Don't Let It Get You Down! Managing - AAP Point-of
advertisement
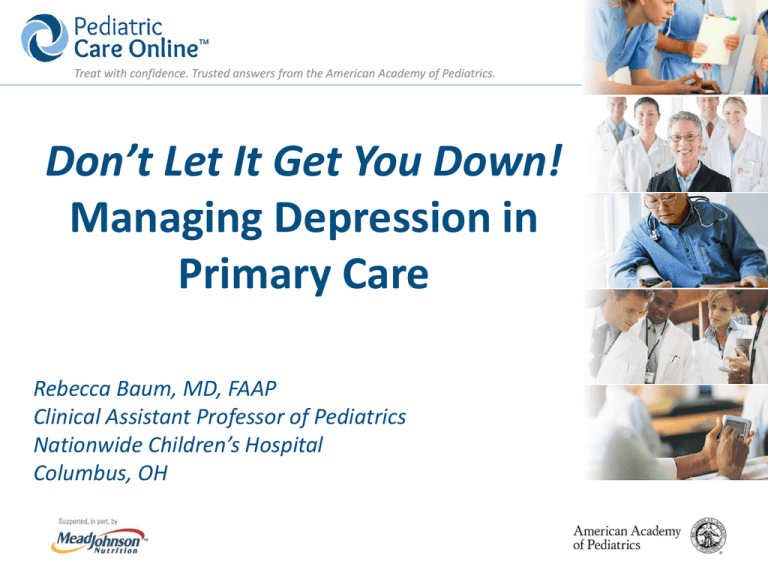
Treat with confidence. Trusted answers from the American Academy of Pediatrics. Don’t Let It Get You Down! Managing Depression in Primary Care Rebecca Baum, MD, FAAP Clinical Assistant Professor of Pediatrics Nationwide Children’s Hospital Columbus, OH Treat with confidence. Trusted answers from the American Academy of Pediatrics. Disclaimer Statements and opinions expressed are those of the author and not necessarily those of the American Academy of Pediatrics. Mead Johnson sponsors programs such as this to give healthcare professionals access to scientific and educational information provided by experts. The presenter has complete and independent control over the planning and content of the presentation, and is not receiving any compensation from Mead Johnson for this presentation. The presenter’s comments and opinions are not necessarily those of Mead Johnson. In the event that the presentation contains statements about uses of drugs that are not within the drugs' approved indications, Mead Johnson does not promote the use of any drug for indications outside the FDAapproved product label. Treat with confidence. Trusted answers from the American Academy of Pediatrics. Objectives Understand the presentation of depression and low mood in pediatrics. Implement first-line strategies to manage depression and low mood in primary care. Identify key system components necessary for managing depression and low mood in the primary care setting. Treat with confidence. Trusted answers from the American Academy of Pediatrics. Well Child Care Visit Sarah is a 13-year-old who presents with her mother for a well child care visit. As you ask about school and friends, Sarah’s mother mentions that her grades have dropped and that she is spending more time in her room. Sarah keeps her head down and shrugs her shoulders when you ask her questions. With the visit about to wrap up, you ask Sarah and her mother if there is anything wrong. Sarah looks down and her mother says, “I don’t know…aren’t all teenagers like this?” Treat with confidence. Trusted answers from the American Academy of Pediatrics. What happened? What should we do next? How could things go differently? Treat with confidence. Trusted answers from the American Academy of Pediatrics. Well Child Care Visit Sarah is a 13-year-old who presents with her mother for a well child care visit. Like all teens in your practice, Sarah completes the Patient Health Questionnaire-9 (PHQ-9) Modified for Teens depression screener at the start of the visit. The results are available to you as you begin your visit. Patient Health Questionnaire-9 for Teens Sarah’s PHQ-9 score is 9 Treat with confidence. Trusted answers from the American Academy of Pediatrics. Defining Features Low, sad mood or irritability o Loss of interest o Thoughts about dying o Pessimism or hopelessness Changes in thoughts about oneself o Loss of self confidence o Guilt or low-self worth, over-focus on past errors Treat with confidence. Trusted answers from the American Academy of Pediatrics. Defining Features Somatic changes o o o o Disturbed sleep Disturbed appetite Fatigue or loss of energy Agitation or slowing of movement or speech Cognitive changes o Trouble with memory/concentration Treat with confidence. Trusted answers from the American Academy of Pediatrics. Related Questions How long have you been feeling like this? Other stressors? Supports? Appetite and sleep? Drugs and alcohol? Thoughts of self-harm or harm to others? Treat with confidence. Trusted answers from the American Academy of Pediatrics. Asking About Self-Harm Have you ever felt so sad that you didn’t want to be here anymore? Or wanted to die? Have you ever had a plan to hurt yourself? Have you ever hurt yourself? Are you thinking of hurting yourself now? Risk Factors Access to lethal means Substance use Family history Recent trauma or stress Treat with confidence. Trusted answers from the American Academy of Pediatrics. Assess Level of Risk and Respond Accordingly • Implement pre-determined office plan for mental health emergencies. • Review safety planning. • Assist with linkage to services. • Provide resources. • Make a plan to follow up with the family. Treat with confidence. Trusted answers from the American Academy of Pediatrics. “Making the Diagnosis” Major depressive disorder o ≥5 symptoms present for ≥2 weeks (≥1 symptoms being low mood or decreased pleasure) o Screeners can help clarify diagnosis Presentations in primary care are more likely to be subclinical and/or shorter in duration. Treat with confidence. Trusted answers from the American Academy of Pediatrics. Challenges to Diagnosis Stigma Over generalizations o “Aren’t all teenagers like this?” o “I’m not crazy…just a little stressed” o “I’m sure it will pass…we don’t need any help” Varied presentations Treat with confidence. Trusted answers from the American Academy of Pediatrics. Sharing Your Impressions Make a clear transition from information gathering to summing up. o Ask the family what they think the symptoms might mean. o Briefly outline your reasoning and ask if you’ve gotten it right. o When possible, present your conclusions as a range of possibilities. Treat with confidence. Trusted answers from the American Academy of Pediatrics. Giving Advice Be thoughtful. o Ask for “permission.” o Ask for their ideas. Offer your advice as a set of choices. o Include their ideas. o Think about short- and long-term plans. Treat with confidence. Trusted answers from the American Academy of Pediatrics. FIRST-LINE STRATEGIES TO TRY IN PRIMARY CARE Treat with confidence. Trusted answers from the American Academy of Pediatrics. Psychoeducation Depression is a common and treatable problem. Depression often runs in families, probably for many reasons. It is normal to feel “down” but when these feelings get in the way of life, there are ways to try to feel better. Physical symptoms can be linked with mood—they are not “made up.” Treat with confidence. Trusted answers from the American Academy of Pediatrics. Cognitive/Coping Skills Recognizing ANTS o Automatic Negative Thoughts that become habit and lead to negative thinking Using positive “self talk” to change thinking patterns Treat with confidence. Trusted answers from the American Academy of Pediatrics. Problem Solving Skills Try to lighten the load. List and prioritize problems. Focus on small, specific steps. Behavioral Rehearsal and Social Skills What things trigger mood problems? o Identify emotional cues and talk them through. o Plan and practice new responses. Treat with confidence. Trusted answers from the American Academy of Pediatrics. Behavioral Activation Plan short-term activities which give enjoyment or build confidence. Practice healthy habits. o o o o Exercise Caffeine intake Sleep patterns Nutrition An example… So, what would make it go better? Are there any other things people could be thinking? Exactly. What if you tried to smile back? If you don’t get a response, maybe they’re having a bad day. Lunch is awful. Everyone is staring at me. They all think I’m stupid. If I had someone to sit with…and if people didn’t stare like I was stupid. You mean like maybe they had a fight with a friend or failed a test? Treat with confidence. Trusted answers from the American Academy of Pediatrics. When to Consider Medication Significant impairment or distress Recurrent or persistent symptoms Inability to access psychosocial interventions When to Refer Longer duration or recurrent episodes Lack of response to first-line treatment Significant impairment Environmental stressors Use of drugs and alcohol Treat with confidence. Trusted answers from the American Academy of Pediatrics. Selective Serotonin Reuptake Inhibitors (SSRIs) SSRI Starting Increments, Effective Dose, mg mg Dose, mg Maximum Dose, mg Fluoxetine (Prozac®) 10 10-20 20 60 Sertraline (Zoloft®) 12.5-25 12.5-25 50 200 5 5 10 20 Escitalopram (Lexapro®) Adapted from Cheung AH, Zuckerbrot RA, Jensen PS, et al. Guidelines for Adolescent Depression in Primary Care (GLAD-PC): II. Treatment and ongoing management. Pediatrics. 2007;120(5):e1313–1326. Treat with confidence. Trusted answers from the American Academy of Pediatrics. US Food and Drug Administration Indications Anxiety disorders o Sertraline (Zoloft®): age ≥6 for obsessive-compulsive disorder (OCD) o Fluoxetine (Prozac®): age ≥7 for OCD Depression o Fluoxetine (Prozac®): age ≥8 o Escitalopram (Lexapro®): age ≥12 Treat with confidence. Trusted answers from the American Academy of Pediatrics. Dosing Considerations Start low, go slow. Increase dose after 1-2 weeks, then monitor. Maximal effectiveness after 4-6 weeks. Continue for 6-12 months after symptoms resolve. Taper when discontinuing to avoid withdrawal effects. Treat with confidence. Trusted answers from the American Academy of Pediatrics. Contraindications Bipolar disorder Psychosis Interactions/Precautions Use with caution in other serotonergic medications Serotonin syndrome o Mental status changes o Autonomic instability o Tremor, myoclonus Treat with confidence. Trusted answers from the American Academy of Pediatrics. Adverse Event Monitoring Nausea Headaches Dizziness Insomnia Activation Bipolar switching Sexual dysfunction Suicidal thinking--? http://www.glad-pc.org/ Treat with confidence. Trusted answers from the American Academy of Pediatrics. Key System Components: A Screening Checklist Processes Documentation Confidentiality Emergencies Care coordination Skills Assessment Intervention Resources Referral sources Consultation Patient education BUCKEYE STATE PRIMARY CARE Process Title: Mental Health Crisis Plan Purpose: Procedure for a child who is from our office that expresses thoughts of harm to self or harm to others. Procedure Steps: PRESENT and IN OUR OFFICE 1. The provider is to evaluate, document, and determine if the child is in an acute mental health emergency (i.e. expressing harm to self or harm to others). 2. Referral to PIRC (Psychiatric Intake Response Center) 3. Security to be called (XXX-XXXX) to escort the child in a wheelchair to the emergency room (ER). 4. The provider calls the ER – Comm Center (XXX-XXXX) 5. Clinical staff talk or walk down to share information with the ER triage nurse. Treat with confidence. Trusted answers from the American Academy of Pediatrics. Resources Patient Health Questionnaire-9 (PHQ-9) Modified for Teens http://www.thereachinstitute.org/images/GLAD-PCToolkit_V2_2010.pdf American Academy of Pediatrics (AAP) Addressing Mental Health Concerns in Primary Care: A Clinician’s Toolkit http://shop.aap.org/Addressing-Mental-Health-Concerns-in-Primary-Care-AClinicians-Toolkit AAP Pediatric Psychopharmacology for Primary Care. http://shop.aap.org/Pediatric-Psychopharmacology-for-Primary-CarePaperback Brief Online Videos about Common Behavioral Health Problems http://pediatriccare.solutions.aap.org/video-series.aspx?categoryid=41125 Treat with confidence. Trusted answers from the American Academy of Pediatrics. Credits John Duby, MD; Larry Wissow, MD; and the Building Mental Wellness Team Additional funding provided by National Institute of Mental Health (NIMH) and the Duke Endowment Many thanks to our friends and colleagues who acted in the videos and who took part in prior versions of the training North Carolina collaborators: North Carolina Psychoanalytic Society (NCPS); North Carolina Academy of Family Physicians (NCAFP); North Carolina Psychological Association (NCPA); National Alliance on Mental Health (NAMI) of North Carolina; and Northwest Area Health Education Center (NW AHEC) Treat with confidence. Trusted answers from the American Academy of Pediatrics. Visit Pediatric Care Online today for additional information on this and other topics. http://pediatriccare.solutions.aap.org Pediatric Care Online is a convenient electronic resource for immediate expert help with virtually every pediatric clinical information need with must-have resources that are included in a comprehensive reference library and time-saving clinical tools. Don’t have a subscription to PCO? Then take advantage of a free trial today! Call Mead Johnson Nutrition at 888/363-2362 or, for more information, go to http://pediatriccare.solutions.aap.org/SS/Free_Trial.aspx