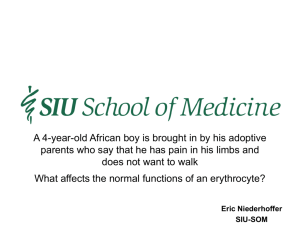
Hemoglobinopathies
advertisement

Hemoglobin 3 Hemoglobinopathies Hemoglobinopathies 1. Hemoglobin functions to transport oxygen from the lungs to respiring tissues. 2. There is an orderly progression during development from fetus to adult of synthesis of several different hemoglobin polypeptide chains. 3. Known hemoglobin mutants arise from point mutations, deletions, insertions, frameshifts and unequal crossing-overs. 4. Hemolytic anemia may result from substitutions altering the heme pocket or the a1b1 interface, or by disruption of alpha helix formation. In these situations the heme iron is more easily oxidized leading to the formation of Heinz bodies. 5. Mutations occurring in the immediate vicinity of heme iron may promote its oxidation (M or methemoglobins). Apart from the mild cyanosis that it produces, no serious consequences follow. 6. Mutations that alter the equilibrium between the high affinity (R) and low affinity (T) conformations of hemoglobin usually favor the R form. Because of high oxygen affinity these hemoglobins release oxygen poorly and polycythemia can result. 7. Hemoglobin S causes the severest clinical consequences (sickle cell anemia) of all the hemoglobinopathies. Peculiar Elongated and Sickle-Shaped Red Blood Corpuscles in a Case of Severe Anemia. James B. Herrick, M.D. This case is reported because of the unusual blood findings, no duplicate of which I have ever seen described. Whether the blood picture represents merely a freakish poikilocytosis or is dependent on some peculiar physical or chemical condition of the blood, or is characteristic of some particular disease, I cannot at present answer. I report some details that may seem non-essential, thinking that if a similar blood condition is found in some other case a comparison of the clinical condition may help in solving the problem. Blood examination The red corpuscles varied much in size, many microcytes being seen and some macrocytes. Polychromatophilia was present. Nucleated reds were numerous, 74 being seen in a count of 200 leukocytes, there being 5,000 to the c.mm. The shape of the reds was very irregular, but what especially attracted attention was the large number of thin, elongated, sickle-shaped and cresecent-shaped forms. These were seen in fresh specimens, no matter in what way the blood was spread on the slide and they were seen also in specimen fixed by heat, by alcohol and ether and stained with the Erlich triacid stain as well as with control stains (Archives of Internal Medicine: 6, 517 (1910)) They were not seen in specimens of blood taken at the same time from other individuals and prepared under exactly similar conditions. They were surely not artefacts, nor were they any form of parasite. In staining reactions they were exactly like their neighbors, the ordinary red corpuscles, though many took on the stain heavily. ……. This is the first reported account of the disease sickle cell anemia. The paper by Herrick is an extremely detailed medical account. We now know that this disease is common among Afro-Americans, West Africans and some white populations in the Mediterranean. Photomicrographs of Blood smears from Herrick’s paper Effect of Hemoglobin Concentration on Oxygen Binding Affinity 6% 20% 33% 7% 1.00 0.80 0.80 0.60 0.60 20% 26% 33% Y Y 1.00 15% 0.40 HbA HbS 0.40 0.20 0.20 0.00 0 20 40 PO2 (torr) 60 80 100 120 0.00 0 20 40 60 PO2 (torr) Adapted from Benesch et al., Anal. Biochem. 89, 162-173 (1978) 80 100 120 Effect of Hemoglobin Concentration on Oxygen Binding 60 50 P 50 HbS 40 HbA 30 20 0 10 20 30 40 Concentration (gm %) Adapted from Benesch et al., Anal. Biochem. 89, 162-173 (1978) Since it was apparent that the disease was partly attributable to the sickle-shaped cells, it seemed likely that some constituent of these cells may be responsible for the abnormal shape of these red cells. Since the main protein in red cells is hemoglobin, therefore, the first definitive test at the molecular level was done by Pauling and his associates. They compared the electrophoretic properties of normal hemoglobin (HbA) and that of sickle-cell hemoglobin (HbS) under native conditions at pH 8.6. Native Gel Electrophoresis at pH 8.6 of Hb’s from Adults 1 2 3 Origin HbS HbA 1. Adult with sickle-cell anemia (homozygous) 2. Adult with sickle-cell trait (heterozygous) 3. Adult with normal blood The electrophoretic experiment by Pauling and his associates indicated that HbS was less negatively charged than HbA. Persons who are homozygous for the HbS gene show only HbS in their blood, whereas those which are heterozygous (sickle cell carriers) have both HbA and HbS present. The molecular basis for the electrophoretic behavior was elucidated by Ingram who separated tryptic peptides by 2D paper electrophoresis and chromatography. This protocol separates the peptides produced by cleavage at the lys and arg residues by both charge and solubility in the aqueous-organic solvent system. The amino acid composition indicates that the a and the b chains have 3 arg and 11 lys residues and, therefore, there should be 15 peptides generated from each class of chain a total of 30 peptides. Thus the job is to digest HbA and HbS with trypsin and then separate the peptides so formed by the 2D technique and compare the two electrochromatograms to determine which peptide has the difference. Two Dimensional “Fingerprinting” of Tryptic Peptides 1 2 3 4 1. Spot the peptide mixture on paper and run vertically to separate by chromatography. Separation by differences in solubility with mobile phase. 2. Yields what looks like a smear. 3. Rotate the paper with smear 90 degrees and subject to electrophoresis. This results in separation due to difference in charges of peptides. 4. Dry paper and stain with ninhydrin dye to detect the peptides revealing ‘fingerprint”. “Fingerprints” of Tryptic Digests of Normal and Sickle Cell Hemoglobin Elute the marked peptide and sequence: val.his.leu.thr.pro.glu.glu.lys HbA Elute the marked peptide and sequence: val.his.leu.thr.pro.val.glu.lys HbS This sequence is from the N-terminal segment of the b chains Why the glu to val change? Codon for glu GAA and GAG Codons for val GUA and GUG also GCU and GUC So a point mutation can bring about the change causing sickle cell anemia. What evolutionary advantage would this change afford to the “victim”? Apparently those with HbS are able to withstand the malarial parasite Plasmodium falciparum better than individuals with just HbA. The consequences of this mutation is that it places a hydrophobic residue in position 6 instead of the negatively charged glutamate. This charged group in the beta chain is exposed to the solvent. Placing a hydrophobic residue on the surface makes it a very unhappy camper. It will try to find someway of avoiding water. It does so by interacting with another deoxy-HbS so that it fits into a hydrophobic cavity and this causes the molecules to aggregate. At high concentrations of HbS these smaller aggregates grow into long multi-stranded fibers. It is the presence of these deoxy-HbS fibers that produce the sickle shape of the blood cells.