Sperm cell
advertisement

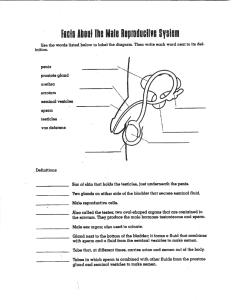
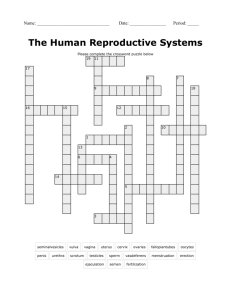
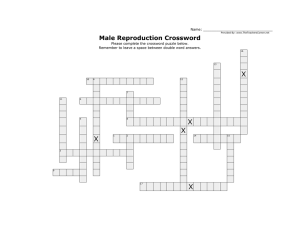
Seminal Vesicles + The pair of seminal vesicles are posterior to the urinary bladder. + Contribute about 65-75% of the seminal fluid in humans + Contain proteins, enzymes, fructose, mucus, vitamin C, flavins, phosphorylcholine and prostaglandins (involved in suppressing an immune response by the female against the foreign semen) + High fructose concentrations provide nutrient energy for the spermatozoa as they travel through the female reproductive system. + To produce, maintain and transport sperm (the male reproductive cells) and protective fluid (semen) + To discharge sperm within the female reproductive tract + To produce and secrete male sex hormones The entire male reproductive system is dependent on hormones - chemicals that stimulate or regulate the activity of cells or organs + Follicle Stimulating Hormone (FSH)- necessary for sperm production. + Luteinizing Hormone (LH) – stimulates the production of testosterone. + Testosterone- also important in the development of male characteristics ( muscle mass and strength, fat distribution, bone mass and sex drive). + Penis + Scrotum PENIS + This is the male organ used in sexual intercourse. + + + three parts: -Root- attaches to the wall of the abdomen -Shaft- the body -Glans - cone-shaped part at the end of the penis. Foreskin- loose layer of skin that covers the glans. This skin is sometimes removed in a process called circumcision. The opening of the urethra, is at the tip of the penis. The body of the penis is cylindrical in shape and consists of three circular shaped chambers. This tissue contains thousands of large spaces that fill with blood when the man is sexually aroused. + Semen- the fluid which carries sperm during ejaculation.. SCROTUM This is the loose and pouch-like sac of skin which hangs posterior to the penis. Inside the scrotum are the testicles, also called testes. -to serve as climate control system for the testes When extreme cold temperature is detected, the scrotum contract which draws the testes closer to the body. When a hot temperature is detected in the body, the scrotum relaxes to keep the testes away from the body. + Epididymis + Vas deferens + Testes This is the long, coiled tube-like structure which is located on the posterior of each testicle. -to transport and store sperm cells which are produced inside the testes. -to nurture the sperm until it matures. During the arousal stage of sexual activity, the contractions of the genitals force the sperm which are contained in the fluid-like semen into the vas deferens. A muscular tube that begins at the lower end of the Epididymis and passes upward along the side of the testis to become part of the spermatic cord. It passes through the inguinal canal, enters the abdominal cavity, and courses over the pelvic brim. From there, it extends back into the pelvic cavity, where it ends behind the urinary bladder. Near its termination, it becomes dilated into a portion called the "ampulla." Just outside the prostate gland, the tube becomes slender again and unites with the duct of a seminal vesicle. Ejaculatory duct, the fusion of prostate gland and the duct of seminal vesicle. These are the oval-shaped organs found inside the scrotum. They are secured at either end by what is termed as the spermatic cord. -to produce testosterone. -to produce sperm cells. Seminiferous tubules- tubes masses which are coiled together. These tubules function by spermatogenesis. SEMINAL VESICLE + Prostate Gland + The prostate gland is a muscular gland that surrounds the first inch of the urethra as it emerges from the bladder. + The smooth muscle of the prostate gland contracts during ejaculation to contribute to the expulsion of semen from the urethra. + Stores and secretes a clear, slightly alkaline fluid constituting up to one-third of the volume of semen. PROSTATE GLAND Bulbourethral Glands + The bulbourethral glands also called Cowper's glands are located below the prostate gland and empty into the urethra. + The alkalinity of seminal fluid helps neutralize the acidic vaginal pH + For secretion of gelatinous seminal fluid that helps lubricate the urethra for spermatozoa to pass through, and to help flush out any residual urine or foreign matter. (< 1% of semen) + It is serve to increase the mobility of sperm cells in the vagina and cervix by creating a less viscous channel for the sperm cells to swim through, and preventing their diffusion out of the semen. + The components of semen come from two sources: sperm, and "seminal plasma". + Seminal plasma is produced by contributions from the seminal vesicle, prostate, and bulbourethral glands. + Basic amines such as putrescine, spermine, spermidine and cadaverine are responsible for the smell and flavor of semen. + These alkaline bases counteract the acidic environment of the vaginal canal, and protect DNA inside the sperm from acidic denaturation. + A spermatozoa are the haploid cell that is the male gamete. + Contribute half of the chromosome number of an individual + The sperm is the main reproductive cell in males. + The sperms differ in that each carry a set of chromosomes dividing each into either a male, or female sperm. + The female sperm also differ phenotypically in that they have a larger head in comparison to the male sperms. This contributes to the male sperm being lighter, and therefore faster and stronger swimmers than their female counterparts although statistically there is still a 50% chance of an either XY or XX embryo forming. Tail flagellates - which propels the sperm cell by rotating like a propeller, in a circular motion Mitochondria in midpiece – for ATP generation Nucleus – carries the genetic material Acrosome – releases enzyme to weaken the thick shell formed by glycoproteins (zona pellucida) Capacitation – process in which sperm develop the capability to fertilize Hypermotility - change in beat frequency and amplitude of sperm motility Acrosome Reaction - lysosomal enzymes contained within the acrosome are released, causing alteration of the sperm head plasma membrane and weaken the shell, allowing the sperm cell to penetrate it and reach the plasma membrane of the egg. 1. Adequate motility to traverse the female genital tract. 2. Ability to recognize and bind to the ovum and its investments. 3. Ability to penetrate the zona pellucida. 4. Ability to fuse with the plasma membrane of the ovum. + The most important laboratory test in evaluating + + + + the fertility potential in a man is the semen analysis. ]The following are the normal parameters. Volume 2-5 cc Sperm density >20 million/cc (avg. 50-60) Motility >60% Morphology Absence of WBC's, RBC's, bacteria, agglutination >60% normal forms + Azoospermia is the condition in which no sperm are found in the ejaculate. Cause of Azoospermia – ductal obstruction – impaired production of mature sperm Tests to know the cause of Azoospermia – The volume of semen may help identify the level of obstruction, since small volumes, indicate obstruction of the ejaculatory ducts. – Testis biopsy will reveal the adequacy of sperm production and the degree of sperm maturation. • Gonadotropin-Releasing Hormone • Luteinizing Hormone • Follicle Stimulating Hormone • Testosterone + Secreted by the hypothalamus to the pituitary + Released in pulses in average of 70-90 minutes and have a half-life of 2-5 minutes + Variation in the pulse frequency regulates the release of FSH and LH + Secreted by the pituitary gland in response to GnRH + Stimulates the Leydig cells to produce testosterone + Secreted by the pituitary gland + Stimulates the Sertoli cells to produce mature sperm with the help of testosterone + Stimulates the protein synthesis in Sertoli cells by stimulating cAMP and protein kinases + Inhibited by inhibin produced by the Sertoli cells + Important in sperm production + Male hormone and androgen produced by the Leydig cells + Masculinization of internal and external reproductive tissues + + + + + + – Promotes the growth of the penis and scrotum Pubertal changes Enables retraction of foreskin during puberty Binds with the andogen-binding protein produced by the Sertoli cells Testosterone aromatase Estradiol (E2) Testosterone 5 α reductase Dihydrotestosterone (DHT) Inhibits the production of LH and GnRH - Stimulated by the androgens 1. Motivation – mainly olfactory inputs; motivation to mate -Androgen binds to amygdala 2. Performance – mainly visual inputs; mating performance -Androgen binds to preoptic area *Castration reduces motivation and performance Male Reproductive System + Penile erection - a physiological phenomenon where the penis becomes enlarged and firm - complex interaction of psychological, neural, vascular and endocrine factors, and is usually, though not exclusively, associated with sexual arousal How an erection happens + Touch, sights, sounds, erotic memories and fantasies cause sexual excitement. + These stimuli increase signal output from a part of the brain called the paraventricular nucleus. These signals then pass through special autonomic nerves in the spinal cord, the pelvic nerves and the cavernous nerves that run along the prostate gland to reach the corpora cavernosa and the arteries that supply them with blood. + + In response to these signals, the muscle fibres in the corpora relax, allowing blood to fill the spaces between them. + Muscle fibres in the arteries that supply the penis also relax, and there is an eightfold increase in blood flow to the penis. The increased blood flow expands the corpora, then stretches the surrounding sheath (the tunica). + As the tunica stretches, it blocks off the veins that take blood away from the corpora cavernosa. This traps blood within the penis, the pressure becomes very high and the penis becomes erect. + During an erection pressure in the penis is at least twice the pressure of blood in the main circulation. This is possible because the muscles of the pelvic floor contract around the base of the corpora cavernosa. Cross-section of the penis showing the position of the corpora cavernosa. + changes in the blood vessels that lessen their ability to deliver blood to the penis + problems with the nervous system that interferes with the nerves that stimulate an erection + problems due to certain drugs such as SSRI antidepressants, antihypertensives (blood pressure pills), anticholinergics, corticosteroids and others + hormone problems such as too much prolactin (a pituitary hormone) or low testosterone + Viagra, Cialis or Levitra act to maintain a high concentration of cGMP – should not be taken with food and alcohol + 60% successful, work only if sexually excited + not successful with low testorone (nitric oxide (NO) and cGMP) + testosterone replacement + Nocturnal erections - rapid eye movement phase - 7 times and 25% of sleep in young men - erection is 70% of the normal (during sexual arousal) + Morning erection - not related to bladder fullness - loss of morning erection may indicate low in testosterone + sufficient level of stimulation = ejaculation + sympathetic nervous system – responsible for semen production + semen ejected to urethra with rhythmic contraction (10-15 contractions) + ejaculation cannot be stopped when contraction started + contraction = 0.6 seconds interval with increment of 0.1 seconds per contraction + immediately following an orgasm, during which time they are unable to achieve another erection, and a longer period again before they are capable of achieving another ejaculation + during this time a male feels a deep and often pleasurable sense of relaxation, usually felt in the groin and thighs + semen = 0.1 – 10 milliliters + adult semen volume is affected by the time that has passed since the previous ejaculation + Hypospermia = low semen volume that may be caused by ejaculatory duct obstruction + last ejaculation + stress levels + testosterone + Oligospermia – unusually low sperm count + Azoozpermia – absence of sperm from the semen + first ejaculation = 12 months from the onset of + + + + puberty (through nuctornal emission or masturbation) 1mL of semen for the following 3 months semen is typically clear = fail to liquify semen liquifies – 12 -14 months after 1st ejaculation = 90% no sperm Semen development during puberty Time after first ejaculation (months) Average volume (milliliter) Liquefaction Average sperm concentration (million sperm/milliliter) 0 0.5 Noa 0 6 1.0 Noa 20 12 2.5 No/Yesb 50 18 3.0 Yesc 70 24 3.5 Yesc 300 ^a Ejaculate is jellylike and fails to liquify. ^b Most samples liquify. Some remain jellylike. ^c Ejaculate liquifies within an hour. a mild injury to the testicles can cause severe pain, bruising, or swelling occur when the testicles are struck, hit, kicked, or crushed, usually during sports or due to other trauma testicular torsion-- when 1 of the testicles twists around, cutting off the blood supply surgery is needed to untwist the cord and save the testicle a varicose vein (an abnormally swollen vein) in the network of veins that run from the testicles usually not harmful, although in some people it may damage the testicle or decrease sperm production see his doctor if he is concerned about changes in his testicles one of the most common cancers in men younger than 40 occurs when cells in the testicle divide abnormally and form a tumor if it's detected early, the cure rate is excellent teen boys should be encouraged to learn to perform testicular self-examinations inflammation of the epididymis, the coiled tubes that connect the testes with the vas deferens caused by an infection and results in pain and swelling next to one of the testicles occurs when fluid collects in the membranes surrounding the testes may cause swelling of the testicle but are generally painless surgery may be needed to correct the condition when a portion of the intestines pushes through an abnormal opening or weakening of the abdominal wall and into the groin or scrotum may look like a bulge or swelling in the groin area can be corrected with surgery a persistent, often painful erection lasting more than four hours occurs when blood flows into the penis but is not adequately drained treatment involves draining the blood using a needle placed in the side of the penis Medications that help shrink blood vessels, which decreases blood flow to the penis, also may be used. surgery may be required to avoid permanent damage to the penis bending of the penis during an erection due to a hard lump called a plaque plaque often begins as a localized area of irritation and swelling (inflammation), and can develop into a hardened scar penile implant can be used in cases where Peyronie's disease has affected the man's ability to achieve or maintain an erection. non-surgical treatment for Peyronie's disease involves injecting medication directly into the plaque in an attempt to soften the affected tissue, decrease the pain, and correct the curvature of the penis. Vitamin E pills have also been shown to benefit some men with Peyronie's disease. inflammation of the skin covering the head of the penis most often in men and boys who have not been circumcised Symptoms include redness or swelling, itching, rash, pain, and a foul-smelling discharge If there is an infection, treatment will include an appropriate antibiotic or antifungal medication. In cases of severe or persistent inflammation, a circumcision may be recommended. taking appropriate hygiene measures avoid strong soaps or chemicals, especially those known to cause a skin reaction. a rare form of cancer, highly curable when caught early occurs when abnormal cells in the penis divide and grow uncontrolled. Certain benign (noncancerous) tumors may progress and become cancer. Surgery to remove the cancer is the most common treatment. condition in which the foreskin of the penis is so tight that it cannot be pulled back (retracted) to reveal the head of the penis treatment may include gentle, manual stretching of the foreskin over a period of time Circumcision- the surgical removal of the foreskin, often is used to treat phimosis occurs when the foreskin, once retracted, cannot return to its original location Treatment of focuses on reducing the swelling of the glans and foreskin. Applying ice may help reduce swelling, as may applying pressure to the glans to force out blood and fluid an injection of medication to help drain the penis may be necessary a surgeon may make small cuts in the foreskin to release it circumcision- may be used as a treatment for paraphimosis + Include human immunodeficiency virus/acquired immunodeficiency syndrome (HIV/AIDS), human papillomavirus (HPV, or genital warts), syphilis, chlamydia, gonorrhea, genital herpes, and hepatitis B + spread from one person to another mainly through sexual intercourse HYPOSPADIAS - a disorder in which the urethra opens on the underside of the penis, not at the tip AMBIGUOUS GENITALIA - occurs when a child is born with genitals that aren't clearly male or female. In most boys born with this disorder, the penis may be very small or nonexistent, but testicular tissue is present. In a small number of cases, the child may have both testicular and ovarian tissue. MICRO PENIS- a disorder in which the penis, although normally formed, is well below the average size, as determined by standard measurements