How well are we doing? Measuring the quality of end-of
advertisement

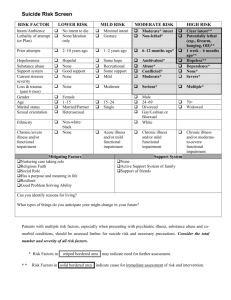
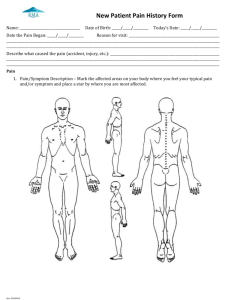
Measuring the quality of endof-life care David J Casarett MD MA Division of Geriatrics University of Pennsylvania Did this patient receive good care? 84 year old man with heart failure and pneumonia. Admitted to the hospital, treated with antibiotics and oxygen. Discharged 3 days later. What is good care for pneumonia? How do you measure the quality of care for pneumonia? Patient received: » Antibiotics » Oxygen » Intravenous fluids Patient was discharged from the hospital alive Did this patient receive good care? A 69 year old man with severe heart failure. Admitted to the hospital with pneumonia, and treated with antibiotics and oxygen. Despite the best treatment, his condition becomes worse. He dies 3 days later. What is good care for dying patients? How do you measure the quality of care for dying patients? Measuring the quality of care for dying patients: Why measure the quality of end-of-life care? A framework for measurement » Structures of care » Processes of care » Outcomes Measuring outcomes » Prospective data » Retrospective data One example: Measuring pain management Good end-of-life care includes palliative care: Palliative care is patient and family-centered care that focuses upon effective management of pain and other distressing symptoms, while incorporating psychosocial and spiritual care according to patient/family needs, values, beliefs, and culture(s). (NCCN) Why measure the quality of end-oflife care? Benchmarking Quality improvement Identification of best practices “Benchmarking” Identifying goals and targets for high quality Examples: » We should assess the pain of all patients » We should use strong opioids (morphine) for severe pain in all patients “Quality improvement” Interventions to improve the quality of care that patients receive. Examples: » Training for physicians and nurses about how to assess pain » Reminders to assess pain in all patients » Pharmacy suggestions about which opioids to use “Best practices” Procedures and rules that lead to better care Examples: » One hospital uses a pain assessment form as part of the admissions process, ensuring that all new patients have their pain assessed » One hospital created rules to guide physicians in using strong opioids (morphine) when appropriate. Measuring quality of end-of-life care Measuring quality of end-of-life care makes it possible to do benchmarking, quality improvement, and to identify best practices. But: How do we measure the quality of endof-life care? 3 ways to measure quality Structures of care Processes of care Outcomes of care Structures, Processes, and Outcomes STRUCTURES PROCESSES OUTCOMES “Structures of care” Aspects of the health care system that contribute to better quality of care Examples: » » » » Staffing Training Protocols Procedures What structures would lead to better quality end-of-life care? » Staffing—Dedicated physicians and nurses for palliative care » Training of all staff in palliative care » Palliative care teams » Protocols for pain management » Procedures for pain assessment Advantages of measuring structures Easily measured through surveys or existing data Easy to compare hospitals Quick indicators of needs/problems Disadvantages of measuring structures Not usually responsive to change Not always related to quality Generally not sufficient to demonstrate effectiveness or success Processes STRUCTURES PROCESSES OUTCOMES “Processes of care” Care that is delivered to patients in order to improve the quality of care Examples: » Assessing pain and other symptoms » Prescribing medications » Prescribing non-medical treatment What processes would lead to better quality end-of-life care? » » » » Assessing pain Having patient seen by a palliative care service Prescribing opioids (morphine) Using a bowel regimen alongside opioids Advantages of measuring processes Easily measured (in some settings) Responsive to improvement efforts/funding Disadvantages of measuring processes May be more associated with better care in some hospitals than others Positive results may offer false sense of improvement Processes not always associated with better care* *Processes and outcomes One physician prescribes morphine to all of his patients with cancer Another physician prescribes morphine to half of his patients with cancer Which physician is providing better care? ? Outcomes STRUCTURES PROCESSES OUTCOMES “Outcomes of care” The effect that structures and processes have on the patient Examples » » » » Control of symptoms Quality of life Comfort Being with family What outcomes of care are important to patients near the end of life? Pain Other symptoms Adequate control over health care decisions (patient’s perspective) Family adjustment after death Advantages of measuring outcomes Ideal measure of needs Measured from the patient’s perspective Disadvantages of measuring outcomes Change may be slow Positive/negative results may be due to other factors Accurate measurement is often: » Difficult » Expensive Which outcomes are most important? The patient’s spiritual and psychological wellbeing Continuity of care across providers and care settings The patient’s physical comfort Information and control over treatment Family adjustment after death Family psychological, spiritual, and social wellbeing The patient’s physical comfort Pain Nausea Pruritis Constipation Dyspnea Thirst Dry mouth … The patient’s spiritual and psychological well-being Psychological: » Depression » Anxiety » Confusion Spiritual/emotional » Peacefulness » Sense of community » Reconciliation with friends/family Information and control over treatment Culturally appropriate understanding of treatment options Culturally appropriate understanding of prognosis and illness trajectory Treatment consistent with preferences Site of death consistent with patients’ and families’ goals Family psychological, spiritual, and social well-being Family’s acceptance of death Reconciliation Caregiver burden Provisions for family members and children Continuity of care across providers and care settings Continuity of information Continuity of treatment Continuity of health care providers Family adjustment after death Adjustment Contribution of grief support (formal/informal) Guilt/acceptance “Prospective” vs. “Retrospective” measurement? Prospective: Going forward Retrospective: Asking patients or families to remember Prospective data: Advantages and disadvantages Advantages: » “Gold standard” of data collection (from patients) Disadvantages: » Challenges of identifying patients near the end of life » Challenges of data collection What proportion of patients near the end of life can provide data? 65% (Fowler 1999) 65% (Lynn 1997) 50-63% (Hospice)(Casarett 2004, Casarett 2005, Rickerson 2005) Declines over time (Stromgren 2005) • 82% at baseline • 70% at week 1 • 69%-52% at weeks 2 – 13 The problem of attrition in a hospice population Number of Responses and Deaths/Terminations 90 80 70 60 50 40 any response patient response known dead dead or left study 30 20 10 0 1 2 3 Visit Number 4 5 Trajectories of functional decline CHF/COP D Cancer Dementia Retrospective (patient-level) data: Advantages and disadvantages Advantages: » Does not require interaction with patients who are seriously ill » “end-of-life” patients are already defined » Best way to assess family’s experience, especially after patient’s death » Economical Disadvantages: » Biased/inaccurate responses » Not all patients have surrogates How accurate are families’ recollections of care? Ahmedzai (1988) poor agreement (patient-family pre-death) in all symptoms except dyspnea. (Higher scores from families) Milne (2005) better agreement for physical symptoms than for psychosocial well-being (pre-death) --------------------------------------------------------------------------- Higginson (1996) better agreement (pre- vs. post- death) for service provision and communication than for symptom control. Klinkenberg (2003) better agreement for physical symptoms than for psychological symptoms (pre- vs. post-death) Hinton (1996) Patient-family ratings during illness and then after death (families). Good agreement about incidence, less for severity of physical/psychological symptoms. Finding a surrogate No surrogate » Not available » Moved/no forwarding address » None “Wrong” surrogate Changing surrogate Finding a surrogate Consent: 55% Knowledgeable: 64% Reachable: 70% Surrogates: 85% Finding a knowledgeable surrogate 79% (Klinkenberg 2003) 37% (Curtis 2002) 90% (Casarett 2004) 69% (Seale 1995) 38%(?) (Teno 2003) Potential response bias? Patients with surrogates: Differences: » » » » Older Fewer ADL dependencies More likely to be white More likely to have private insurance and/or Medicare BUT: Generally small effect Outline: Why measure the quality of end-of-life care? A framework for measurement » Structures of care » Processes of care » Outcomes Measuring outcomes » Prospective data » Retrospective data One example: Pain measurement Outcome measurement: Pain Pain is often undertreated Pain is often not recognized Pain reduces quality of life and is an important source of discomfort Measuring pain For which patients should pain be measured? How should we measure pain? For which patients should pain be measured? All patients How should we measure pain? Is the patient cognitively impaired? » » » » No Mild Moderate Severe Can patients with dementia report pain? Is the patient cognitively impaired? Mild impairment (Mini Mental State score of >22 out of 30) » Some problems with memory or complex tasks » Often impairment is not noticeable Moderate impairment (Mini Mental State score of 1222 out of 30) » Knows name/location » Able to follow commands » Impaired memory Moderate or severe impairment (Mini Mental State score of <12 out of 30) » » » » May not know name/location Limited understanding Able to follow simple commands only Severely impaired memory Cognitive function and pain assessment Mild impairment » No different assessment techniques Moderate impairment » Additional teaching » Use simple scales with pain descriptions Moderate or severe impairment » Use scale, but also rely on behaviors » Include assessments of family members and caregivers Numeric rating scale: acceptable for mild impairment 0 1 No pain 2 3 4 5 6 7 8 9 10 Worst possible pain Assessing pain in patients with moderate cognitive impairment Rely on patient Surrogate report only if patient cannot reliably communicate Use terms synonymous with pain Use standard pain scale: » 0-10 Numeric Rating Scale » Better: Verbal Descriptor/Pain Thermometer Assessing pain in patients with moderate cognitive impairment Ask about present pain Ensure understanding of tool use » Do a “practice” assessment » Compare pain now with best and worst pain » Check for discrepancies between pain rating and function to identify possible underreporting of pain Verbal Descriptor Scales Verbal Descriptor Scale (VDS) ___ ___ ___ ___ ___ ___ ___ Most Intense Pain Imaginable Very Severe Pain Severe Pain Moderate Pain Mild Pain Slight Pain No Pain (Herr et al., 1998) Present Pain Inventory (PPI) 0 = No pain 1 = Mild 2 = Discomforting 3 = Distressing 4 = Horrible 5 = Excruciating (Melzack & Katz, 1992) Pain Thermometer Pain as bad as it could be Extreme pain Severe pain Moderate pain Mild pain Slight pain No pain (Herr and Mobily, 1993) Assessing pain in patients with severe cognitive impairment Ask the patient Also ask: Family members Caregivers Particular attention to factors that could increase pain (movement, bathing, transfers, dressing changes) Use simple scale and/or behaviors to assess severity Facial Pain Scales Faces Pain Scale Bieri D et al. Pain. 1990;41:139-150. Behaviors and non-verbal clues Direct Observation or History from Caregiver for evidence of pain-related behaviors (during movement, not just at rest) Facial expressions of pain (grimacing) » Less Obvious: slight frown, rapid blinking, sad/frightened face, any distorted expression Vocalizations (crying, moaning, groaning) » Less obvious: grunting, chanting, calling out, noisy breathing, asking for help) Body movements (guarding) » Less obvious: rigid, tense posture, guarding, fidgeting, increased pacin, rocking, restricted movement, gait/mobility changes such as limping, resistance to moving The importance of recognizing changes as clues to pain Changes in Interpersonal Interactions Combative/ aggressive Resisting care Decreased social interactions Socially inappropriate Disruptive Withdrawn Changes in Activity Patterns/Routines Sudden cessation of common routines Increased wandering Difficulty sleeping Increase in rest periods Refusing food/appetite change Changes in Mental Status Irritability or distress Increased confusion Agitation Crying or tears Algorithm for assessing pain in severe cognitive impairment 1. Unusual behavior should trigger assessment of pain as a potential cause But: Some patients exhibit little or no pain-related behaviors associated with severe pain 2. 3. 4. 5. 6. Are Comfort Needs Being Met? Evidence of pathology that may be causative (e.g. infection, constipation, fracture)? Assess patient report (if possible) Assess behaviors Attempt an analgesic trial 1. 2. If in doubt, analgesic trial may be diagnostic Acetaminophen 500mg TID, (titrate up to 3-4G/day) Summary of pain measurement Overview Challenges and approaches Mild to moderate cognitive impairment Moderate to severe cognitive impairment Examples of tools to assist assessment » » » » Intensity Scales Interview Guide Pain-related Behaviors Approach to Nonverbal Cognitively-Impaired Older Adult Outline: Why measure the quality of end-of-life care? A framework for measurement » Structures of care » Processes of care » Outcomes Measuring outcomes » Prospective data » Retrospective data One example: Pain measurement