Sources of drugs
advertisement

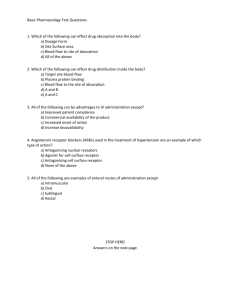
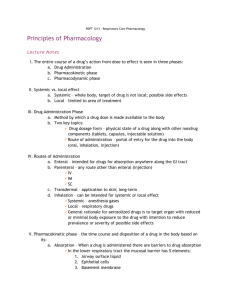
General Pharmacology Dr Nasim Ullah Siddiqui What is Pharmacology? • Pharmacology: – Pharmacon (drugs) + Logos (studies) – The study of drugs 2 Drugs & Medicines • Drugs: – Any substance that, when absorbed into the body of a living organism, alters (changes) normal body function – Examples: • • • • • 3 aspirin, Antibiotics, Nicotine, alcohol, Marijuana…. Drugs & Medicines • Medicines: – In pharmacology, a drug is a chemical substance used in the: • treatment, cure, prevention, or diagnosis of disease • Or used to enhance physical or mental wellbeing 4 Drugs & Medicines • Drug is called medicine when used in proper dosage form for safe administration • All medicines are drugs but all drugs are not medicines 5 Clinical / Experimental • Clinical Pharmacology – deals with the study of drug effects in humans beings, i.e. healthy volunteers and patients • Experimental Pharmacology – deals with the study of drug effects in laboratory animals • In vitro – Isolated tissue • In vivo – Intact organism Definitions • Toxicology: – deals with adverse (undesired) reactions of drugs & their treatment • Pharmacogenetics: – How genetics influence the mode of drug actions (e.g.. Metabolism) and biological variations of drug responses Definitions • Pharmacogenetics is generally regarded as the study or clinical testing of genetic variation that gives rise to differing response to drugs. • Pharmacogenetics refers to genetic differences in metabolic pathways which can affect individual responses to drugs, both in terms of therapeutic effect as well as adverse effects. 8 Definitions • Pharmacokinetics: – How the body handles the drug – Includes absorption, distribution , biotransformation, and elimination • Pharmacodynamics: – How drug handles the body – Deals with the biochemical and physiological effects of drugs on man Definitions Receptors • Biochemical receptors are large protein molecules that can be activated by the binding of a ligand (such as a hormone or drug). • Receptors can be membrane-bound, occurring on the cell membrane of cells, or intracellular, such as on the nucleus or mitochondrion. Binding occurs as a result of noncovalent /covalent interaction between the receptor and its ligand, at locations called the binding site on the receptor. 10 Definitions • Potency is a measure of drug activity expressed in terms of the amount required to produce an effect of given intensity. • A highly potent drug (e.g., morphine) evokes a larger response at low concentrations. • while a drug of lower potency (acetylsalicylic acid) evokes a small response at low concentrations • It is proportional to affinity and efficacy 11 12 Definitions • Affinity is the ability of the drug to bind to a receptor. • Efficacy is the relationship between receptor occupancy and the ability to initiate a response at the molecular, cellular, tissue or system level. • The response is equal to the effect(E), and depends on both the drug binding and the drugbound receptor then producing a response; thus, potency depends on both affinity and efficacy. 13 Definitions • The agonist (ligand, drug or hormone) that binds to the receptor and initiates the response. • The less the concentration of a drug is required to produce 50% of maximum effect and the higher the potency. 14 Definitions • A receptor antagonist is a type of receptor ligand or drug that does not provoke a biological response itself upon binding to a receptor, but blocks or dampens agonist-mediated responses. • The majority of drug antagonists achieve their potency by competing with endogenous ligands or substrates at structurally-defined binding sites on receptors. • Antagonists have affinity but no efficacy for their receptors, and binding will disrupt the interaction and inhibit the function of an agonist at receptors. 15 Antagonist • Antagonist activity may be reversible or irreversible depending on the longevity of the antagonist–receptor complex, which, in turn, depends on the nature of antagonist receptor binding. • Physiological antagonists, substances that have opposing physiological actions, but act at different receptors. For example, histamine lowers arterial pressure through vasodilation at the histamine H1 receptor, while adrenaline raises arterial pressure through vasoconstriction mediated by β-adrenergic receptor activation. 16 Definitions • Tachyphylaxis : Rapidly developed tolerance is tachyphylaxis, is a medical term describing a decrease in the response to a drug due to previous exposure to that drug. • Caused by depletion or marked reduction of the amount of neurotransmitter responsible for creating the drug's effect, or by the depletion of receptors available for the drug or neurotransmitter to bind to. Examples: Amphetamine, ephedrine (indirectly acting drugs) • Tachyphylaxis is characterized by the rate sensitivity i.e, a high-intensity prolonged stimulus or oftenrepeated stimulus may bring about a diminished response also known as desensitization. 17 Definitions • Physiological tolerance or drug tolerance is a subject's reaction to a drug (such as an opiates painkiller, benzodiazepine drug) is reduced at a later time even though the dose or concentration at the effect site is the same. • This means that larger doses are required to achieve the same effect. • Drug tolerance can involve both psychological & physiological drug tolerance factors. • It is reversible • Physiological tolerance occurs after repeated exposure . 18 Definitions • Idiosyncrasy (idiosyncratic drug reaction) denotes a non-immunological hypersensitivity to a substance, without connection to pharmacological toxicity. • Is an individual based on a specific condition of the one who suffers it. Most commonly, this is caused by an enzymopathy, congenital or acquired. 19 Drugs actions • Drug actions are mediated by 3 ways: 1. Acting on somatic or psychic processes or functions 2. Correction of deficiencies 3. Toxic action on pathogenic microorganism Ideal drug effects • Drug effects should be: – Selective – Temporary – Dose-related (controllable) – Show close relationship with bioavailability Drug Responses • How are drug responses produced? • By interaction with active binding sites called RECEPTORS – Drug may be agonist or antagonist for the receptors Nature of drugs • Physical: – Solid (aspirin) – Liquid (nicotine, ethanol) – Gas (nitrous oxide) • Chemical structure: – Protein, lipid, carbohydrate – To be weak acid or weak base – Amine (primary, secondary, tertiary, ..) Sources of drugs • Natural from: – Plants – Animals / Humans – Micro-organisms – Minerals – Inorganic metals • Semi-synthetic • Synthetic • Bio-synthetic Sources of drugs Natural from Plants: • Active principles are found in roots, leaves and seeds in 2 forms: – Glycoside, e.g • Cardiac glycoside Digoxin ( from the Foxglove plant) – Alkaloid, e.g • Morphine (from Poppy capsules), • Atropine (from Belladonna leaves) • Quinine (from bark of Cinchona tree) – Castor oil (from castor seed) Sources of drugs Natural from animals / humans: • Hormones: – Heparin from Pig or Ox liver, – Insulin from Pig or Ox pancreas – Gonadotrophins from urine of pregnant women • Plasma or serum from blood • Thyroxin from Pig or Ox thyroid gland • Cod Liver Oil from Cod fish Liver Sources of drugs Natural from micro-organisms: • Antibiotics: – Penicillin from Penicillium notatum, – Streptomycin from Streptomyces griseus, – Bacitracin from Bacillus Sources of drugs Minerals: • Calcium, Magnesium, Aluminium, Sodium, Potassium & Iron salts, • Liquid paraffin from petroleum. Inorganic metals: • Iodine, • Lithium, • Radioactive elements: I131 Sources of drugs Semi synthetic drugs: • Prepared by chemical modification of natural drugs in labs. – Ampicillin from Penicillin-G, – Semisynthetic cephalosporin's from 7amino cephalosporinic acid Sources of drugs Synthetic Drugs: • Prepared by chemical synthesis pharmaceutical laboratories – Sulphonamides – Salicylates – Barbiturates – Benzodiazepines in Sources of drugs Bio-Synthetic Drugs: • Prepared by cloning of human DNA into bacteria like E.Coli. Sources of drugs Bio-Synthetic Drugs: • Technique is called Recombinant DNA technology or Genetic Engineering – Cells from animals or human that produce active substance – Isolation of DNA – Transfer to bacteria (E-coli) by plasmids (Gene cloning) – A new E-coli synthesizes the new substance – Cloning of ‘new’ E-Coli means production of identical subjects like parent Sources of drugs Bio-Synthetic Drugs: • Examples: Human Insulin's, Human Growth Hormones, Human BCG vaccine , Human Hepatitis B Vaccine Criteria for drug classification 1. Chemical structure: – Cholinesters, – Organophosphates, – Catecholamine's 2. Location of action: – Cardiac glycosides, – Autonomic drugs Criteria for drug classification 3. Purpose of medication: – – – – 4. Antihypertensive Diuretic Antiemetic Analgesic Name of plant: – Opium alkaloids – Cardiac glycosides – Belladonna alkaloids Prescription / Over the counter • Drugs fall into two distinct categories: 1)Those that require a physician’s prescription to obtain (Rx) 2)Those that can be purchased over-the counter (OTC) • both are regulated by the regulatory authorities Pharmacotherapy • Employment of drugs for the prevention and treatment of diseases • Its scope: 1. 2. 3. Indications Contraindications Drug interactions • Therapy: – Radical (full healing) – Symptomatic (treatment of symptoms only) – Prophylactic (e.g. contraception, vaccine) Therapeutic Index • Therapeutic Index (TI): – Toxic dose / Effective dose • Indicates the relative safety of a drug • Examples: – Acetominophen : 27 – Valium: 3 – Methotrexate, vincristine: 1 • Narrow TI indicates the need for frequent blood tests to monitor drug levels Mechanism of Action • Agonist: – drug mimics an endogenous substance that would normally stimulate a receptor • Antagonist: – drug which binds a receptor site, doesn't stimulate it, but blocks other substances from stimulating it Drug Nomenclature Most drugs have at least three names: 1. Chemical name 2. Generic name (Official, Approved) 3. Proprietary name (Trade name, Company name) Drug Nomenclature 1. Chemical name – The chemical composition and structure Drug Nomenclature 2. Generic name (Official, Approved) – is usually the abbreviated form of the chemical name – this name is used and chosen by official bodies Drug Nomenclature 3. Proprietary name (Trade name, Company name) – the name given by the company which markets the drug – It is the commercial property of a pharmaceutical company – It indicates a particularly formulation of a particular substance by a particularly manufacturer Drug Nomenclature • Since several companies market the same drug under different proprietary names, unnecessary confusion may arise • Whenever possible drugs should be prescribed by their approved names – Chemical name: • Acetyl-p-aminophenol – Official name: • Paracetamol – Proprietary name: • Panadol, Calpol, Adol, Fevadol Routes of Drug Administration 45 Routes of Drug Administration • Factors Deciding Choice of Route 1. Type of described effect, systemic or local 2. Physiochemical properties, solid or insoluble 3. Rapidity of effect, oral, intramuscular (IM), intravascular (IV) 4. Condition of patient, conscious or unconscious, vomiting Topical Application - Mucous Membrane • Conjunctiva, nasopharynx , oropharynx, vagina, urethra, urinary bladder, ear, nose, anal canal for local / systemic effects • Absorption rapid • Local anesthetic for local effects rapidly absorbed, produce systemic toxicity • Types: – ointment, cream, drops, jelly, powder, tablet, suppository, pessary Topical Application - Skin • Absorption- depends on – surface area, lipid solubility • Few drugs readily penetrate skin • Burned, denuded, abraded, inflamed skin increase systemic absorption • Toxicity by highly lipid soluble insecticides • Controlled- release by topical patches Topical Application - Injection • Intra articular (in joint) – hydrocortisone • Intra thecal into subarachnoid space of L2-3 or L3-4, – Local anaesthetics • Subcutaneous (under skin) – Local anaesthetics • Intra arterial – anticancer drugs in limbs cancer Systemic Routes • Enteral through GIT – Orally – Buccal or sublingual – Rectal • Parental – Intravenous (IV) – Intramuscular (IM) – Subcutaneous (SC) – Transdermal Therapeutic system (TTS) – Inhalation Oral Ingestion /Swallowing • Tablets, capsules, powder, syrup, mixture suspension or emulsion • Absorption variable • Most conventional, economical, more safe and acceptable to patient • Absorption delayed, reduced after food • Not good for some drugs: – Gentamicin not absorbed – Insulin destroyed in gut Oral Ingestion /Swallowing • Absorption from stomach intestine is affected by: and upper – Surface area, – Blood flow to site of absorption, – Physical state: (solid, solution, suspension), – Water solubility, – Concentration at the site of absorption, – Rate of dissolution, – Rate of disintegration, – Particle size Sublingual • • • • Good, readily available Systemic effect Quick Example of a clinically useful drugs: – Nitroglycerine Rectal Administration • Used when recurrent vomiting or unconscious • 50% absorbed drug bypass liver • Absorption incomplete, irregular in lower rectum by external haemorrhoidal veins • Example: – indomethcin, steroids, soap water & barium sulphate as enema • Inconvenient & embarrassing • Rectal inflammation occurs Intravenous • Advantages: – Rapid reach and response – Life-saving in critical conditions (Blood, IV fluids) • Disadvantages / Precautions – Careful of too quick infusion – Anaphylactic shock – Can not withdraw medication once given • Example: – Blood transfusion, Antibiotics for rapid effect Intramuscular • Advantages: – Quick absorption and response – Easy to learn • Disadvantages / Precautions – Possible infection, or injury to nerve – Could not retrieve – Painful • Example: – Pain killer (Pethidine) Subdermal • Advantages: – Slow control release – Easy accessibility – Less painful • Disadvantages / Precautions – Not very effective – Not good if circulation not effective – Collapsed hypotensive patients • Example: – Insulin (bypasses digestion) Inhalation Drug Administration • Most common types: – Volatile liquids, gaseous anaesthetics and therapeutics gases – Metered dose aerosol inhaler • e.g. salbutamol – Compressed air driven nebulised solution inhaler Inhalation Drug Administration Pulmonary Absorption • Important route for drugs abuse • Access to circulation rapid – large surface area of lungs • • • • Fine drug droplets in air (aerosol ) inhaled Instantaneous absorption Avoids hepatic first-pass loss Local application at the desired site of action in pulmonary disease • Treatment of bronchial asthma Aerosol Delivery 59 Inhalation Drug Administration • Only 2-10 % dose deposited in lungs • 90 % dose is swallowed 60 Pharmacokinetics • Pharmacokinetics deal quantitative study of: – Absorption – Distribution – Biotransformation and – Excretion of drugs with the Pharmacokinetics Absorption: • is the process by which a drug is transferred from its site of entry to the volume of distribution • The rate of absorption affects the – Onset, – Duration, and – intensity of drug action Factors affecting drug absorption Drug-related factors: • Physical state • Particle size • Concentration • Dosage form (preparation) • Solubility (lipid and water solubility) • Degree of ionization Factors affecting drug absorption Host-related and other factors: • Transport (absorption) of drug – Passive transport (e.g. simple diffusion) – Specialized transport (e.g. active transport) • Circulation at the site of absorption • Area of absorbing surface • Presence of other agents Drug Distribution • The process by which a drug leaves the blood stream and enters the extracellular fluid and or cells of the tissues • Depends on: – Capillary permeability, – Degree of drug to plasma and tissue proteins, – Relative hydrophobicity of the drug Bioavailability • Bioavailability of a drug = availability of biologically active drug • Is the proportion of the active drug that reaches the systemic circulation (site of action) after administration – Helps in choosing “best drug” and “best route” of administration Bioavailability • The bioavailability of a drug may vary from one dosage form to another and for the same dosage form it may vary according to the pharmaceutical formulation. • The bioavailability is of great importance in therapeutics specially in the case of life saving drugs, antibiotics and drugs with a narrow margin of safety e.g. anticoagulants. • Differences in the rate of absorption may cause patients to be overmedicated or under medicated. 67 Factors Affecting Bioavailability • Quality Control in Manufacturing and formulation • First pass metabolism • Factors affecting absorption of drugs from GIT - These are pH of GIT fluids, area of absorbing surface, functional integrity of GIT, presence of food and other substances in stomach, blood flow, physiochemical properties of the drug. 68 Biotransformation • Chemical alteration which a drug undergoes within a living organism • Most of the substance (taken exogenously or produced endogenously) need a change in their forms, which changes their activity (increased, decreased or become inactive) and make them available for elimination from liver and kidney Biotransformation Metabolism of drugs may may change them from: • Inactive to active • Active to: – Less active – More active – Inactive Biotransformation Metabolism of drugs takes place in various organs: • Liver (most important) • Epithelial cells of GIT • Lungs • Kidneys • skin • brain Drug metabolism Extrahepatic microsomal enzymes (oxidation, conjugation) Hepatic microsomal enzymes (oxidation, conjugation) Hepatic non-microsomal enzymes (acetylation, sulfation,GSH, alcohol/aldehyde dehydrogenase, hydrolysis, ox/red) Drug metabolism Factors affecting drug metabolism: • Age • Sex • Genetic differences • Nutrition • Pathological conditions • Route of administration • Effect of drug on metabolism Drug elimination • The removal of drugs from the body • may occur from – Kidneys (most important), – Bile, – Intestine, – Lung, – Breast, – Skin M A J O R M I N O R Concept of “Half-Life” • Time required to metabolize 1/2 of the original dose of the drug • Use of this terms helps in determining how long a drug will remain in the body Concept of Critical Threshold • Defined as the minimum level of drug concentration needed for the desired therapeutic effect to be present. Elimination • Zero order: – Constant rate of elimination irrespective of plasma concentration. • First order: – Rate of elimination proportional to plasma concentration. Constant Fraction of drug eliminated per unit time. – Rate of elimination ∝ Amount – Rate of elimination = K x Amount Plasma Concentration (mg/l) Zero order elimination 1000 C 100 C/2 10 t1/2 1 0 1 2 3 4 5 6 Time (hr) t½ is the time for the plasma concentration to reach half the original, i.e., the half-life of elimination. First Order Elimination 14 12 Plasma concentration 10 C 8 t1/2 6 t1/2 C/2 4 C/4 2 0 0 5 10 TIME (hours) 15 20 Drug elimination • Elimination of drugs from the body usually follows first order kinetics with a characteristic half-life (t1/2) and fractional rate constant (Kel). First Order Elimination • Clearance: volume of plasma cleared of drug per unit time. • Clearance = Rate of elimination ÷ plasma conc. • Half-life of elimination: time for plasma conc. to decrease by half. • Useful in estimating: – Time to reach steady state concentration – Time for plasma concentration to fall after dosing is stopped. Plasma concentration Concentration due to repeated doses (infusion) Concentration due to a single dose The time to reach steady state is ~ 4 t1/2’s Plasma concentration • Drug concentration in plasma – Should be maintained within the specific drug therapeutic range 84 Plasma concentration • Drug concentration in plasma – Should always be maintained above the drug sub-therapeutic level 85 Plasma concentration • Drug concentration in plasma – Should always be maintained below the specific drug lethal dose level 86 Plasma concentration 87 Adverse Drug Reactions • Unwanted or unexpected effects of drug • Quite common but in most of the cases they are not serious • Occasionally they could be so serious as to endanger life e.g. – Acute anaphylactic shock with penicillin, – Severe hypoglycemia after excessive insulin administration Adverse Drug Reactions Adverse Drug Reactions Adverse Drug Reactions Adverse Drug Reactions • Adverse drug effects can be divided into two groups: • Predictable Reactions • Withdrawal symptoms or rebound responses Adverse Drug Reactions Predictable Reactions: a) Due to excessive pharmacological activity of the drug • They are liable to occur with CNS depressants cardio-active drugs, hypotensive agents and hypoglycemic drugs • All patients are at risk of developing this type of reaction if high doses are given • Patients with renal disease, liver disease and extreme of ages are particularly susceptible Adverse Drug Reactions Predictable Reactions: b) Withdrawal symptoms or rebound responses after discontinuation of treatment • Crisis may be precipitated by sudden stoppage of corticosteroid therapy • Withdrawal symptoms occur after narcotic analgesics, barbiturates and drugs liable to cause addiction • These drugs should be gradually withdrawn to avoid such mishaps. Adverse Drug Reactions Unpredictable Reactions: – They occur usually infrequently, and are not dose dependent. They are of following types: • Drug allergy: (e.g. to Penicillin) • Genetically determined: ( e.g. patients with G6PD deficiency may develop acute hemolytic anemia after anti-malarial drugs) • Idiosyncrasy: (unusual, unexpected, unexplained) Summary: Concept no 1 • Almost ALL DRUGS ARE POISONS • The only thing that determines if a drug provides a benefit or kills a patient is how we administer it Concept II : Our Therapeutic Goal • To achieve drug concentrations at the site of action (target tissue)…that are sufficiently high enough…to produce the intended effect without producing adverse drug reactions (or with minimal adverse reactions) Summary What happens after drug administration? Drug at site of administration 1. Absorption Drug in plasma Drug metabolites in tissues 3. Metabolism Drug metabolites In urine, feces, bile 98