Nursing Care for Labor and Delivery
advertisement

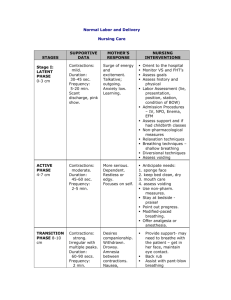
Establishing a Therapeutic Relationship Establishing a Therapeutic Relationship Make the family feel welcome Determine family expectations about birth Convey confidence Use touch for Comfort Respect cultural values Health History Once the woman has been admitted and labor progress has been assessed, the following additional information regarding health history is collected: Personal data – blood type, allergies, etc. History of previous illnesses Problems with this pregnancy Preferences for labor and delivery Preparation for childbirth Admission to Labor and Delivery Assessments performed on admission include: Vital signs Physical exam with a vaginal exam Contraction pattern Membrane status Fetal status Psychosocial assessment, cultural assessment Preparation for labor and delivery Assessment of Contractions Palpation Electronic Monitoring Vaginal Examination Palpation Leopold’s Maneuver Start by: Stand on the Right side, face the woman and palpate with the palms of the hands. Step 1 - Start at upper fundus and palpate for the head or buttocks Step 3 - Gently grasp lower portion of uterus and feel for the head Step 2 - Go down each side and locate back Step 4 - Turn and face the woman and repeat the steps. Characteristics of a Contraction Latent Phase • Every 10-30 min. progressing to • Every 5-7 min. X 30-40 sec. Active Phase • Every 2-5 min. X 40-60 sec. • Moderate to strong Transition Phase • Every 1½ -2 min. X 60-90 sec • Strong Auscultation Location of FHR in relation to the more commonly seen fetal positions Ask Yourself? If the fetal heart tones (FHT’s) are heard loudest (PMI) in the patient’s upper right quadrant of her abdomen, the fetus would be assessed for a breech presentation. A. True B. False Vaginal Examination Information Obtained: Presentation Position Condition of Membranes -ruptured or intact Dilation - enlargement and widening of os ( cm.) Effacement- thinning of the cervix (%) Station Engagement Fetal Oxygenation Main assessments related to fetal well-being are: Fetal Heart Rate Contractions Characteristics of amniotic fluid Maternal vital signs Signs and Symptoms of the Stage 1 - Latent Phase Contraction: dilate 0-3 cm. Mild Duration – 30-45 seconds Frequency – 5-20 minutes Scant pinkish discharge, bloody show Mother’s response Surge of energy and excited Talkative, outgoing Anxiety low **Best time to do teaching! Nursing Care Stage 1 – Latent Phase Welcome to the Hospital Assess goals for this labor Assess Psychological response Orient to common procedures Vital signs and FHT’s Enema IV NPO Assessment of Labor Progress – dilation, effacement, station, lie, etc. Stage 1 – Active Phase Signs and Symptoms Contractions – dilate 4-7 cm. Moderate Duration – 45-60 seconds Frequency – 2-5 minutes Mother’s Response More serious Determined, Dependent Restless Focuses on self Stage 1 – Active Phase Nursing Care Anticipate Needs: Sponge face with cool cloth Keep bed clean and dry- change chux Provide with mouth care – lip balm to lips Assess voiding Non-Pharmacological Measures Modified breathing Effleurage Music Analgesia and Anesthesia Stage 1 – Transition Phase Signs and Symptoms Contractions 7-10 cm Strong Irregular with multiple peaks Duration – 60-90 seconds Frequency – 2 minutes Mother’s response Withdrawn, drowsy, Nausea, trembling of legs Irritable, aggressive Urge to push Stage 1- Transition Nursing Care Provide support- may need to breathe with the patient – get in her face Back rub Assist with pant-blow breathing Watch for hypervention – have breathe in mask and slow down the breathing Do NOT allow to push by having patient blowblow-blow with urge. Do not be offended by irritability Stage Two of Labor Signs and Symptoms: Sudden Appearance of sweat on upper lip An episode of vomiting Increase in bloody show Shaking of extremities Increased restlessness Pressure on rectum; involuntary bearing down Bulging of perineum Stage 2 Nursing Care 1. The key to care during this stage is to teach QUALITY PUSHING ! 2. Keep perineum clean and dry 3. Provide quiet environment 4. Support with positive feedback 5. Repeat doctors instructions 6. Allow to hold the baby , Congratulate!! Stage 2 – Nursing Care Stage 3 – Nursing Care Congratulate on delivery of baby Coach in relaxation for delivery of the placenta Initiate contact with the infant May allow to breast feed if desires Test Yourself! The cardinal movement that facilitates the emergence of the fetal head ____________. A. Flexion B. Extention C. External rotation Cardinal movement that allows the smallest diameter of the head to pass through the pelvis is__________________. A. Flexion B. Internal rotation C. Extension Cardinal movement that occurs as the fetal shoulders engage and descend through the pelvis is termed ______. A. Internal rotation B. External rotation Causes of Pain in Labor Stretching of the cervix during dilation & effacement Stage One Uterine Anoxia Stretching of the uterine ligaments Causes of Pain in Labor Distention of the vagina and Perineum Stage Two Compression of the nerve ganglia in cervix & lower uterus Pressure on urethra, bladder, rectum during fetal descent Traction on and stretching of the perineum Factors affecting Mothers Response to Pain in Labor Preparation - Knowledge and confidence gained through childbirth classes Cultural influences on expression of pain Maternal fatigue, anxiety, sleep deprivation Previous experiences with pain Support Methods of Pain Relief Nonpharmacologic Childbirth methods Breathing Techniques Relaxation Techniques Touch Focusing attention on one object Effleurage Non-Pharmacological Sensory Stimulation Listening to music; subdued lighting Imagery Applying heat and cold Massage (lower back); Counterpressure TENS Position Changes Pain Relief in Labor Pharmacologic Methods Analgesia Stadol Barbiturates Seconal; Nembutal Tranquilizers Vistaril Pain Relief in Labor Criteria for administering an analgesic: Needs to be in active phase of labor If give in latent phase – it may slow labor If give in transition phase – can lead to neonatal respiratory depression Anesthesia Regional Paracervical Epidural; Caudal Spinal Pudendal Local General Used mainly in cesarean deliveries Epidural Anesthesia Injection of an anesthetic agent into the epidural space Provides pain relief during labor and delivery Nursing Care related to an epidural Preparation Assess platelet count – must be normal Empty bladder Assess vital signs for baseline IV fluids Following Assess V/S – especially the B/P because the main side effect is hypotension Rotate position between right and left side-lying Assess bladder and catheterize as needed Assess for other side effects and intervene Spinal Anesthesia A local anesthetic is injected directly into the spinal fluid in the spinal canal to provide anesthesia for cesarean birth and occasionally for vaginal birth Pudendal Anesthesia Anesthesia administered transvaginally and intercepts pudendal nerve. Provides pain relief for episiotomy and delivery. Local Anesthesia Local injection of anesthetic agent in the perineum for episiotomy and repair General Anesthesia Mainly used for emergency deliveries via cesarean birth Used for delivery of the woman with active herpes who will require a cesarean delivery. Do not want fetus to go through the birth canal and risk contact. True or False ? The anesthesia used for both labor and delivery is an epidural A. True B. False The nurse would be careful to keep the patient flat following delivery with a pudendal block A. True B. False The initial side effect of an epidural anesthesia is fetal bradycardia A. True B. False The End