Respiration, Breathing Mechanics and Lung Function
advertisement

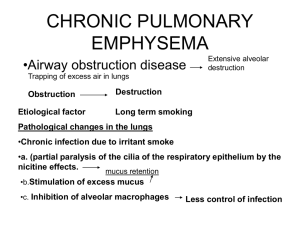
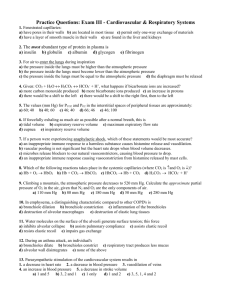
Respiration, Breathing Mechanics and Lung Function Learning Objectives • Know the basic anatomy of the pulmonary airways and circulation, and the pleural space. • Understand the basic autonomic and local control of airways. • Know the mechanics and pressure changes of inspiration and expiration. • Understand pulmonary elastic recoil and compliance. • Understand alveolar surface tension and pulmonary surfactants. • Understand the basic pulmonary volumes and capacitances. • Know what the rate of alveolar ventilation is and how to calculate it. Lung Anatomy Lung Anatomy - Airways Airways • Cartilage rings keep the trachea open. These rings are less extensive in the bronchi and are gone in the bronchioles. • Smooth muscle occupies areas that are not cartilage in the trachea and bronchi. Bronchioles are almost entirely smooth muscle, except the respiratory bronchioles. • Many obstructive diseases of the lungs result from narrowing of the smaller bronchi and larger bronchioles. Airway Resistance • Most of the resistance is in the larger bronchioles and bronchi near the trachea (due to small numbers of these airways). • In disease, the resistance of bronchioles is a bigger concern, because these are easily occluded by muscle contractions in their walls, edema, or mucus collecting. Autonomic Control of Airways • Sympathetic – norepinephrine and epinephrine relax the trachea and bronchi. Direct control of bronchioles by sympathetic fibers is weak. Because of beta-adrenergic receptors, epinephrine has a greater effect. • Parasympathetic - acetylcholine causes mildto-moderate bronchiolar constriction. Local Control • Histamine causes bronchiolar constriction and is released during an allergic reaction. • What do you thing the effects are of the typical vasodilators, such as blood levels of O2 and CO2? What do these substances do in the lungs during exercise? Lung Anatomy - Circulation Note: Pulmonary arteries carry deoxygenated blood and pulmonary veins carry oxygenated blood Pulmonary Vessels • Pulmonary arteries, compared to systemic arteries, are thin, short, and have larger diameters. This gives them a high compliance and can accommodate the stroke volume of the right ventricle. • Pulmonary veins are short and immediately empty their effluent into the left atrium. • Bronchial vessels supply the blood needed to maintain the lungs (oxygenated) and originate from the systemic circulation. It empties into the pulmonary veins. Pulmonary Blood Pressure • As you might expect from short, highly compliant vessels, the pressures in the pulmonary system are low, compared to the pressures in the systemic vasculature. Pleural Sacs • The intrapleural fluid normally consists of a very thin layer. • The pleural pressure is slightly negative. Thus, the lungs are held to the thoracic cavity, but in a fluid so that they can slide freely as the chest expands and contracts. • Imagine the water between glass microscope slides. The glass slides are lubricated, but hart to pull apart. Contraction and Expansion of the Thoracic Cage Lungs are contracted or expanded in 2 ways: 1. Downward and upward movement of diaphragm (major force during normal, quiet breathing. 2. Elevation and depression of the ribs, using abdominal and rib cage (intercostal) muscles. Contraction and Expansion of the Thoracic Cage Expiration – Diaphragm relaxes and moves up. Rib cage is pulled downward and the chest wall and abdominal structures compress the lungs. Inspiration – Diaphragm contracts and moves down. Rib cage is pulled upward and expanded. Pressures Causing Ventilation • As with blood, air moves by bulk flow from high pressure to low pressure. What equation? • Two pressures important in ventilation are: - Alveolar pressure – the pressure difference between the inside of the alveoli and the atm (atm P is the zero reference). -Transpulmonary pressure – the pressure difference between the inside of the alveoli and the pleural pressure. • Air flows into the alveoli when the atm pressure is greater than the alveolar pressure. Changes pressure are achieved by changing the volume. Pleural Pressure Changes • During inspiration, expansion of the chest decreases the pleural pressure (by decreasing the volume). • This changes the transpulmonary pressure (alveolar pressure – pleural pressure). • The alveolar pressure then decreases below atm pressure and air flows into the lungs (images on next slide). Pressure Changes During Normal Breathing Elastic Recoil • Elastic recoil is the tendency of an elastic structure to oppose stretching. • The lungs naturally have a tendency to collapse because of elastic recoil. They are held open by the negative pleural pressure (established by lymphatic pumping of fluid). • The chest wall naturally expands, but is also held by the negative pleural pressure. Punctured Lung • What would happen if the visceral pleura was punctured, but the lung was not damaged? • Air would rush into the intrapleural space and the lung would collapse – a pneumothorax. Lung Compliance • Compliance is the magnitude of the change in volume produced by a given change in pressure. • The greater the lung compliance, the easier it is to expand the lung at any given change in transpulmonary pressure. Lung Compliance Diagram Note the elasticity of the air-filled lung. Elastic Forces of the Lungs • Characteristics of the compliance diagrams are determined by 2 elastic forces: - Elastic properties of the lung tissue itself (fairly straightforward). - Elastic forces caused by the surface tension of the fluid that lines the inside walls of the alveoli. • Looking at Fig 37-4, one can see that surface tension forces in the alveoli represent ~ 2/3 of the elastic forces tending to cause the lung to collapse. Surface Tension • H2O molecules at the interface with air are attracted to each other. This causes the H2O at the surface to contract (collapsing the alveoli). • The pressure caused by surface tension can be calculated from Surfactants • Surfactants in water decrease the surface tension and are secreted by type II alveolar epithelial cells. • The body’s surfactant is a complex mixture of phospholipids, proteins, and ions. • Surfactant is partially dissolved in the water, whereas the rest spreads over the water surface. • Surfactants can decrease the surface tension by up to 10-fold. Surfactants in Neonates • Premature babies often have alveoli with diameters less than ¼ that of an adult (note effect of pressure equation). • Moreover, surfactant is not secreted into the alveoli until between the 6th and 7th month of gestation. • Thus, the lungs of premature babies are more likely to collapse. • The condition respiratory distress syndrome of the newborn is a concern in premature babies. Pulmonary Volumes • Tidal Volume – normal volume of air expired or inspired each normal breath. • Inspiratory Reserve – the extra volume aboe the tidal volume. • Expiratory Reserve – The maximum volume of air that can be expired. • Residual Volume – The volume of air remaining in the lungs after maximum expiration. Pulmonary Capacities • Inspiratory capacity is the tidal volume + the inspiratory reserve. • Functional residual capacity is the expiratory reserve + residual volume. • Vital capacity is the inspiratory reserve + tidal volume + expiratory reserve. • Total lung capacity is the vital capacity + residual volume. Minute Respiratory Volume • This is the total amount of new air moved into the respiratory passages each minute. • It equals the tidal volume x respiratory rate/min. • Normally, this is ~ 500 ml x 12 breaths/min ~ 6L/min. Alveolar Ventilation • The key area to bring new air in is to the alveoli, where gas exchange occurs with the pulmonary blood. • Air that does not reach the gas exchange areas is called “dead space air”. • The normal amount of dead space air in a young adult male ~ 150 ml. Alveolar Ventilation • Alveolar ventilation per minute is determined as follows: • Where, VA = vol of alveolar ventilation/min Freq = rate of respiration/min VT = Tidal vol VO = dead space vol