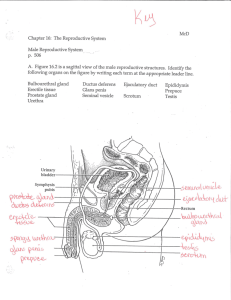
Male Reproductive System
advertisement

Similarities / Differences Develop very similar structures of sex glands Two genital tubes Both sexes have reproductive organs called GENITALS or GENITALIA, designed for the purpose of intercourse and conception. Only the female has organs for pregnancy and childbirth. 4 Essential Stages of Female Reproduction The female body goes through 4 essential stages: Puberty- age 8-13; develop breasts, hormones, pubic hair; menstruation begins Reproduction – Puberty till age 45; pregnancy can happen Perimenopause – age 40-60 (last 2 years or so); time right before menopause where body is getting low on hormone production, irregular periods, hot flashes, night sweats, mood swings, dry vagina and other side effects can occur Menopause – average age 45 or when full hysterectomy is performed; menstruation ends; pregnancy cannot occur; body stops producing estrogen. Ovulation The egg travels through the fallopian tube. The egg takes approximately 2 weeks to travel from the ovary to the uterus. In a woman (with a fairly regular menstrual cycle), ovulation occurs in approximately 14-15 days before her next menstrual period is due. Some women do not have a regular cycle due to various changes in their lives, including emotional stress, drug use, diet etc. If you have an irregular cycle, ovulation will also be irregular and unpredictable. Ovulation is the time that a woman is most likely to get pregnant. You can get pregnant if you have sex during or near the time of ovulation. Fertilization • During sex, sperm are released into the vagina. They travel up through the cervix, through the uterus, and out up to the tubes. • Around the time of ovulation, there is thin mucus in the cervix that helps the sperm move. • If a sperm meets an egg in the tube, fertilization (the joining of egg and sperm) can occur. The fertilized egg then moves through the tube into the uterus and becomes attached there to grow into a fetus. External Female Anatomy Vulva: woman’s external genital area. Labia Majora: (large lips) two folds of skin running from the mons pubis to below the vaginal opening Labia Minora: two smaller folds of tissue which lie just within the labia majora. Clitoris: a small, pea-shaped bump at the front of the labia that contains erectile tissue (counter part to male penis.) Urethra: below the clitoris, the opening to the bladder. Internal Organs Vagina: passageway between the uterus and the outside of a woman’s body. Cervix: Opening from the uterus to the vagina. Uterus: Triangular shaped organ just above pubic bone that is place where the baby grows in a woman’s abdomen. Oviducts (Fallopian Tubes): two tubular structures leading from the ovaries to the uterus Ovaries: organs holding a woman’s eggs. Other related concerns Endometriosis: fragments of the endometrium in abnormal places. These fragments may be found on the outside of the uterus, in the abdominal cavity, and may be attached to the intestines. Dysmenorrhea: painful menstruation Hysterectomy: surgical removal of the uterus, cervix, fallopian tubes and possibly one or both ovaries. Tubal Ligation: an operation for sterilization of women where they cut or tie off the fallopian tubes so that ova cannot be fertilized. PMS: premenstrual syndrome. Symptoms may include moodiness, cramping, nausea and body aches a few days before menstruation is to begin. Menstrual Cycle: the process of passing the blood and tissue lining of the uterus from the body. Toxic Shock Syndrome: caused by bacteria that live in the vagina, which then multiply and cause infection. Tampons left in the vagina for too long have been known to cause this condition. Menopause: the remaining ova no longer ripen or develop. Estrogen: the hormone responsible for secondary sex characteristics and for the sex drive in females. The “egg producing” hormone. Progesterone: Sustains pregnancy. Secreted by the corpus luteum and causes the following changes: Uterine lining thickens (endometrial cells grow and store nutrients to offer an appropriate condition for implantation of fertilized egg) Cervical secretions thicken to keep bacteria and other sperm out Cervix firms, lowers and closes Resting body temperature is higher Timelines Male Time Line: Infancy Erections begin Female Time Line: Ages 11-14 Secondary sex characteristics appear Ages 9-12 Secondary sex characteristics appear Ages 13-16 Sperm produced in adult amounts (puberty) Ages 11-14 Menstrual cycle begins Late teens Peak sexual urges for boys Late 20-30’s Peak sexual urges Throughout life If good health is present, there is the sex urge and ability to father children. Ages 45-55 menopause (cycle stops, but sex urge continues) Female Reproductive System Male Reproductive System Sexual Health: Your Guide to the Male Reproductive System The purpose of the organs of the male reproductive system is to perform the following functions: To produce, maintain and transport sperm (the male reproductive cells) and protective fluid (semen) To discharge sperm during sex To Produce and secrete male hormones responsible for maintaining the male reproductive system. Male Reproductive Structure Unlike the female reproductive system, most of the male reproductive system is located outside of the body. These external structures include the penis, scrotum, and testicles. The placement of the male reproductive organs on the outside of the body is necessary for temperature control of sperm which need to be kept cooler than normal body temperature. Penis This is the male organ used in sexual intercourse. The head of the penis is covered with a loose layer of skin called foreskin. (This skin is sometimes removed in a procedure called circumcision when a boy is first born.) The opening of the urethra, the tube that transports semen and urine, is at the tip of the penis. The penis also contains a number of sensitive nerve endings. The body of the penis is cylindrical in shape and consists of 3 circular shaped chambers. These chambers are made up of special, sponge-like tissue. This tissue contains thousands of large spaces that fill with blood when the man is sexually aroused. As the penis fills with blood, it becomes rigid and erect, which allows for penetration during sexual intercourse. The skin of the penis is loose and elastic to accommodate changes in penis size during an erection. Semen, which contains sperm (reproductive cells), is expelled (ejaculated) through the end of the penis when the man reaches sexual climax (orgasm). When the penis is erect, the flow of urine is blocked from the urethra, allowing only semen to be ejaculated at orgasm. Scrotum This is the loose pouch-like sac of skin that hangs behind the penis. It contains the testicles (also called testes), as well as many nerves and blood vessels. The scrotum acts as a "climate control system" for the testes. For normal sperm development, the testes must be at a temperature slightly cooler than body temperature. Special muscles in the wall of the scrotum allow it to contract and relax, moving the testicles closer to the body for warmth or farther away from the body to cool the temperature. Testicles (testes) These are oval organs about the size of large olives that lie in the scrotum, secured at either end by a structure called the spermatic cord. Most men have two testes. The testes are responsible for making testosterone, the primary male sex hormone, and for generating sperm. Within the testes are coiled masses of tubes called seminiferous tubules. These tubes are responsible for producing sperm cells. The internal organs of the male reproductive system, also called accessory organs, include the following: Epididymis The epididymis is a long, coiled tube that rests on the backside of each testicle. It transports and stores sperm cells that are produced in the testes. It also is the job of the epididymis to bring the sperm to maturity, since the sperm that emerge from the testes are immature and incapable of fertilization. During sexual arousal, contractions force the sperm into the vas deferens. Vas deferens The vas deferens is a long, muscular tube that travels from the epididymis into the pelvic cavity, to just behind the bladder. The vas deferens transports mature sperm to the urethra, the tube that carries urine or sperm to outside of the body, in preparation for ejaculation. Vasectomy During a vasectomy, the vas deferens from each testicle is clamped, cut, or otherwise sealed. This prevents sperm from mixing with the semen that is ejaculated from the penis. An egg cannot be fertilized when there are no sperm in the semen. The testicles continue to produce sperm, but the sperm are reabsorbed by the body. (This also happens to sperm that are not ejaculated after a while, regardless of whether you have had a vasectomy.) Because the tubes are blocked before the seminal vesicles and prostate, you still ejaculate about the same amount of fluid. It usually takes several months after a vasectomy for all remaining sperm to be ejaculated or reabsorbed. You must use another method of birth control until you have a semen sample tested and it shows a zero sperm count. Otherwise, you can still get your partner pregnant. Urethra The urethra is the tube that carries urine from the bladder to outside of the body. In males, it has the additional function of ejaculating semen when the man reaches orgasm. When the penis is erect during sex, the flow of urine is blocked from the urethra, allowing only semen to be ejaculated at orgasm. Seminal Vesicles The seminal vesicles are sac-like pouches that attach to the vas deferens near the base of the bladder. The seminal vesicles produce a sugar-rich fluid (fructose) that provides sperm with a source of energy to help them move. The fluid of the seminal vesicles makes up most of the volume of a man's ejaculatory fluid, or ejaculate. Prostate Gland The prostate gland is a walnut-sized structure that is located below the urinary bladder in front of the rectum. The prostate gland contributes additional fluid to the ejaculate. Prostate fluids also help to nourish the sperm. The urethra, which carries the ejaculate to be expelled during orgasm, runs through the center of the prostate gland. Bulbourethral glands: Also called Cowper's glands These are pea-sized structures located on the sides of the urethra just below the prostate gland. These glands produce a clear, slippery fluid that empties directly into the urethra. This fluid serves to lubricate the urethra and to neutralize any acidity that may be present due to residual drops of urine in the urethra.