(neocortex) Anterior lobe
advertisement

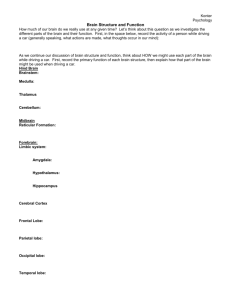
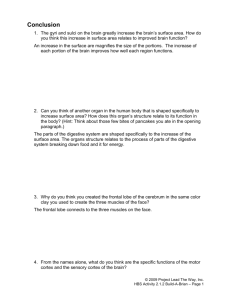
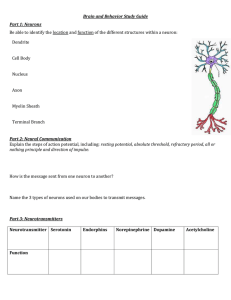
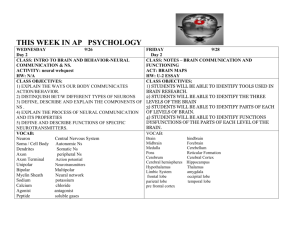
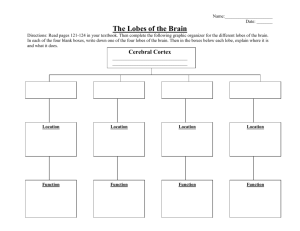
Cerebral Localisation Prof.Dr. S. Naz Yeni Objectives • To learn functional areas of the brain and the brain stem • To learn how to localise the neurologic symptoms and signs to particular areas in the brain. • Although the brain functions are integrated as one unit some certain areas are specialised on particular functions. • Brain lobes • Cerebellum • Brain stem – Mesencephalon – Pons – Medulla oblangata Frontal lobe Frontal lobe is the greatest lobe. Its boundaries are parietal lobe posteriorly and temporal lobe under slyvian sulcus. Areas of major clinical importance Motor cortex (area 4) Suplementary motor cortex (area 6) Frontal eye fields (area 8) Cortical centre for micturation Broca’s speech area (dominant hemisphere) Prefrontal cortex Neighboring structures of clinical interest: olfactory bulb optic nerve Motor cortex • Contralateral weakness usually limited to a body part e.g. Hand, foot, mouth, commisure • Epileptic seizures: focal motor seizures with or without jacksonien march • Parasagittal motor strip lesions may cause bilateral paraplegia.Sphinctary control may be lost in these patients. Eye and head deviation center • Vulpian’s rule: a destructive lesion may cause the head/eye deviate towards the side of the lesion ipsilaterally • Adversive fit: an excitation ( an epileptic seizure) may cause contralateral deviation of eye/head Prefrontal cortex • Frontal lobes play a major role in acquired social behavior: executive functions, abstraction, reasoning, attention. Lesions in prefrontal cortex causes personality change. • Personality change may present in two diferrent ways: inhibitory, dysinhibitory type • Inhibitory type: patient becomes apathic. Executive dysfunction is the prominent feature. • Loss of drive, apathy occurs. Decrease in personal hygiene, loss of concern about personal, social and famıly, business affairs. • Dysinhibitory type: manic-like behavior occurs. Patient doesn’t obey social rules. he may well urinate in public without any feeling of ashame. Such a patient can use inproper language and slang words. Extrafrontal signs • Foster Kennedy syndrome : tumors growing at the base of frontal lobe such as a meningioma of sphenoid bone may cause: Ipsilateral anosmia Ipsilateral optic nerve atrophy Contralateral papilla edema Additional signs • If the lesion is in the dominant hemisphere Broca’s type of dysphasia (expressive type) may occur. • Grasp reflex: indicates contralateral frontal lobe damage.If there is bilateral grasp reflex this may indicate bilateral damage in the frontal lobes. Temporal lobe • Anteriorly frontal lobe, posteriorly there is occipital lobe. It is folded on itself .Temporal lobe has two distinct part: medial and lateral. • Medial: hippocampus amygdala, uncus, parahippocampus etc.. • Lateral: primary auditory and vestibular cortex, associated visual cortex, central representation of receptive language (Wernicke) area. • Deep in the layers passes the visual pathways forming Meyer’s loop. Functions • Hippocampus: memory formation (recall of the recent memory) visceral motility functions • Uncus: smell and taste represantation • Amygdala: autonomic activity via the connections with hypothalamus sexual behavior • A part of limbic system. Connections with frontal lobe have implications on behavior personality Clinical features • • • • Epileptic seizures Wernicke’s type of receptive dysphasia Upper homonym quadrantanopsia Emotional facial asymmetry Epileptic seizure Auras implying temporal lobe epilepsy; Hippocampus: epigastric rising sensation, deja vu, jamais vu like feelings.. Amygdala: fear, palpitation, autonomic symptoms (piloerection, sweating, mydriasis) Uncus: gustatory, olfactory hallucinations Lateral temporal lobe: Vestibular, auditory hallucinations, complicated visual hallucinations Parietal lobe • Extending from rolandic sulcus posteriorly to the parieto-occipital junction. Below there is temporal lobe. Critical zones • Somato-sensory cortex: 3,1,2 • Receptive language area of Wernicke (at the junction with temporal lobe: opercular area) • Visual pathways Signs and symptoms • Lower quadrantanoptic homonym hemianopsia • Wernicke’s (receptive) type of dysphasia in the dominant hemisphere • Cortical sensory loss : astereoagnosia, loss of two point discrimination, extinction phenomenon. • Apraxia (dominant hemisphere lesions) • Anosagnosia (nondominant hemisphere lesions) Gerstman syndrome (angular gyrus/dominant side) • • • • Loss of right/left discrimination Acalculia Finger agnosia Alexia with agraphia Some definitions • Apraxia: loss of ability of learned motor skills Ideomotor apraxia: when asked “as if to brush teeth” patient can not perform. However in daily life spontaneous acts are performed. Ideational apraxia: the patient can not program, plan multistep activities. Daily life may be problematic. • Agnosia:is a loss of ability to recognize objects, persons, shapes, etc. while the specific sense is not defective. Some definitions • Dyslexia(word blindness): loss of ability to reading • Anosagnosia: denial, hemineglect • Asteroagnosia: inability to identify an object by touch without visual input. Occipital lobe • Primary visual cortex(area 17) is located behind parietal and temporal lobes. Signs and symptoms; • Epileptic seizures • Homonymous hemianopsia (unilateral disease) • Cortical blindness (in bilateral lesions) • Agnosia • Dyslexia Epileptic seizures • occipital lobe seizures start with auras of elemantary visual hallucinations, scotomas, amourosis, homonoym hemianopsia. Bilateral occipital lobe damage • Cortical blindness with macular sparing • If there is widespread damage to the occipital lobes without sparing macular vision, cortical type of blindness occurs. The question is how can we differ such a blindness from a blindness as a result of a bilateral optic nerve disease; importance of light reflex Definitions • Prosopagnosia: Loss of ability to recognize familiar faces. Such a patient can recognize a familiar person by using mimics, emotional clues. The lesion is usually located in the periphery of occipital lobe bilaterally(not in the primary visual cortex). • Visual agnosia: loss of ability to recognise visual stimuli; may describe all details of a picture but still can not understand the picture as a whole (lesions in the bilateral visual association areas). Cerebellum • • • • Coordination of movement Control of gait, posture (Balance ) Control of muscle tone (Motor control ) Cognitive functions – Attention – Emotions – Language Features with regard to lobes Posterior lobe (neocortex) Anterior lobe (paleocortex) Flocculonodulus (archicortex) Ataxia + ++ + Nystagmus + - +/_ Intentional tremor ++ - _ Hyptonia +/_ ++ +/_ Rebound + +/_ _ Dysmetria.. ++ _ _ Mesencephalon Midbrain is located above pons and below diencephalon(thalamus). Critical structures: Edinger westphal nuclei 4 th nerve nuclei Substantia nigra Crus cerebri Well-known vascular syndromes Weber’s syndrome • Ipsilateral 3rd nerve palsy • Contralateral hemiparesis Benedikt’s syndrome • İpsilateral tremor(nucleus ruber) • Cerebellar signs • 3rd nerve palsy Pons • Location: below midbrain, above medulla oblangata and in front of cerebellum • Spinothalamic tract • Corticospinal tract • Cerebellar peduncles Pons; important structures • mid-pons: The chief or pontine nucleus of the trigeminal nerve sensory nucleus (V) • mid-pons: the motor nucleus for the trigeminal nerve (V) lower down in the pons: • abducens nucleus (VI) • facial nerve nucleus (VII) • vestibulocochlear nuclei Well-known vascular and nonvascular syndromes • Millard-Gubler syndrome • Locked-in syndrome • Cerebello-pontine angle tumors Crossed motor deficits • Ipsilateral 6th nerve palsy • Ipsilateral 7th nerve palsy • Contralateral hemiparesis Locked-in syndrome • Occlusion of basilary artery may cause this syndrome. The signs consist of quadriplegia and the inability to speak in otherwise cognitively intact individuals. Consciousness is preserved.Those with locked-in syndrome may be able to communicate with others through coded messages by blinking or moving their eyes, which are not affected. Cerebello-pontine angle tumours • This is usually a schwannoma of 8 th nerve. • One sided sensorineural hearing loss may last many years before diagnosis. Additional features may be; • 5th nerve (loss of cornea reflex) palsy • 6, 7th nerve palsies • Cerebellar features Medulla oblangata • It is the lower half of brain stem below pons. • • • • • Corticospinal tract and the decussation Spinothalamic pathway and the leminiscus Cerebellar peduncles (inferior) 9,10,11,12 cranial nerves and the nuclei Autonomic fibers Wallenberg syndrome (lateral medullary syndrome) • • • • • • • A vascular syndrome Vertigo Nausea, womiting Ipsilateral cerebellar findings, ataxia Difficulty in swallowing Horner’s syndrome Crossed sensory deficit (one sided facial, contralateral-sided body)