AD- the extent of the problem
advertisement

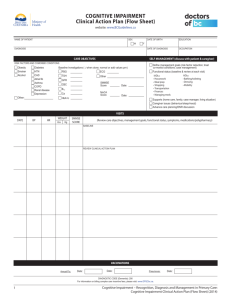
1 AD- the extent of the problem • AD represents over 50% of all dementia cases • AD prevalence doubles every 5 years after 60 years of age • AD affects 15 million people worldwide 2 The diagnosis and assessment of AD • "Listen to the patient, they are telling you the diagnosis." • "It is possible to make a diagnosis of Alzheimer's disease, just as we can make a diagnosis of other major illnesses." • "The challenge today is to obtain an early, accurate and specific diagnosis of dementia using an effective diagnostic process." 3 Mini Mental State Examination score AD prognosis Optimal case 25 ---------------------| Symptoms 20 |----------------------| Diagnosis 15 |-----------------------| Loss of functional independence 10 |--------------------------------| Behavioral problems 5 Nursing home placement |-------------------------------------------| 0 Death |------------------------------------------ 1 2 3 4 5 Years 6 7 8 9 Feidman and Gracon, 1996 4 Definition of the dementia syndrome DEMENTIA • Multiple cognitive deficits – memory loss – aphasia – apraxia – agnosia – disturbance in executive function • These lead to functional decline 5 Causes of dementia Reversible dementias Irreversible dementias • Common causes: – Depression – Delirium – Drug toxicity • Common causes: – Alzheimer's disease – Vascular dementia • Other causes – Lewy body disease – Pick's disease (dementia of the frontal lobe type) – Parkinson's disease with dementia 6 Differentiating AD from other dementias Cognitive impairment Exclude other causes (e.g. delirium and depression, etc) Dementia Exclude other dementias Alzheimer's disease 7 Dementia or delirium Dementia Delirium * Insidious onset with unknown date * Slow, gradual, progressive decline * Generally irreversible * Disorientation late in illness * Slight day-to-day variation OR * Less prominent physiological changes * Consciousness clouded only in late stage * Normal attention span * Disturbed sleepwake cycle; daynight * Psychomotor changes late in illness * Abrupt, precise onset, known date * Acute illness, lasting days or weeks * Usually reversible * Disorientation early in illness * Variable, hour by hour * Prominent physiological changes * Fluctuating levels of consciousness * Short attention span * Disturbed sleepwake cycle; hour-to-hour variation * Marked early psychomotor changes Ham, 1997 8 Dementia or depression Dementia * Insidious onset * No psychiatric history * Conceals disability * Near-miss answers * Mood fluctuation day to day * Stable cognitive loss * Tries hard to perform but is unconcerned by losses * Short-term memory loss * Memory loss occurs first * Associated with a decline in social function Depression * Abrupt onset * History of depression * Highlights disabilities * ’Don't know' answers * Diurnal variation in mood OR * Fluctuating cognitive loss * Tries less hard to perform and gets distressed by losses * Short- and long-term memory loss * Depressed mood coincides with memory loss * Associated with anxiety Ham, 1997, modified from Wells CE, 1979 9 AD risk and protective factors Risk factors Protective factors * Age * Family History of AD (ApoE-4) * Head trauma * Low educational level * Environmental factors * Down’s syndrome * Genetic (ApoE-2) * High educational level * Long-term antiinflammatory drug use, e.g. NSAIDS * Long-term use of estrogens (in women) IPA AD Conference, 1996 10 Making a diagnosis of AD Need for early diagnosis Consistent onset, clinical presentation and disease progression Practical assessment methods New symptomatic treatments Patient and caregiver support IPA AD Conference, 1996 11 Clinical features of AD Functional impairment * IADL * ADL Cognitive decline Insidious onset * Memory loss * Aphasia * Apraxia * Agnosia * Executive function difficulties AD Behavioral signs * Mood swings * Agitation * Wandering Age over 60 years No gait difficulties IPA AD Conference, 1996 12 Clinical features of AD Mild stage of AD (MMSE 2130) Cognition * Recall/learning * Word finding * Problem solving * Judgement * Calculation IMPAIRMENT Function * Work * Money/shopping * Cooking * Housekeeping * Reading * Writing * Hobbies Behavior * Apathy * Withdrawal * Depression * Irritability Adapted from Galasko, 1997 13 Clinical features of AD Moderate stage of AD (MMSE 1020) Cognition IMPAIRMENT Function * Recent memory (remote memory unaffected) * Language (names, paraphasias) * Insight * Orientation * Visuospatial ability * IADL loss * Misplacing objects * Getting lost * Difficulty dressing (sequence and selection) Behavior * Delusions * Depression * Wandering * Insomnia * Agitation * Social skills unaffected Adapted from Galasko, 1997 14 Clinical features of AD Severe stage of AD (MMSE <10) Cognition IMPAIRMENT Function * Attention * Basic ADLs * Difficulty Dressing performing Grooming familiar activities Bathing (apraxis) Eating * Language Continence (phrases, mutism) Walking Motor slowing Behavior * Agitation Verbal Physical * Insomnia Adapted from Galasko, 1997 15 Diagnosing AD in primary care case-finding "How is your memory?" Case-finding Pattie and Gilleard, 1979 16 Diagnosing AD in primary care clinical history, common presentations * Forgetfulness * Getting lost in familiar settings * Difficulties with finance * Deterioration of work or home performance * Inability to recognize, or a lack of interest in, family members * Difficulties driving or using the telephone Clinical History 17 Diagnosing AD in primary care clinical history, questioning Ask the following questions: * How did it start? Was it sudden or gradual? * How long has it been going on? * Is the situation progressing? If so, how rapidly? * Is it step-wise or continuous? * Is it worsening, fluctuating or improving? * What changes have you noticed? * Has there been a change in personality? * Has the patient suffered any delusions or hallucinations? * Does the patient become agitated or wander? Clinical History 18 Diagnosing AD in primary care functional assessment Score Score Maximum Actual Functional Activities Questionnaire (FAQ) 1. Dealing with financial matters, paying bills, writing checks 3 2. Keeping records of taxes, business affairs 3 3. Shopping for everyday necessities: groceries, clothes, etc 3 4. Hobbies or playing games 3 5. Making tea, turning the kettle on and off 3 6. Cooking a balanced meal 3 7. Perception of current events 3 8. Level of attention and understanding: books, television 3 9. Memory: remembering appointments and medications 3 10. Getting about: driving or taking public transport 3 Total 30 Functional Assessment Pfeffer et al 1982 19 Diagnosing AD in primary care cognitive assessments, MMSE Cognitive area Mini Mental State Examination: test outline and scoring Score Score Maximum Actual Orientation *What is the (date, day, month, year, season)? * Where are you (clinic, town, country)? 5 5 Memory *Name three objects. Ask the patient to repeat them Attention *Serial sevens. Alternatively ask the patient to spell world backwards (dlrow) Cognitive Assessment Folstein et al 1975 3 5 20 Diagnosing AD in primary care cognitive assessments, MMSE (continued) Cognitive area Mini Mental State Examination: test outline and scoring Score Score Maximum Actual Recall *Ask for the three objects mentioned above to be repeated 3 Language *Name a pencil and watch *Repeat, 'No ifs, ands or buts’ *A three stage command *Read and obey CLOSE YOUR EYES *Write a sentence *Copy a double pentagon Cognitive Assessment 2 1 3 1 1 1 Total 30 Folstein et al 1975 Diagnosing AD in primary care cognitive assessment The Clock Draw Test Time: 5.00 Score: 7 (normal) Time: .10.30 Score: 3 (demented) Time: 'no real time' Score: 2 (demented) Time: 1/4 past 25 Score: 3 (demented) Cognitive Assessment Thalmann et al 1996. 21 22 Diagnosing AD in primary care physical examination * Life-threatening conditions, e.g. mass lesions, vascular lesions and infections * Blood pressure and pulse * Vision and hearing assessments * Cardiac and respiratory function * Mobility and balance * Sensory and motor system examination (tone, reflexes, gait and coordination) and depressive symptoms (sleep and weight) Physical examination 23 Diagnosing AD in primary care laboratory tests All patients Most patients * Complete blood count * Thyroid function * Vitamin B12 and folate * Syphilis serology * BUN and creatinine * Calcium * Glucose * Electrolytes * Urinalysis * Liver function tests * ECG * Chest X-ray Laboratory tests 24 Diagnosing AD in primary care neuroimaging, computed (axial) tomography (CT) Various CT scan reports in AD * Normal examination for the patient's age * Generalized cerebral atrophy * Small vessel changes, areas of leucoencephalopathy * No signs of subdural hematoma (if head trauma suspected) * Absence of specific areas of cerebral infarctions or evidence of stroke Neuroimaging 25 Primary care management of AD specialist referral * Inconclusive diagnosis * Atypical presentation * Behavioral/psychiatric symptoms * Second opinion * Family dispute * Caregiver support 26 The role of the primary care physician in mild to moderate AD * Define all contributory factors and other illnesses * Discuss the diagnosis, and differentiate other types of dementia * Withdraw non-essential drugs that may interfere with cognition * Treat or manage concomitant illness (e.g. depression, hearing loss) Gauthier, Burns and Pettit, 1997 The role of the primary care physician in mild to moderate AD 27 (continued) * Discuss the use of symptomatic therapies * Monitor functional ability e.g. driving, safety * Referral to specialist if appropriate * Advise on will-making and advance directives * Refer to local AD association for support * Managing caregivers Gauthier, Burns and Pettit, 1997 28 The role of the primary care physician in severe AD * Help caregivers discover and optimize the patient's preserved function * Monitor and treat complications * Facilitate caregiver support (respite and day care programs) * Be aware of caregiver burden and stress * Plan institutionalization, if needed * Assist with end-of-life decisions Gauthier, Burns and Pettit, 1997 Diagnosing AD in primary care 29 A systematic approach summary CASE-FINDING Symptoms YES suggesting cognitive impairment CLINICAL ASSESSMENT *Clinical history *Physical examination *Laboratory tests *Functional assessment *Cognitive assessment Functional decline and cognitive impairment DIFFERENTIAL DIAGNOSIS *Exclude AD diagnosis delirium depression other causes of dementia *Evaluate evidence for AD (neuroimaging) MANAGEMENT OF AD *Follow-up *Patient and caregiver counseling *Management and symptomatic treatment *Specialist referral if indicated 30 Primary care management of AD follow-up * Cognitive ability * Functional ability * Behavior * General health * Routine health checks 31 Caregiver support in primary care * Caring for patients * Self-help * Support services * Medico-legal help * Caregiver well being