Treatment - IS MU - Masaryk University
advertisement

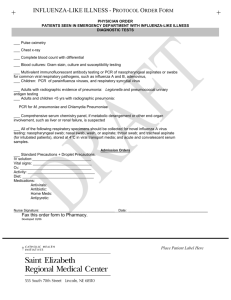
Institute for Microbiology, Medical Faculty of Masaryk University and St. Anna Faculty Hospital in Brno Agents of respiratory infections – I + II Ondřej Zahradníček (with use of prof. Votava's slideshows from 2011) Lecture for 3rd-year students 21st of September, 2012 Significance of respiratory diseases The most significant infections in general practitioner‘s office (respiratory tract = an ideal incubator) Big economic effect on the economics (people stay home, including mothers of ill children) They tend to be seen in collectives and often produce outbreaks and epidemics ¾ of respiratory infections (and even more in children) are caused by viruses Localization of infection in the respiratory tract The localization of infection in the respiratory tract – influences the clinical symptomatology – enables us to suspect specific agents Therefore, we have to distinguish – upper respiratory tract (URT) infections (and infections of adjacent organs ) – lower respiratory tract (LRT) infections (infections of lower respiratory ways and of lungs) (lungs are not a „way“, therefore they are often taken apart) Of course, it is also possible, that a disease influences more than one part together Respiratory infections – Classification: URT infections and LRT infections and lung infections of adjacent infections organs infection of epiglottis infections of nose a infection of larynx and nasopharynx trachea infections of oropharynx infection of bronchi incl. tonsillae infection of bronchioli infections of paranasal infections of lungs sinuses otitis media* For practical reasons they use to be taken here, as the sites of infection are conjunctivitis* related anatomically with the URT „Flu“ and influenza Commonly, acute respiratory infections are rhinitis, pharyngitis or mixed rhinopharyngitis (inflammations of nasal and pharyngeal cavities). Epidemiologists use an abbreviation „ARI“ – acute respiratory illness Many people describe this as a „flu“, but it is not a true influenza. True influenza rather attacks lower respiratory tract, it contains dry cough and whole-body symptomatology (fever, muscle pain). Nevertheless, similar symptomatology can be also seen in case of parainfluenzas and other diseases. Epidemiologists use abbreviation „ILI“ (influenza-like illness). . Common flora in respiratory ways Nasal cavity has no its specific flora, but it is usually colonized by skin bacteria (= staphylococci, coryneforms, especially the anterior part) or pharynx (the posterior part) The pharynx (similarly as oral cavity) contains neisseriae and streptococci (viridans group), usually haemophili, sometimes small amounts of pneumococci, meningococci etc. Lungs and LRT is usually microbes-free, but the specimens coming from here use to be contaminated by URT flora Rhinitis, rhinopharyngitis (or nasopharyngitis) acuta It is almost caused by viruses („common cold“). More than 50 % are caused by rhinoviruses, 2nd place have coronaviruses, other viruses may be also present (but NOT influenzavirus) Bacteria* may multiply secondarily; they are often patient‘s own bacteria from skin or pharynx. They disappear without treatment, antibiotic treatment is useless and usually also ineffective. *Staphylococcus aureus, Haemophilus influenzae, Streptococcus pneumoniae, Moraxella catarrhalis; in rather chronical cases: Klebsiella ozaenae, Klebsiella rhinoscleromatis In differential diagnostics, we should think about allergic and vasomotoric rhinitis http://www.drgreene.org/body.cfm?xyzpdqabc=0&id=21&action=detail&ref=1285 http://www.bupa.co.uk/health_information/a sp/direct_news/general_health/rhinitis_240 706.asp Examination and treatment for rhinitis Examination is useless. Even mucopurulent secretion does not necessarily mean bacteriological examination, except long time durating secretion. The treatment is symptomactical (nasal drops for decongestion of the mucous membrane, tea etc.; even antipyretics are not very useful, as elevated temperature is helpful against viruses. Antibiotic treatment is not recommended. In borderline cases it is possible to use local antibiotic treatment (e. g. bacitracin + neomycin) Only for infection durating 10–14 days it is recommended to examinate nasal swab (to avoid skin contamination!) and to perform targeted antibiotic treatment Carriership of MRSA strains Nasal carriership of Methicilin-resistant Staphylococcus aureus strains (MRSA) is relatively common. It uses to be asymptomatic Treatment is not routinely recommended. Eradication of MRSA strains is quite difficult and often only temporary Nevertheless, sometimes we try to get rid of MRSA in nasal cavity, especially prior to surgery. Mupirocin is mostly used for this. Sinusitis acuta (inflamation of paranasal sinuses) Transient finding in sinuses is normal during common cold and it is not a reason for treatment (even if found in X-rays) Treatment is recommended in case of painful sinusitis with pain of teeth, head, fever, headache and durates at least a week, eventually nervus trigeminus is involved Although viral infection may be primary, the important causative agents are bacteria, almost Streptococcus pneumoniae and Haemophilus influenzae Sinusitis acuta http://www.drgreene.org/body.cfm?xyzpdqabc=0&id=21&action=detail&ref=1285 Examination and treatment of sinusitis Treatment should be started immediatelly, even without examination Drug of 1st choice is amoxicilin (e. g. AMOCLEN), an alternative is e. g. doxycycline (DOXYBENE), in children co-trimoxazol (BISEPTOL) Examination of nasal of pharyngeal swab is useless In case that we wish to perform targeted treatment, the only way is properly performed punction or sinus washing (usually on oto-rhinolarangological department of a hospital), of course, it should be washed by saline, not disinfectant! Middle ear inflammation – otitis media Middle ear is anatomically related to respiratory tract Common in children (short horizontal tuba auditiva) Agents: Streptococcus pneumoniae, Haemophilus influenzae, Moraxella catarrhalis, less commonly anaerobic bacteria In chronical inflamations also G– rods etc. It is necessary to differenciate – otitis media × otitis externa: In case of otitis externa, the causative agents are the same as for skin infections – almost Staphylococcus aureus. The treatment is local. Otitis media http://www.medem.com/MedLB/articl e_detaillb.cfm?article_ID=ZZZPMV6 D1AC&sub_cat=544 Examination and treatment of otitis media Treatment has a sense, if it is a really proven inflammation (pain, redness, fever) and it is not suppressed by anti-inflammatory treatment Drug of choice is again amoxicilin (e. g. AMOCLEN), an alternative co-trimoxazol Examination of external ear swab is a logical nonsense, except in case of perforated tympanon (spontaneously or artificially at paracentesis) Of course, in case of having pyogene liquid taken during paracentesis, it is recommended to examinate it microbiologically Etiology of conjunctivitis Conjunctivitis is usually of viral origin It usually accompanies acute URT infections In adenoviral infections typically: follicular conjunctivitis, pharyngoconjunctival fever (adenoviruses 3, 7), epidemic keratoconjunctivitis (adenoviruses 8, 19) Viral conjunctivitis of other origin: – hemorrhagic conjunctivitis (enterovirus 70) – herpetic keratoconjunctivitis (HSV) Treatment is usually only local Bacterial conjunctivitis – Acute suppurative conjunctivitis: S. pneumoniae, S. aureus, in children also other bacteria – Inclusion conjunctivitis: C. trachomatis D – K – Chronical bacterial conjunctivitis: S. aureus, C. trachomatis A – C (trachoma) – Allergic, mechanic (alien body) Acute tonsillitis and pharyngitis majority (70–85 %) viral (rhinoviruses, coronaviruses, adenoviruses, but also EB virus = infection mononucleosis) The most significant of bacterial ones (more than 95 % cases): accute tonsilitis caused Streptococcus pyogenes (group A haemolytical streptococcus). More bacteia: arcanobacteria, possibly also haemolytical streptococci of other groups, pneumococci etc. Rare, but important: diphtheria, gonorrhoea Viral tonsilopharyngitis http://upload.wikimedia.org/wikipedia/commons/thumb/b/b1/Pharyngitis.jpg/250px-Pharyngitis.jpg Tonsilopharyngitis http://medicine.ucsd.edu/Clinicalimg/Head-Pharyngitis.htm http://www.newagebd.com/2005/sep/12/img2.html Purulent (= pyogenic, puscontaining) bacterial tonsilitis http://www.meddean.luc.edu/lumen/MedEd/medicine/PULMONAR/diseases/pul43b.htm Pharyngitis: Examination and treatment A throat swab (tonsils swab) should be always performed to find the causative agens. (The fact that many GPs do not do it does not mean that this is the good way how to do it.) As it is usually not possible to wait for results of culture, in the same time CRP is examined (elevated in bacterial infections), the result is available soon Treatment should be targeted. In tonsillitis caused by Streptococcus pyogenes (huge majority of bacterial ones) the drug of choice is V-penicillin. Macrolids (RULID, KLACID, SUMAMED, AZITROX) should be used in allergic patients only Eventually serology of EB virus and cytomegalovirus might be examined in unclear subacute cases Dangers Many doctors think that they are able to distinguish clinically bacterial tonsillitis against the viral one. The research shows that it is not true in many cases. So, at least CRP examination ought to be done. Another common mistake is use of macrolids (KLACID, SUMAMED, RULID), although the patient is not allergic. It is not good: macrolids are bakteriostatic antibiotics only, the effectiveness of treatment is only 80–90 % (against 100 % for penicillin – in the Czechia, no strain resistant to penicillin was found until now!) Even use of ampicillinu or amoxicillin instead of penicillin is a mistake, especially when the examination was not performed. Aminopenicillins may cause hard damage in case of infection mononucleosis! Etiology of epiglottitis disease – medical emergency The child may suffocate! Serious One only really important causative agent: Haemophilus influenzae type b Treatment: transport to emergency unit, first aid, among antibiotics: 3rd generation cephalosporins Examination if often not performed (it might lead to a new disease attack), eventually blood culture is performed It is very rare now (vaccination) Epiglottitis de.wikipedia.org/wiki/Epiglottitis http://health.allrefer.com/health/epiglottitis-throat-anatomy.html Even George Washington died because of this disease www.fathom.com/course/10701018/session4.html Etiology of laryngitis and tracheitis Again respiratory viruses, but other than agents of nasopharyngitis: parainfluenza and influenza A viruses + respiratiory syncitial (RS) virus Bacteria are rather rare here: Chlamydia pneumoniae, possibly Mycoplasma pneumoniae Secondarily sometimes: Staphylococcus aureus and Haemophilus influenzae Laryngotracheitis pseudomembranosa (croup): Corynebacterium diphtheriae Lagyngitis acuta http://www.emedicine.com/asp/image_search.asp?query=Acute%20Laryngitis Examination and treatment of laryngitis and tracheitis No examination is needed, even possible. Throat swab is a nonsense, as the microflora in pharynx is different from larynx and trachea. In subacute or chronical states it is possible to examinate serum for antibodies againts respiratory viruses (and simillar agents) Treatment is almost symptomatical. Unlike very rare cases, antibiotics are not indicated www.cartoonstock.com/directory/l/laryngitis.asp www.cartoonstock.com/directory/l/laryngitis.asp www.cartoonstock.com/directory/l/laryngitis.asp Acute bronchitis and tracheobronchitis Acute bronchitis: – Caused almost only by viruses, influenza is a typical example. – Outbreaks in scholar childrend and young aduls may be caused by Mycoplasma pneumoniae. – Other bacterial species, like Streptococcus pneumoniae and Haemophilus influenzae, are not important here. When isolated from sputum specimen, their origin is probably in URT. Bronchitis acuta http://www.yourlunghealth. org/lung_disease/copd/nut shell/index.cfm http://www.lhsc.on.ca/resptherapy/st udents/patho/brnchit5.htm Chronical bronchitis Bronchiolitis Chronical bronchitidy (cystic fibrosis, diseased people): – Pseudomonas aeruginosa, Burkholderia cepacia, Staphylococcus aureus Bronchiolitis attacts small babies and seniors. Causative agents are mostly viruses (Pneumovirus/respiratory syncytial virus, Metapneumovirus), sometimes hospitalisation is needed. Targeted treatment is not possible. Whooping cough is an exceptional case. Here antibiotics are always needed. Bronchitis and bronchiolitis – examination and treatment The basis is clinical examination and eventually Xrays, showing development of cough without finding on lung tissue Laboratory examination is almost useless. When sputum is expectorated, it is possible to send it to the laboratory, as in such case a secondary bacterial infection is likely. Here, CRP may be also examined. It is also possible to perform serological examination (mycoplasmas, chlamydia) Antibiotic treatment is almost useless, in mycoplasms and chlamydia macrolids or tetracyclins are used Particular situation: accute exacerbation of chronical bronchitis (EACB) Characterized by – Worsening ot the cough – Elevated expectoration and change of character of sputum and its colour – Often also worsened breathing Less than 40 % of these are caused by viruses Among bacteria, causative agents are H. influenzae, Streptococcus pneumoniae and Moraxella catarrhalis. Routine antibiotic treatment is not recommended, it should be individual Different types of pneumoniae Acute – community-acquired pneumonia (outpatients) in originally healthy (subdivision: adults × children) in disabled persons after a contact with animals Acute – nosocomial pneumonia VAP = ventilator-associated early (before 4. day) late other Subaccute and chronical Pneumonia www.medicinenet.c om/pneumonia/artic le.htm Acute, community-acquired, in healthy persons Streptococcus pneumoniae: the most frequent (almost in seniors > 65 years) Haemophilus influenzae: less common Moraxella catarrhalis: rare Legionella pneumophila: rare Staphylococcus aureus: very rare (influenza epidemic only) In newborns also Streptococcus agalactiae Atypical pneumoniae (small clinical finding, but X-rays show it) In adults almost atypical bacteria (it is not possible to find them in sputum specimen, antibody examination is needed): Mycoplasma pneumoniae Chlamydia pneumoniae In small children respiratory viruses are important (RSV, influenza A, adenoviruses) In newborns also Chlamydia trachomatis, serotypes D–K (perinatal infection) Pneumonia http://www.uspharmacist.com/index.asp?page=c e/105057/default.htm People with diseased immunity Not serious dammage of immunity pneumococci, stafylococci, hemophili Klebsiella pneumoniae (alcohol abusers) Legionella pneumophila Rather serious dammage: Pneumocystis jiroveci (a strange fungus) cytomegalovirus atypic mycobacteria (related to TB) Filamentous bacterium Nocardia asteroides fungi (Aspergillus, Candida) Particular situation: contact with animals Bronchopneumoniae Pasteurella multocida (contact with dogs and cats) Francisella tularensis (tularemia – contact with hares or agricultural stuff contaminated by hares) Atypic pneumoniae Chlamydia psittaci (psitacosis, ornithosis) Coxiella burnetii (Q-fever) Pneumonia http://www.uspharmacist.com/index .asp?page=ce/105057/default.htm Acute, nosocomial: VAP (ventilator) soon (sooner than 4th day): susceptible „normal“ strains of common causative agents (like in community acquired pneumoniae) late: resistant hospital strains (Klebsiella pneumoniae and others) Other Viruses (RS virus, cytomegalovirus) Legionella Nosocomial pneumoniae Subacute and chronic: Aspiration pneumonia and lung abscesses – Anaerobic bacteria (Prevotella melaninogenica, Bacteroides fragilis, peptococci and peptostreptococci) Lung tuberculosis and mycobacterioses Mycobacterium tuberculosis Mycobacterium bovis atypical mycobacteria (e.g. the complex M. avium–M. intracellulare) Bronchopneumonie www.szote.u-szeged.hu/radio/mellk1/amelk4a.htm Lobar a lobular pneumonia www.supplementnews.org/pneumonia Microbiological examination in lung infections Classis community-aquired pneumoniae – blood for blood culture (haemoculture) – sputum – microscopical and basic cultivation examination – sputum – cultivation of Legionella pneumophila – urine – detection of antigen of L. pneumophila Atypic pneumoniae – – – – blood – serological examination (antibodies) Blood and sputum for bacteriology (just for sure) search for viruses (serology, direct examination) sputum – direct detection (ELISA, PCR) Treatment of LRT/lung infections Classical community-acquired pneumoniae: amoxicillin, eventually targeted treatment Atypical pneumoniae: tetracyclins or (especially in children < 8) macrolids. Hospital infections: targeted treatment needed, high risk of resistant strains In TB combination of three of four drugs usually needed „Respiratory viruses“ and non-viral agents tested by virological methods Respiratory viruses are related to many types of respiratory infections, therefore it is useful to know them Virology laboratories examine patients sera labeled „examination of antibodies against respiratory viruses“ – usually, they perform tests for the most common agents Such examinations often include non-viral agents – atypical bacteria that cannot be detected by bacteriological cultivation Respiratory viruses often tested serologically in the lab The most important and most common: – – – – influenzavirus A and B adenoviruses RSV and metapneumovirus parainfluenzaviruses (type 1+3 = Respirovirus, type 2+4 = Rubulavirus) – rhinoviruses – coronaviruses (incl. SARS agent) Less common viral agents – – – – – HSV coxsackieviruses echoviruses EBV Ťahyňa virus Bacterial agents causing atypical pneumonia (but diagnosed in virologic laboratories): Mycoplasma pneumoniae – the most common one Coxiella burnetii – agent of Q-fever Chlamydia (Chlamydophila) psittaci – agent of ornithosis & psittacosis Chlamydia (Chlamydophila) pneumoniae Direct examination for influenza For bacteria it is not recommended to send pharyngeal swabs in LRT infections For influenza it is different: pharyngeal swab is useful here It is necessary to use a swab with a special transport medium for viruses The specimen should be sent to the laboratory as soon as possible Such specimen may be processed by methods of direct diagnostics (virus isolation on cell cultures, especially the modern shell-vial technique) Sputum What to take Sterile container How to také it – A doctor or nurse has to survey it – The patient should wash the mouth – Patient coughs now, trying to get out the secret of lower respiratory ways. – The amount should be at least 1ml. It is possible to keep it < 24 h at refrigerator temperature (but it is better to send it immediately) Transport: < 2 h at room temperature Other specimens from LRT and lungs Trachal aspiration Bronchoalveolar lavage Endotrachal cannula (after extraction) Some of these have special ways of procession in the laboratory, even semiquantitative, enabling to differentiate between a contamination and a true infection Thank you for your attendance Foto: archiv MÚ