Zoonotic Pathogens

Zoonotic Pathogens:
An Introduction
Dr. Emilo DeBess
Oregon Health Division
Dr. McKinley Thomas
Augusta State University
Zoonotic Diseases
• ...cause infections in animals and can be transmitted to humans
• …are typically endemic and occur in a natural foci
– However, ecologic changes and meteriologic or climate events can promote epidemic expansion of the host and geographic range.
History
• Interactions between animals and humans have occurred since the beginning of time.
• As animals became domesticated and a close bonds developed between animals and humans, the occurrence of zoonotic diseases increased.
Significant Zoonitic Pandemics
• 1700s, Mongols invaded Europe
• Mongols carried plague with them
• This lead to pandemic
“black death” or plague
• Killed 1/3 of European population
Significant Zoonitic Pandemics
• Early 1900’s
• “Spanish flu” transmitted from pigs to humans
•
Decimated 20 million people worldwide
•
Continues to pose a threat to humans
Contemporary Threats
• Potential Human Pathogens
–
E. coli 0157H7
–
Caliciviruses (evolved from the sea)
–
Bovine Spongiform Encephalopathy
(BSE) also known as “mad cow disease”
Etiology
• Today’s threat involving zoonotic diseases is considered to be partly due to human involvement in which the artificial multiplication of these pathogens can be used as biological terrorism.
Prevalence
•
Largely Unknown
•
Both serological studies and anecdotal discussion have been used to generate estimates
–
1997 a study trying to asses the prevalence of antibodies against Bartonella henselae and B. quintana was done at a veterinary conference. The results indicated that 7.1% of the veterinary population had antibodies which was no different from the general population studies at an earlier time.
Believed More Common
•
Ringworm caused by Trychophitum species. believed to be heavily under diagnosed / not reported
•
More prevalent among children
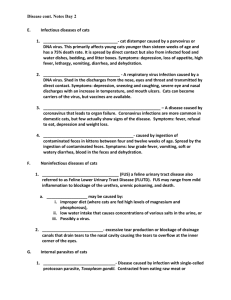
Common Zoonotic Diseases
• Bacterial
– Plague
– Cat Scratch Fever
– Salmonellosis
• Parasitic
– Toxoplasmosis
– Ring Worm
• Viral
– Hantavirus
– Prion
• BSE
Plague in Domestic Animals
• Exudates from buboes or respiratory secretions and sputum are highly contagious to humans
• Most cases of human pneumonic plague in the last two decades were acquired from infected cats
• Owners should control fleas on their pets and keep pets away from wildlife
Plague in History
• Pandemics in history involving Europe, Asia,
Africa
• “The Black Death,” thought to be caused by displeasure of the gods or other supernatural powers, heavenly disturbances
• The etiologic agent,
Yersinia pestis, first isolated in 1894 (Yersin and Kitasato)
Cat Scratch Disease
•
One estimate by the Centers for Disease Control found that there were 2.5 cases of CSD per
100,000 people per year in the United States.
•
In recent years, many studies have implicated the gram negative bacterium Bartonella
henselae as the primary (but not the sole) cause of CSD
•
Typically, a small skin lesion (resembling an insect bite) develops at the site of a cat scratch or
(less commonly) a bite, followed within two weeks by swollen lymph nodes and sometimes a fever.
Cat Scratch Disease
•
Cats are the main reservoir for B. henselae.
Surveys for B. henselae antibodies in cats in the
United States have found average infection rates to be from 25% to 41% in clinically healthy cats.
•
The lowest rates were in the Midwest and great plains regions (4-7%) and the highest were in the southeast (60%). Warmer, more humid climates are most supportive of fleas, which have been shown to transmit B. henselae from cat to cat.
•
It appears that the majority of cats do not become ill when they are infected with this bacterium and kittens are more commonly infected than adults.
Cat Scratch Disease
•
CSD is primarily a concern in homes with immunosuppressed people.
•
Since kittens are more likely to carry B.
henselae than adult cats, it is recommended that people with compromised immune systems adopt cats older than 1 year of age to reduce the risk of contracting CSD.
Cat Scratch Disease
• Since carrier cats are always healthy and multiple
• cases of CSD within a household are rare, euthanasia of a suspected carrier is not warranted.
• Onychectomy (declawing) is also not recommended, since infection can occur without a cat scratch.
• As is always the case, any cut or scratch should be promptly washed with soap and water.
Reptile-Associated
Salmonellosis
Reptile-associated Human Salmonella
History
1944 First Salmonella sp. isolate from snakes.
1946 First Salmonella sp. isolate from turtles and lizards.
1963 Turtle-associated salmonellosis first described.
1972 FDA regulation requiring certification of turtles for sale as
"Salmonella-free."
1974 Study shows 300,000 turtle-associated human salmonellosis cases per year in U.S.
1975 FDA bans sale of viable turtle eggs or live turtles with carapace length < 10.2 cm.
1977 CA State regulations ban sale, as above.
Reptile-Associated
Salmonellosis
•
In the United States, pet turtles were an important source of salmonellosis until commercial distribution of pet turtles less than 4 inches long was banned in 1975.
•
This ban led to a 77% reduction in the frequency of turtle-associated Salmonella serotypes isolated from humans during
1970-1976.
Reptile-Associated
Salmonellosis
•
Approximately 93,000 (7%) cases per year of Salmonella infections are attributable to pet reptile or amphibian contact.
•
An estimated 3% of households in the
United States have a reptile (CDC, unpublished data, 1999)
Reptile-Associated
Salmonellosis
•
Kansas. During April 1997, a 6-year-old boy had bloody diarrhea of 10 days' duration, abdominal cramps,vomiting, and fever (104.9 F
[41 C]). Stool culture yielded Salmonella serotype Typhimurium. The child was treated with ceftriaxone and amoxicillin / clavulanate.
•
Nine days after the boy started therapy, his 3year-old brother also developed diarrhea, and a stool sample yielded S. Typhimurium..
Reptile-Associated
Salmonellosis
•
No other family members became ill. The two boys shared a room with two corn snakes that they handled regularly. Stool cultures from the corn snakes yielded S.
Typhimurium.
•
The parents reported to health department staff that they were unaware that snakes are a source of salmonellosis
Salmonella Infection in Reptiles
• Numerous serotypes reported (5 or more may be isolated from a single reptile specimen).
• Latent infections with reactivation resulting in intermittent shedding
• Usually asymptomatic (wound infections, septic arthritis, endocarditis reported after inoculation via bites/scratches).
DIFFICULT TO IDENTIFY OR ELIMINATE CARRIERS.
Chiodini RJ, Am J Epidemiol 1981.
MMWR November 12, 1999
Recommendations to Prevent Human
Reptile-associated Salmonellosis
• Do not keep reptiles as pets where high risk individuals may be exposed such as infants, the elderly, and people with compromised immune systems.
• Thoroughly wash hands after any contact with reptiles, including handling of the animal or its cage.
• Confine reptiles to prevent environmental contamination. For example, keep reptiles off of floors and rugs where infants crawl and out of tubs and sinks where infants are bathed.
Toxoplasmosis
•
Toxoplasmosis is a disease caused by microscopic parasite called Toxoplasma gondii.
•
It is not a new disease, having first been discovered in 1908. Since its discovery, toxoplasmosis has been found in virtually all warm-blooded animals including most pets, livestock, and human beings.
•
Nearly one-third of all adults in the U.S. and in
Europe have antibodies to Toxoplasma, which means they have been exposed to this parasite.
Toxoplasmosis
• There are 3 principal ways Toxoplasmosis is transmitted:
• 1.Directly from pregnant mother to unborn child when the mother becomes infected with
Toxoplasmosis during pregnancy.
• 2.Consumption and handling of undercooked or raw meat from infected animals.
• 3.Ingestion of food or water or inhalation of dust contaminated with a very resistant form of
Toxoplasmosis called the oocyst.
Toxoplasmosis
•
Toxoplasma in meat can be killed by cooking at 152ºF (66ºC) or higher or freezing for a day in a household freezer.
•
Of all the infected animals tested, only cats are the perfect hosts for the production of the infectious and resistant
Toxoplasma oocysts.
Toxoplasmosis
•
There are two populations at high risk for infection with Toxoplasma; pregnant women and immunosuppressed individuals. In the United
States it is estimated that approximately 3,000 children are born infected with toxoplasmosis every year.
•
Although the majority of infected infants show no symptoms of toxoplasmosis at birth, many are likely to develop signs of infection later in life.
Loss of vision, mental retardation, loss of hearing, and death in severe cases, are the symptoms of toxoplasmosis in congenitally infected children.
Toxoplasmosis
5
Hantavirus Pulmonary Syndrome Cases by State of Residence
22
33
12
14
14
14
2
24
6
7
1
14
2
5
1
1 2
3
1
1
1
2
1
31 41
1
13
1
1
1
1 - 5 cases
6 - 10 cases
11 -15 cases
>15 cases
277 cases in 31 states
10/4/2000
Transmission of Hantaviruses
Chronically infected rodent
Virus is present in aerosolized excreta, particularly urine
Horizontal transmission of infection by intraspecific aggressive behavior
Virus also present in throat swab and feces
Secondary aerosols, mucous membrane contact, and skin breaches are also a consideration
• Non-specific flu-like prodrome
– fever, headache, myalgia, malaise,
GI, respiratory signs
• Thoracic radiographs: interstitial infiltrates
• Rapid progression to respiratory failure
– "leaky capillaries" -> noncardiogenic pulmonary edema
BSE
•Since 1996, evidence has been increasing for a causal relationship between ongoing outbreaks in Europe of a disease in cattle, called Bovine Spongiform Encephalopathy (BSE, or
"mad cow disease"), and a disease in humans, called new variant
Creutzfeldt-Jakob disease (nvCJD).
•Both disorders are invariably fatal brain diseases with unusually long incubation periods measured in years, and are caused by an unconventional transmissible agent.
Ringworm
•
Ringworm is a fungus infection of the scalp or skin. Symptoms include a rash that is often itchy and flaky
•
Ringworm is spread by direct contact with a person or animal infected with the fungus.
•
The same fungi that infect humans can also infect animals such as dogs, and cats, and infections may be acquired from pets as well as from infected children.
Bibliography
•
Swedish Institute of Infectious Disease
Control. (2001). Available: http://www.smittskyddsinstitutet.se/
•
Control of Communicable Diseases Manual
James Chin, MD 17 th edition
Centers for Disease Control and Prevention www.cdc.gov
We would like to acknowledge Michelle Jay, DVM,
MPVM for providing materials for this presentation
.