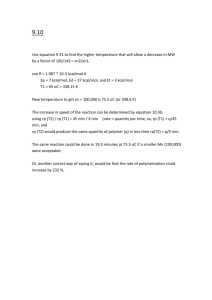
NUT 4700 MNT I Case Study 1: Malnutrition and Depression Copy and paste the questions at the end of this case study to a Word document. Type your answers, and turn in a hard copy in class on the due date as noted on the syllabus. You will also submit your case study into Blackboard Learn. Note that there are terms that you may need to look up. In addition, you will need to identify the information relevant to the nutrition assessment (not all information in medical records is pertinent to nutrition – part of the assessment is judging what the relevant information is.) Case Presentation ML is an 80 year old widower who was brought to his primary care physician’s office by the local Older Americans Transportation Service. He had missed his two prior scheduled office visits because of the recent death of his wife and a subsequent fall, which resulted in an intertrochanteric fracture of his right hip. On presentation, ML appeared withdrawn and much frailer than on previous visits. He answered in a monotone with terse, nonspontaneous speech, and he lacked expression. When asked about how he has been coping after the loss of his wife, he became tearful. He admitted that, in addition to the loss of companionship, his wife had done all of the cooking and grocery shopping which has caused additional hardship. Past Medical History ML tripped on the steps in his house 2 months ago and fractured his hip. He underwent an open reduction/internal fixation surgery to repair the fracture, and the operation went well. He had no serious operative complications, but he lost approximately 250cc blood during the procedure (1 unit = 500cc). ML underwent inpatient rehabilitation for 10 days after discharge from the surgical service and then returned home, where he lives alone. He ambulates slowing with a cane and can climb stairs only with difficulty. During his inpatient rehabilitation stay, he was diagnosed with depression and was started on an antidepressant. He has no major chronic diseases except for osteoporosis, discovered at the time of his hip fractures 2 months ago. ML had an appendectomy at age 46 and bilateral cataract surgeries 10 years ago. He has no previous history of pneumonia, tuberculosis, hepatitis, or urinary tract infection. Medications ML is currently taking fluoxetine (Prozac), 20mg daily, for depression and an iron supplement for anemia three times per day. He also self-medicates with over the counter (OTC) ibuprofen (200-400mg three times a day) and frequently uses OTC laxatives and glycerin suppositories for constipation, which he attributes to the iron tablets. He does not take a multiple vitamin, calcium or vitamin D. He has no known food allergies. Social History ML lives alone in the four-bedroom, two-story home that he has occupied since he married 55 years ago. His son and daughter both live out of state. Although they call him every few weeks, they have not visited since his wife’s death. ML also explains that he used to attend church and visit the local senior center regularly with his wife but has not been to either lately. ML explains that he has no energy to “get up and go” anymore and he falls asleep in front of the television. He also reports being constipated and that his food does not have much taste. He avoids alcohol and tobacco and drinks three cups of coffee daily. Review of Systems General: Weakness, fatigue, weight loss, and depression. Mouth: Food lacks taste (hypoguesia); dry, “thick-feeling” tongue; sores in corners of mouth. Gastrointestinal (GI): Poor appetite, constipation. Extremities: Hip pain when climbing stairs, some tenderness at old incision site, and chronic low back pain Physical Examination Vital Signs Temperature: 97.0 deg F Heart rate: 88 BPM Respiration: 18 BPM Blood pressure: 130/80 mm Hg Height: 5’11” Current weight: 145 lb Usual weight: 170 lb General: Thin, elderly man who is appropriately conversant but withdrawn. He is well groomed, but his clothes are loose fitting, suggesting weight loss. Skin: Warm to touch, patches of dryness and flaking to elbows and lower extremities Head, ears, eyes, nose, throat (HEENT): Temporal muscle wasting, no enlargement of thyroid Mouth: Ill-fitting dentures, sore beneath bottom plate, cracks/fissures at corners of mouth (angular cheilitis) Cardiac: Regular rate at 88 BPM Abdomen: Well-healed appendectomy site scar, no enlargement of liver or spleen, diffusely diminished bowel sounds. Extremities: Well-healed hip surgery incision with slight surrounding erythema, no sores on feet, traces pretibial edema to both lower extremities Rectal: Hard stool in vault, stool test for occult blood negative Neurologic: Alert, good memory, no evidence of sensory loss Gait: Slightly wide-based with decreased arm swing, antalgic and tentative but with safe, appropriate use of cane Laboratory Data Albumin: 2.5 g/dL (normal 3.5-5.8g/dL) Hemoglobin: 11.0 g/dL (normal 11.8-15.5 g/dL) Hematocrit 33.0% (normal 36-46%) ML’s 24 hour dietary recall: At his physician’s request, ML provided the following 24 hour recall, stating that this represents his usual daily intake: Breakfast (home) 1 Jelly donut 1 slice white toast 2 tbsp Jelly 1 cup coffee Lunch (home) 1 cup chicken and noodle soup 3 saltine crackers 2 butter cookies 1 cup coffee Dinner (home) 1 slice white bread 2 tbsp jelly 2 tbsp peanut putter 2 butter cookies 1 cup coffee Total kcals: 1270 Protein: 25 gm/day (8% of kcals) Fat: 42 gm (30% of kcals) Carbohydrate: 201 gm (62% of kcals) Calcium 153mg Iron 4 mg Kelsey Starck HCM 4700-01 Case Study 1 Questions 1. Calculations: a. BEE (using Mifflin St Jeor and Harris Benedict- compare the results) RMR Mifflin= (9.99 x weight) + (6.25 x height) – (4.92 x age) + 5 = (9.99 x 65.91kg) + (6.25 x 180.34cm) – (4.92 x 80) + 5 =1396.97 kcal/day RMR HBE= 66+ (13.7 x weight) + (5 x height) – (6.8 x age) = 66 + (13.7 x 65.91 kg) + (5 x 180.34cm) – (6.8 X 80) = 1326.67 kcal/day b. Total energy needs for repletion (weight gain) Weight gain = (HBE X AF) + 500 kcal/day Activity Factor (AF) = 1.2 (sedentary) 500 kcal/day = 3,500 kcal/ wk = 1 pound / week = (1326.67 kcal/day x 1.2) +500 kcal/day = 2,092 kcal/day I decided to use HBE and an activity factor because it gave me the closest estimate of ML’s calories expended per day. Because ML needs to gain weight, and gaining one pound a week is healthy weight gain, 500 kcal /day must be added to his diet. c. Protein needs RDA= 1.2 g/kg =(1.2 g/kg)(65.91kg) =79.08 g/day d. Fluid needs >75years = 30 ml/kg (30 ml/kg) (65.91kg)= 1,977 ml/day e. Ideal body weight 106lbs + 6lbs every inch over 60in) +/- 10% 106 + 66 = 172 pounds +10% : 189.2 pounds -10%: 154.8 pounds f. Percent ideal body weight (current / IBW) x100 (145/ 172) x 100 = 84.3% g. Percent usual body weight (current / usual) X100 (145/ 170) x 100 = 85.3% Evaluation: moderately/ mildly underweight h. BMI (kg/ (m^2) =(65.91/ 1.803^2) = 20.27 18.5 – 24.9 = Normal BMI 2. What do ML’s BMI and percent weight change indicate about his nutritional status? Percent weight change= (current wt – usual wt) / usual wt =(145- 170) / 170 = -14.7% ~ 14.7% BMI= 20.27 ML’s percent weight change and BMI indicate that he has lost a significant amount of weight recently, 14.7%. Although he has lost this weight, which is concerning, his BMI still falls within normal values of 18.5 – 24.9. BMI is not usually a good indicator of nutritional status because it is likely that ML is malnourished, based on other lab values, even though his BMI is normal. Percent weight change is a better indicator of nutritional status because it is known that unintentional weight lost is a sign towards malnutrition. ML did not plan his weight loss, and therefore indicates that his nutritional status isn’t normal. 3. What nutrition-related issues do his lab values indicate? -Albumin: ML’s albumin results of 2.5 g/dL are significantly lower than normal (3.5 g/dL – 5.8 g/dL). This most likely indicates chronic malnutrition. Because there is no storage of protein, when a patient is chronically malnourished the body begins pulling active visceral and somatic proteins to make glucose to fuel the brain, via gluconeogenesis. Albumin is a visceral protein. Albumin has a long half-life, and will show nutritional habits three months prior, therefore marking its chronic nature. It is important to realize, however that low albumin levels could mark liver disease and dehydration. The albumin levels alone do not suffice for a malnutrition diagnosis. -Hemoglobin & Hematocrit: ML’s hemoglobin (11.0 g/dL) and hematocrit (33%) levels were slightly under normal values. Hemoglobin and hematocrit lab values help diagnosis anemia and evaluate the number of red blood cells. These levels change in regards to patient’s hydration level, and can help diagnosis many issues including bone cancer, anemia, dehydration, and inflammatory diseases. If ML is anemic, which is diagnosed from complete blood count test, it is likely that he is low in iron, folate and Vitamin B12. Anemic patients usually present with fatigue and weakness, as ML does. It is noted that ML currently takes iron supplement. 4. Would a functional assessment of this patient yield any extra valuable information? Justify your answer. -It is noted in the physician’s note that ML presents with temporal muscle wasting, which is a clear sign of malnourishment. Further functional testing will be beneficial in helping diagnosis of malnutrition. Clavicle assessment and shoulder assessment will provide registered dietitian with further information regarding muscle wasting. Muscle wasting is prevalent in malnourished people because when one is energy deficient, the body will break down somatic proteins in muscle to help fuel the body. Muscle wasting is prevalent in marasmus, and therefore functional assessments are vital to determine this. 5. What medical, environmental, and social factors have led to nutritional problems in this patient? -ML’s depression diagnosis contributes to his nutritional problems because it is likely he doesn’t feel motivated to eat. ML suffers from constipation and may want to avoid foods that will prolong constipation symptoms. Potential chronic pain from fractured hip will lower desire to eat. -Recently ML fractured his hip and spent 10 days in an inpatient rehabilitation facility. It is likely he did not prefer food available. ML lives in a two-story house, it is noted that ambulating is difficult; therefore traveling to the grocery store to obtain food would be difficult. ML does not live close to family that can help him prepare meals. -Socially, ML just lost his wife and is now living alone. ML’s wife did all of the cooking, and without her he doesn’t get groceries or cook. ML no longer goes to church or senior center. 6. What general conclusions can you draw regarding the adequacy of his current diet? -According to ML’s 24-hour dietary recall his usual daily intake excludes all fresh fruits and vegetables and lacks a significant amount of protein. As calculated in 1c, ML requires 79.08 g/day of protein. ML is only consuming 25 g/day of protein, and therefore is not consuming adequate amounts of protein per day. The current RDA for carbohydrates is 130 g/day and ML is consuming 201 g/day. ML is exceeding his carbohydrate need. As calculated in 1a, according to ML’s current BW he should be consuming at least 1397 kcal/day to maintain his current weight, and ML is only consuming 1270 kcal/day. Therefore, ML is losing weight, instead of gaining weight. ML must increase calorie intake per day to 2,092 kcal/day (see 1b) to gain weight. ML’s current diet is absolutely not adequate to support his nutritional needs. 7. How can ML’s diet be improved to meet his energy requirements, achieve weight gain, and relieve constipation? Plan a 1-day menu with specific amounts of foods and times to eat that would improve ML’s nutritional status. -ML’s diet can be improved to meet his energy requirements, achieve weight gain and relieve constipation by incorporating fresh fruits and vegetables, and adding higher calorie founds containing protein. Furthermore, ML needs to meet his fluid requirement by addition of water and fibrous juices in his diet. 8am: Breakfast -1 glass of prune juice (120kcal, 29g CHO, 2g protein) -1 cup of coffee -1/2 grapefruit w/ sugar (60kcal, 1g protein) -1 piece of whole grain toast (85kcal, 4.35 g protein, 13.9 g CHO) -2T peanut butter (188kcal, 8g protein, 6.3g CHO) Breakfast Total: 465kcal 49.2 g CHO 15.35 g Protein 10am: Snack #1 -1 apple (130kcal, 0g protein, 30.8g CHO) -2T peanut butter (188 kcal), 8g protein, 6.3g CHO) Snack Total: 318 kcal 37.1 g CHO 8 g protein 12pm: Lunch -Turkey Sandwich (297 kcal, 25g protein, 43g CHO) -2 Butter cookies (200kcal, 2g protein, 29g CHO) -1cup carrots (30kcal, .5g protein, 7g CHO) Lunch Total 527 kcal 27.5 g Protein 79 g CHO Dinner: 5pm -Italian sausage (286 kcal, 15.9g protein, 3.5g CHO) -Spaghetti and sauce: (444kcal, 18g protein, 44g CHO) -Garlic bread: (160kcal, 4g protein, 22g CHO) Dinner Total 890 kcal 37.9 g protein 69.5 g CHO Day Total 2200 kcal/day 243.3 g CHO 117.85g protein In order for ML to gain weight, it is necessary to drastically increase his energy intake, CHO and protein intake. Gaining weight should be done healthfully, but it is important to provide ML with foods that he is interested in and he can easily make himself. It may be beneficial to provide ML with a weekly grocery list and resources that can deliver groceries to him. Educate the patient that prune juice, fresh fruits and vegetables will decrease his incidence in constipation. Overall energy intake will provide ML with more energy and likely make him feel better. Educate patient regarding simple ways to incorporate protein into meals using meats, peanut butter and nuts. Potential referral to occupational therapy could be beneficial to stimulate musculature via light lifting, and making tasks easier without his wife. *All nutritional data was found on www.caloriecount.about.com