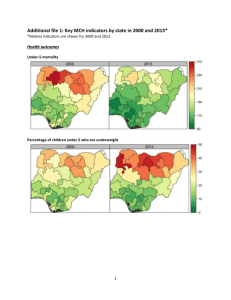
Web Appendix: Additional description of
advertisement

Web Appendix: Additional description of methods for estimating malaria deaths prevented 2001-2010 using the Lives Saved Tool (LiST) model 1. African countries included in this analysis Thirty-six countries in malaria-endemic Africa were included in the analysis of the impact of vector control on child mortality (figure 1). Gabon was excluded due to lack of available data. Cape Verde, Comoros, Botswana, Djibouti, Namibia, Sao Tome and Principe, South Africa, Lesotho and Swaziland were excluded due to the low number of malaria deaths in these countries [1]. The 36 countries included in the analysis represent 98.5% of the population at risk of malaria in sub-Saharan Africa (SSA) or 99.7% of the malaria-caused mortalities in 2000 in SSA [1, 2]. Thirty-one malaria endemic countries were included in the analysis of the impact of malaria prevention in pregnancy on malaria-caused child mortality. Cape Verde, Comoros, Eritrea, Burundi, Ethiopia, Mauritania, Botswana, Djibouti, Namibia, Rwanda, Sao Tome and Principe, South Africa, Lesotho, and Swaziland were excluded because malaria prevention in pregnancy has little to no effect in countries with low transmission, thus there is no official policy for malaria prevention in pregnancy with intermittent preventive treatment (IPTp) in these countries [3, 4]. The 31 countries included in the analysis account for 88.3% of the population in SSA at risk of malaria and 90.0% of the malaria-caused child deaths in 2000 in SSA [1, 2]. 2. LiST model overview The LiST model used in this analysis (version 4.22) and accompanying documentation can be downloaded from www.jhsph.edu/dept/ih/IIP/list/. LiST is a computer projection model used to estimate the number of deaths that can be prevented as a result of scaling up effective child health interventions. A complete description of the uses of LiST and background on its creation, including expert technical inputs, are described in detail elsewhere [5]. LiST is programmed as a module in the demographic projection model SPECTRUM, as described elsewhere [6]. LiST uses a simple cohort model that follows children through five age bands from birth to five years to estimate the number of neonatal and child deaths that could be prevented by different intervention scale-up scenarios. The model can be used to make future projections of deaths prevented from intervention scale-up, compared to a baseline of the current year, or can be used retrospectively to estimate the number of deaths that were prevented in the past from intervention scale-up, compared to a historical baseline year. The model estimates child deaths prevented (within specific cause of death categories) due to 1 intervention scale-up within a specified country as a function of three primary parameters: 1) the number of child deaths by cause projected to occur in each year (including population growth parameters over time); 2) the protective effect (PE) on cause-specific mortality (PE = 1-relative risk*100) for each intervention being scaled-up; and 3) increases in population coverage of each intervention. After accounting for population growth, the model computes the number of deaths prevented by cause each year as the difference between the estimated deaths that occur with intervention scale-up and the estimated deaths that would have occurred had no scale-up occurred beyond the level at a baseline year. The following basic equation is used within the model to estimate the number of child malaria deaths 1-59 months that were prevented from increases in vector control coverage (insecticide-treated mosquito nets [ITNs] and indoor-residual spraying [IRS]), where cause i is malaria and intervention j is vector control: Deaths Avertedijs = Deaths Averted Totals * (%RedMorttij / %RedMortsTotal) %RedMortijs = [Iij * (Pjt – Pj0) ]/ (1 - Iij* Pj0), %RedMortijs = % reduction in mortality from cause i by scale-up of intervention j Iij = effectiveness of intervention j in reducing mortality from cause i P j0 = baseline coverage of the intervention j P js = scale-up coverage for the intervention j where While low birth weight (LBW) is due to either intrauterine growth retardation (IUGR) or preterm delivery, the effect of malaria prevention interventions during pregnancy (either through ITNs or IPTp) on LBW in the LiST model acts solely through IUGR. The effect of reducing IUGR has two effects in the LiST model for estimating <5 child deaths prevented, as noted elsewhere [7, 8]. First, children with IUGR have a greater relative risk (RR) of dying during the neonatal period, with increased RR of dying due to diarrhea [RR = 2.0], sepsis/pneumonia (RR =2.0), and asphyxia (RR = 2.3). Second, IUGR increases the chance that the child will be stunted, which in turn increases the RR for measles, malaria, diarrhea and pneumonia deaths in the post-neonatal period. In this analysis, the effect of malaria prevention in pregnancy acted only on deaths from the first 2 pregnancies of women in each country. The following basic equation is used within the model to estimate the number of child malaria deaths 1-59 months that can be prevented from malaria prevention in pregnancy, where cause i is deaths from IUGR and intervention j is composite indicator for ITNs and IPTp in the first 2 pregnancies: 2 %RedIUGRj = Ij (Pjt – Pj 0) /(1 – IjPj 0), where %RedIUGRj = percent of reduction in IUGR due to intervention scale-up of j Ij = proportion by which intervention j reduces IUGR P j0 = baseline coverage of the intervention j P js = scaled-up coverage for the intervention j 3. Within country estimates of cause-specific child deaths Within the LiST model, the number of disease/condition-specific deaths among children under 5 years old in each country is based on country-specific estimates of cause-specific mortality for all low- and middle-income countries, whereby a disease/condition-specific mortality profile is applied to the estimated total number of deaths among children <5 estimated for each country each year. These estimates were developed for the period 2000-2003 for WHO and UNICEF by CHERG [9] and then reviewed by national programs before being adopted as the official UN estimates of cause-specific mortality for children <5. The number of malaria deaths in children 1-59 months in our baseline year of 2000 was estimated as the proportion of the 1-59 month all-cause mortality envelope attributable to malaria by the CHERG for each sub-Saharan African country [10]. 4. Estimates of intervention effectiveness As described in detail elsewhere, the PE of vector control for preventing malaria deaths in children 1-59 months has been estimated to be 55% (range 49% - 60%) based on a systematic review of related trials and studies [11]. The PE of malaria prevention during pregnancy for preventing low-birth weight has been estimated to be 35% (95% confidence interval [CI] 23-45%) during the first 2 pregnancies in malaria endemic areas in the presence of SP resistance based on a systematic review of related trials [11]. 5. Methods for obtaining survey point estimates for malaria prevention intervention coverage 20002010 The majority of malaria deaths occur in rural areas [12]. It has also been shown that intervention coverage in rural areas lags behind urban areas in many countries in Africa, especially prior to 2005[13, 14]. For these reasons and to be most conservative, the level of malaria prevention intervention coverage in rural survey strata were used for the national-level estimates for each country for estimating the malaria deaths prevented from intervention scale-up at the national level. 3 5.1. Estimating yearly vector control intervention coverage (ITNs/IRS) 2000-2010 As outlined elsewhere [11], estimates of the proportion of households protected by vector control in the Lives Saved Tool (LiST) is defined as a household owning either ≥1 ITN or a long lasting ITN (LLIN; henceforth referred to as ITN), or having received IRS in the past 12 months. Vector control coverage estimates from 2000 through 2010 were used in the LiST analysis to estimate the malaria deaths prevented 2001-2010, compared to a baseline of 2000. These estimates were obtained from reports of national household surveys that included the Demographic and Health Survey (DHS), the Multiple Indicator Cluster Survey (MICS), the Malaria Indicator Survey (MIS), and AIDS Indicator Survey (AIS). If the survey was conducted across 2 calendar years (i.e. 2005-2006), the estimate was applied to the earlier year. Empirically-estimated standard errors adjusted for correlated data at the cluster level were ascertained from all available survey datasets to obtain 95% CIs about survey estimates. For those surveys without available datasets and where standard errors were not reported (33 of 74), standard errors were imputed using the point estimate, sample size and assuming a design effect of 2 (Equation 1). standard error = 2 * square root [1 / (point estimate * 1 – point estimate)] Formula 1 Most DHS and MICS from 2000-2001 did not ascertain information on the number of ITNs per household, only on the proportion of children <5 sleeping under an ITN the previous night. To estimate household possession of an ITN from such surveys without household possession information, we used the empirical relationship (ratio) between ITN household possession and child ITN use reported in surveys within the same country at a later time point. Empirically-estimated standard errors for these estimates were then imputed using Model 1. This method of household ITN estimation was used for the following countries 2000-2001: Angola, Benin, Burundi, Cameroon, Central African Republic, Cote d’Ivoire, Democratic Republic of the Congo, Gambia, Guinea-Bissau, Kenya, Malawi, Niger, Rwanda, Senegal, Sierra Leone, Tanzania, Togo, Uganda and Zambia (Table 1). The bulk of the scale-up of ITNs/IRS occurred after 2004 across Africa [15]. To avoid using a linear interpolation between survey data points, for the period of 2004-2008ITN procurement data from manufactures for each country were used to inform ITN coverage estimate changes between survey 4 estimates as follows. Predicted estimates of the proportion of households with ≥1 ITN within each country 2004-2008 were ascertained from a basic linear regression model. The model quantified the observed relationship between net delivery data from manufacturers, aggregated yearly, and ITN household coverage estimates from household surveys. Data on the delivery of ITNs and LLINs to countries from manufacturers 2004-2008 were obtained from the Net Mapping Project (John Millner USAID). Under this project, yearly data on the number of ITNs and LLINs purchased and shipped to countries were obtained from Sumitomo/A-Z, Vestergaard-Frandsen, Clarke, BASF, Intection/BestNet and Tana Netting. Estimates of national ITN household possession from nationally-representative household surveys 2004-2008 were obtained as outlined above. ITNs reported delivered by manufacturers older than 3 years (i.e. those nets delivered to countries more than 3 years ago) were subtracted from the cumulative number of nets each year. To account for the lag between ITN manufacturer delivery to the country and availability to the household, yearly cumulative ITN delivery estimates were lagged by one year. The 3-year lagged cumulative ITN delivery estimates were then standardized across countries by the number of households within the country, with the final variable henceforth referred to as yearly corrected ITN delivery estimates. There were 47 data points across countries between 2004 and 2008 with both a survey-derived estimate of ITN household possession and yearly corrected ITN delivery estimates. In addition to the yearly corrected ITN delivery estimates, the following covariates were included in the regression model and tested for model fit: year, proportion of households within each country at risk for malaria, as defined by MARA http://www.mara.org.za/, the gross national income for 2006 (GNI), and a dichotomized variable (0,1) indicating if the country was a Presidents Malaria Initiative (PMI) country in a particular year. The fit of models with the squaring, cubing, log, exponent and quadratic of yearly corrected ITN delivery estimates was assessed using an Ftest. The following model had the best fit (R2 = 0.7099, F-test = 20.07, df = 46, P-value < 0.0001): Proportion of households with ≥1 ITN = -8612.68154 + 18.74738*(corrected net delivery) + -0.00095456*(proportion of households at risk for malaria) + 4.30381*(year) + -0.00466*(GNI) + 9.40987*(PMI) Model 1 The predicted estimates from Model 2 were not actually used in the LiST analysis reported here in place of survey estimates (Table 2). Rather, the percent changes year to year (slope of the line) from the predicted results of Model 2 were used to inform changes in household ITN possession between household survey estimates 2004-2008. In the case that this percent change showed a decline in 5 coverage, ITN coverage was held constant until it began to rise again. An actual decline in ITN coverage is unlikely due to the large increase in funding for malaria interventions throughout this time period. This occurred in 4 instances: Cote d’Ivoire, Nigeria, Togo and Zambia. Coverage from years 2000-2003 was estimated using linear interpolation from the earliest survey point estimate to the 2004 estimate obtained using the above method. For those countries without a survey estimate in 2000, the 2000 estimate was set to the survey estimate in 2001 with its respective 95% confidence intervals. If the country did not have a 2001 survey, the estimate in 2000 was set to 1.9, the mean estimate across all 2000-2001 survey estimates with the exception of Gambia 2000 (Gambia had very high net coverage in 2001 [20.2%] due to the ITN trials that occurred, and was therefore excluded from the estimation of the mean ITN coverage in 2000). The standard error from the earliest survey was then applied to the midpoint estimate 2000-2003 to obtain uncertainty intervals. A survey in 2003 in Mauritania estimated household ITN possession to be 0.6, and so this value with its respective 95% confidence interval was used for 2000-2002. This process yields the most conservative increase in ITN coverage. Although perhaps overestimating the proportion of rural households owning an ITN in 2000, it will yield the most conservative impact throughout the decade. Coverage for years 2009-2010 were projected by applying the linear slope between the most recent survey and the earliest survey. This approach yielded the most conservative slope for this period while maintaining the likely increase in coverage due to increasing funding. The 2004 DHS conducted in Chad did not estimate household ITN possession, but did however show the proportion of households owning a mosquito net to be 61% among rural households. The ratio of the proportion of households owning a mosquito net to the proportion of households owning ≥ 1 ITN was ascertained for Burkina Faso and then applied to Chad. The standard error was then imputed using model 1 to achieve 95% CIs. Burkina Faso was used because of the similarity in climate, mosquito net culture, and proximity of survey date. Sudan’s household survey in 2006 did not specify between urban and rural populations, thus the overall proportion of households owning ≥1 ITN was used. Eritrea’s estimate of ITN coverage in 2003 was taken from the published results of a sub-national survey [16] that included 3 of the 4 zobas surveyed in the 2008 MIS. Information was unavailable for mainland Equatorial Guinea. However, considering that Bioko Island is 28.6% of the population of Equatorial Guinea we applied the coverage reported from malaria prevention interventions on the island [17] and 6 multiplied the results by 28.6%. The national survey in Niger 2010 did not report a rural estimate. To estimate the rural estimate from the total estimate, the ratio of total ITN coverage to rural ITN coverage in the 2009 Niger survey was applied to the 2010 estimate. Resultant ITN/IRS coverage changes for each country 2000-2010, with uncertainty, are presented in Figure 2. 5.2. Estimating yearly intervention coverage for malaria prevention in pregnancy (IPTp/ITN) 2000-2010 As outlined elsewhere,[11] protection by malaria prevention in pregnancy, defined as the higher of the estimates of either proportion of pregnant women using an ITN the previous night or the proportion of women who had a live birth in the past 2 years who received 2+ doses of sulfadoxamine-pyremethamine (SP) during an ante-natal care (ANC) visit (IPTp), were used in the LiST analysis. These estimates were obtained from the final reports of DHS, MICS, MIS and Office of National Statistics (ONS) surveys (Table 3). If the survey did not specify the number of doses of SP or where it was received, the estimate of IPTp taken during pregnancy without specification of number of doses or if taken at ANC was used. This occurred in the following surveys: Congo 2005, Liberia 2005, and Malawi 2000. Standard errors were ascertained from survey datasets to obtain 95% CIs about survey point estimates. In the case that standard errors about the estimate were unavailable, the standard errors were imputed using formula 1. The year prior to the country declaring IPTp with SP as national policy was set to 0%, for those countries using IPTp as the coverage indicator[4, 18, 19]. It was unclear what year Liberia adopted the policy, and so the year 2000 was set to 0 in this case. Where the higher indicator for malaria prevention in pregnancy was ITN use by pregnant women, the coverage of ITNs among pregnant women was set to 0% in 2000. While this may lead to a slight overestimate of the impact of malaria prevention in pregnancy the overall contribution of malaria prevention in pregnancy to the total number of lives saved is quite small. Linear interpolation was used between the first year of measured coverage and the next available survey point estimate. Linear interpolation was also used between multiple surveys where available. The slope between the most recent household survey and the earliest household survey was used to 7 inform the increase for years beyond the most recent household survey through 2010. In the case that there was only 1 household survey in the country, the year set to 0 was used in place of the earliest household survey. Coverage was assumed to never decrease unless surveys estimated otherwise. Resultant IPTp/ITN coverage changes for each country 2000-2010, with uncertainty, are presented in Figure 3. 6. Uncertainty estimation of LiST estimates Uncertainty bounds about total estimated malaria deaths prevented from vector control 2001-2010 were estimated by projecting lives saved when varying the three primary model parameters: 1) estimated malaria deaths within each country; 2) the estimated PE of vector control on malaria mortality; and 3) intervention coverage changes 2000-2010. Using this approach, lower and upper uncertainty bounds were estimated using a high impact / low impact scenario. The uncertainty about the number of malaria deaths among children 1-59 months was derived from the 95% confidence intervals about the proportion of all deaths due to malaria in this age group in 2000 estimated by the CHERG [1]. The reported range of 49-60% about the 55% PE of vector control for preventing malaria mortality was used as the uncertainty about this parameter in this analysis [11]. The uncertainty about ITN scale-up is dependent on the percent change, or the slope of the vector control coverage curve, from 2000-2010. Under the largest-increase scenario, the percent change in coverage was set to that from the lower bound of the 95% CI in 2000 to the upper bound in 2010, resulting in the greatest slope during this period. Under the smallest-increase scenario, the percent change in coverage was set to that from the upper bound of the 95% CI in 2000 to the lower bound in 2010, resulting in the least slope during this period. The slope of each uncertainty bound between 2000-2010 was then calculated in the same manner as the slope of the midpoint over this period (see Figure 1 for resultant uncertainty of vector control scale-up 2000-2010). Uncertainty bounds about total estimated child deaths prevented from malaria prevention during pregnancy 2001-2010 were estimated by projecting lives saved while two primary model parameters: 1) the estimated PE of malaria prevention in pregnancy on preventing LBW; and 2) intervention coverage. The 95% CI of 23-45% about the 35% PE of malaria prevention in pregnancy for preventing LBW was used as the uncertainty about this parameter in this analysis [11]. The uncertainty about IPTp/ITN scaleup under the largest-increase / smallest-increase scenario followed the methodology for vector control 8 outlined above. Linear interpolation was used between bounds (see Figure 2 for resultant uncertainty of malaria prevention in pregnancy scale-up 2000-2010). 7. Estimating total continental coverage Yearly coverage estimates for each country were weighted according to each country’s 2005 population estimate (mid-point of 2000-2010) to estimate the continental coverage rates of vector control in rural areas and malaria in pregnancy prevention in rural areas[20]. 8. Coverage estimation of other interventions in this analysis Using the LiST model, this analysis accounted for the scale-up of other interventions that affect child mortality such as vaccinations and antenatal care. Coverage estimates for these interventions were derived from nationally representative household surveys. Coverage for the years after the survey was held constant. Other LiST inputs not included in the survey or not included in this analysis, one being case management of malaria, were held constant during this time period. As LiST is driven by a change in coverage, these indicators were then assumed to have no effect on child mortality throughout the time period. This method may affect the number of deaths occurring each year, but would have only a minimal effect on the number of deaths prevented due to malaria prevention interventions. 9 References 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. 15. 16. 17. 18. 19. 20. Rowe AK, Rowe SY, Snow R, Korenromp EL, Armstrong-Schellenberg JR, Stein C, Nahlen BL, Bryce J, Black RE, Steketee R: Estimates of the burden of mortality directly attributable to malaria for children under 5 years of age in Africa for the year 2000 Final report. For the Child Health Epidemiology Reference Group (CHERG). In. Washington DC: Child Health Epidemiology Reference Group (CHERG); 2006. Hay SI, Guerra CA, Gething PW, Patil AP, Tatem AJ, Noor AM, Kabaria CW, Manh BH, Elyazar IR, Brooker S et al: A world malaria map: Plasmodium falciparum endemicity in 2007. PLoS Med 2009, 6(3):e1000048. Steketee RW, Nahlen BL, Parise ME, Menendez C: The burden of malaria in pregnancy in malaria-endemic areas. The American journal of tropical medicine and hygiene 2001, 64(1-2 Suppl):28-35. WHO: World Malaria Report 2009. In. Edited by WHO. Geneva: WHO; 2009. Boschi-Pinto C, Young M, Black RE: The Child Health Epidemiology Reference Group reviews of the effectiveness of interventions to reduce maternal, neonatal and child mortality. Int J Epidemiol 2010, 39 Suppl 1:i3-6. Stover J, McKinnon R, Winfrey B: Spectrum: a model platform for linking maternal and child survival interventions with AIDS, family planning and demographic projections. Int J Epidemiol 2010, 39 Suppl 1:i7-10. Bhutta ZA, Ahmed T, Black RE, Cousens S, Dewey K, Giugliani E, Haider BA, Kirkwood B, Morris SS, Sachdev HP et al: What works? Interventions for maternal and child undernutrition and survival. Lancet 2008, 371(9610):417-440. Friberg IK, Bhutta ZA, Darmstadt GL, Bang A, Cousens S, Baqui AH, Kumar V, Walker N, Lawn JE: Comparing modelled predictions of neonatal mortality impacts using LiST with observed results of community-based intervention trials in South Asia. Int J Epidemiol 2010, 39 Suppl 1:i11-20. Bryce J, Boschi-Pinto C, Shibuya K, Black RE: WHO estimates of the causes of death in children. Lancet 2005, 365(9465):1147-1152. Rowe AK, Rowe S, Snow RW, Korenromp E, Armstrong Schellenberg J, Stein C, Nahlen BL, Bryce J, Black RE, Steketee RW: The burden of malaria mortality among African children in the year 2000. International Journal of Epidemiology 2006, 35(3):691-704. Eisele TP, Larsen D, Steketee RW: Protective efficacy of interventions for preventing malaria mortality in children in Plasmodium falciparum endemic areas. Int J Epidemiol 2010, 39(suppl_1):i88-101. Hay SI, Guerra CA, Tatem AJ, Atkinson PM, Snow RW: Urbanization, malaria transmission and disease burden in Africa. Nature reviews 2005, 3(1):81-90. Steketee RW, Eisele TP: Is the scale up of malaria intervention coverage also achieving equity? PLoS ONE 2009, 4(12):e8409. Korenromp EL, Miller J, Cibulskis RE, Kabir Cham M, Alnwick D, Dye C: Monitoring mosquito net coverage for malaria control in Africa: possession vs. use by children under 5 years. Trop Med Int Health 2003, 8(8):693-703. Unicef: Malaria & children: Progress in intervention coverage. In. New York: Unicef and RBM; 2007. Macintyre K, Keating J, Okbaldt YB, Zerom M, Sosler S, Ghebremeskel T, Eisele TP: Rolling out insecticide treated nets in Eritrea: examining the determinants of possession and use in malarious zones during the rainy season. Trop Med Int Health 2006, 11(6):824-833. Kleinschmidt I, Schwabe C, Benavente L, Torrez M, Ridl F, Segura J, Ehmer P, Nchama G: Marked increase in child survival after four years of intensive malaria control. Am J Trop Med Hyg 2009, 80(6):882-888. WHO: World Malaria Report 2005. In.: World Health Organization; 2005. WHO: World Malaria Report 2008. In. Edited by WHO. Geneva: WHO; 2008. U.N.: The World Population Prospect: The 2008 Revision. In. New York: UN Population Division; 2008. 10 Figure legend Figure 1: Countries included in the analysis of the impact of malaria prevention intervention scale-up. Figure 2: Country specific estimates of vector control (ITNs/IRS) coverage in rural areas from 20002010. The blue line is the predicted vector control scale-up. The red line is the scenario of the lowest coverage increase used for lower bound estimate for uncertainty; the green line is the scenario of the highest coverage increase used for the upper bound estimate for uncertainty. Circles represent MICS surveys, diamonds represent DHS surveys, triangles represent MIS surveys, and squares represent other types of household surveys. Figure 3: Country specific estimates of malaria prevention in pregnancy (IPTp/ITNs) coverage in rural areas from 2000-2010. The blue line is the predicted malaria in pregnancy prevention intervention scale-up. The red line is the scenario of the lowest coverage increase used for lower bound estimate for uncertainty; the green line is the scenario of the highest coverage increase used for the upper bound estimate for uncertainty. Circles represent MICS surveys, diamonds represent DHS surveys, triangles represent MIS surveys, and squares represent other types of household surveys. 11 12 Figure 2: Total estimated vector control coverage by year for 36 countries in sub-Saharan Africa, weighted by population size 100 90 80 70 60 50 40 30 20 10 0 Lower bound Estimated ITN coverage 20002001200220032004200520062007200820092010 Upper bound 13 Angola Benin 100 100 80 80 60 60 40 40 27.5 20 1.4 20 0 Burundi 100 100 80 80 60 60 40 50.4 40 15.2 20 3.2 0 20 1.2 8.5 0 Cameroon Central African Republic 100 100 80 80 60 60 40 40 0 4.7 0 Burkina Faso 20 21.4 0.9 1.0 3.5 20 11.2 1.4 0 14 Chad Congo (Brazzaville) 100 100 80 80 60 60 36.5 40 20 40 20 4.7 0 0 Cote d'Ivoire Democratic Republic of the Congo 100 100 80 80 60 60 40 40 20 0 8.0 2.1 2.2 6.3 48.3 20 0 0.2 7.1 15 Equatorial Guinea 100 Eritrea 100 87.0 94.0 80 77.0 60 40 20 20 0 0 Gambia 100 100 80 80 56.2 60 40 20 20 3.1 0.0 21.9 Guinea 100 100 80 80 60 60 37.5 40 0 61.6 0 Ghana 20 94.1 60 40 0 66.8 60 40 Ethiopia 70.7 80 25.8 4.8 40 20 9.3 2.7 0 16 Guinea-Bissau Kenya 100 100 80 80 54.1 60 53.0 0 20 2.9 3.3 Madagascar 100 100 80 80 60 60 51.8 40 20 6.7 0 0 Malawi Mali 100 100 80 80 60.2 60 37.5 40 24.8 60 76.5 48.4 40 20 3.1 0 0 Mauritania Mozambique 100 100 80 80 60 60 40 40 0 56.4 40 20 20 5.8 0 Liberia 20 47.7 40 40 20 60.7 60 0.6 8.5 28.8 20 0 17 Niger Nigeria 100 80.5 80 60 100 80 60 44.2 40 20 78.4 45.0 40 20 3.6 0 7.6 3.1 0 Rwanda Senegal 100 100 80 80 60 69.9 60 53.8 40 40 20 20 38.4 22.2 1.8 11.8 0 0 Sierra Leone Somalia 100 100 80 80 60 60 36.7 40 20 0 4.8 0.9 6.5 40 20 11.0 0 18 Sudan Tanzania 100 100 80 80 60 60 50.6 40 18.4 0 Togo 0.1 Uganda 100 100 80 80 60 60 42.5 40 40 20 20 1.5 47.7 14.0 0 Zambia Zimbabwe 100 100 80 66.3 53.7 60 37.9 40 0 13.8 20 0 20 32.6 40 20 0 63.4 10.9 3.3 72.9 80 60 33.5 40 20 7.2 0 19 Figure 3: Total estimated malaria prevention in pregnancy coverage by year for 31 countries in sub-Saharan Africa, weighted by population size 100 90 80 70 60 50 40 30 20 10 0 Smallest IPTp coverage change Estimated IPTp coverage Largest IPTp coverage change 20002001200220032004200520062007200820092010 20 Angola Benin 100 100 80 80 60 60 40 26.4 40 20 20 0 0 Burkina Faso Cameroon 100 100 80 80 60 60 40 40 20 0.3 20 0 8.9 0 Central African Republic Chad 100 100 80 80 60 60 40 40 20 20 0 2.3 4.7 17.7 0 21 Congo (Brazzaville) Cote d’Ivoire 100 100 80 80 60 60 40 40 20 20 3.2 0 0 Democratic Republic of the Congo Equatorial Guinea 100 100 80 80 60 42.5 60 40 40 20 20 4.4 0 19.0 0 Gambia Ghana 100 100 80 67.2 80 60 60 40 7.2 33.8 40 20 20 0 0 26.1 0.9 22 Guinea Guinea-Bissau 100 100 80 80 60 60 40 40 20 1.2 0 20 3.3 Liberia 100 100 80 80 48.3 60 60 44.8 40 40 12.8 4.4 0 20 4.3 0 Madagascar Malawi 100 100 80 80 60 7.1 0 Kenya 20 29.3 45.6 60 40 40 28.3 20 20 0 0 50.7 42.5 45.7 23 Mali Mozambique 100 100 80 80 60 41.9 40 40 20 60 16.1 20 5.6 0 0 Niger Nigeria 100 71.3 80 100 80 60 60 40 40 20 20 4.9 0 0 40.8 0.2 3.7 Senegal 100 80 60 46.5 54.2 40 20 ] 10.0 0 24 Sierra Leone Somalia 100 100 80 80 60 60 40 20 29.3 40 20 1.1 0.7 0 0 Sudan Tanzania 100 100 80 80 60 60 31.6 40 59.2 27.9 40 21.7 20 20 0 0 Togo Uganda 100 100 80 80 60 60 40 40 20 0 18.5 20 43.5 16.2 0 25 Zambia Zimbabwe 100 100 80 60 59.1 58.1 52.5 65.2 80 60 40 40 20 20 0 0 7.4 26 Table 1: Vector control coverage estimates from household surveys 27 Country Year Angola Angola Benin Benin Burkina Faso Burkina Faso Burundi Burundi Burundi Cameroon Cameroon Cameroon CAR CAR Chad Chad Congo (Brazzaville) Cote d’Ivoire Cote d’Ivoire Cote d’Ivoire DRC DRC DRC Equatorial Guinea4 Equatorial Guinea4 Equatorial Guinea4 Eritrea Eritrea Ethiopia Ethiopia Ethiopia Gambia Gambia Gambia5 Ghana Ghana Ghana Guinea Guinea Guinea-Bissau Guinea-Bissau Guinea-Bissau Kenya Kenya Kenya5 Kenya Liberia Liberia Madagascar Malawi Malawi Malawi Malawi Mali Mali Mauritania Mauritania Mozambique5 Niger Niger 2001 2006 2001 2006 2003 2006 2001 2005 2010 2000 2004 2006 2000 2006 2004 2010 2005 2000 2005 2006 2001 2007 2010 2005 2006 2008 2003 2008 2000 2005 2007 2000 2006 2010 2003 2006 2008 2005 2007 2000 2006 2010 2000 2003 2007 2009 2005 2009 2008 2000 2004 2006 2010 2006 2010 2003 2007 2007 2000 2006 Rural HH estimate 1.41 25.9 4.71 21.4 3.2 15.2 1.21 8.5 50.4 0.9 1 1.0 3.5 1.41 11.2 20.73 36.5 2.1 2.11 2.2 6.3 0.21 7.1 48.3 87.0 77.0 94.0 66.8 70.7 0.0 3.1 56.2 21.91 61.6 94.1 4.8 25.8 37.5 2.7 9.3 2.91 54.1 53.0 3.31 5.8 47.7 55.0 6.7 51.8 56.4 3.11 24.8 37.5 60.2 48.4 76.5 0.6 8.5 28.8 3.61 44.2 Sample Size 1968 1500 3185 10279 6898 5010 3325 7020 7817 2071 5616 4808 8963 7628 4295 9987 2028 4919 2473 4348 6559 5188 7014 1274 2142 2478 2341 1530 14072 10055 6154 2300 3230 4335 3733 3822 6603 4562 1669 3571 3071 6059 1439 5662 5929 6147 6337 2278 13364 2528 11939 27711 1091 8859 9400 2218 6393 2740 3227 5298 Rural HH standard error 0.5 3.5 0.72 0.8 0.4 0.6 0.42 0.3 0.42 0.42 0.2 0.3 0.22 0.72 1.52 1.08 0.3 0.42 0.5 0.5 0.12 1.0 2.0 2.0 1.5 1.0 3.0 2.32 0.52 0.6 1.32 1.72 0.9 0.9 0.6 0.8 1.2 0.3 0.7 0.62 0.9 1.1 0.92 0.6 1.42 1.8 0.62 3.2 1.0 0.72 0.8 0.4 3.02 1.5 0.92 0.32 0.4 2.12 0.72 1.5 95% confidence interval 0.4 – 2.4 19.0 – 32.7 3.2 – 6.2 20.0 – 22.9 2.4 – 4.1 14.1 – 16.4 0.5 – 2.0 7.8 – 9.1 48.2 – 52.6 0.1 – 1.7 0.6 – 1.5 2.9 – 4.1 0.9 – 1.8 9.8 – 12.6 17.7 – 23.7 34.4 – 38.7 1.5 – 2.6 1.3 – 2.9 1.3 – 3.1 5.3 – 7.4 0.0 – 0.4 5.2 – 9.0 44.3 – 52.3 80.0 – 91.0 74.0 – 80.0 92.0 – 95.0 60.9 – 72.7 66.1 – 75.3 0 – 0.9 1.9 – 4.2 53.7 – 58.7 18.5 – 25.3 59.9 – 63.3 92.3 – 96.0 3.5 – 6.1 24.3 – 27.4 35.2 – 39.9 2.1 – 3.3 7.9 – 10.8 1.8 – 4.0 52.3 – 56.0 50.7 – 55.2 1.5 – 5.2 4.6 – 7.0 45.0 – 50.4 51.5 – 58.5 5.5 – 7.9 45.4 – 58.2 54.5 – 58.4 1.7 – 4.4 23.2 – 26.5 36.8 – 38.3 54.4 – 66.0 45.3 – 51.4 74.8 – 78.2 0.0 – 1.2 7.8 – 9.3 24.6 – 33.0 2.3 – 4.9 41.1 – 47.2 Survey MICS MIS DHS DHS DHS MICS MICS MICS DHS MICS DHS MICS MICS MICS DHS MICS DHS MICS DHS MICS MICS DHS MICS [17] [17] [17] [16] MIS DHS DHS MIS MICS MICS MICS DHS MICS DHS DHS ONS MICS MICS MICS MICS DHS MIS DHS MIS MIS DHS DHS DHS MICS MIS DHS MICS DHS MICS MIS MICS DHS 28 Niger Niger Nigeria Nigeria Nigeria Rwanda Rwanda Rwanda Senegal Senegal Senegal Senegal Sierra Leone Sierra Leone Sierra Leone Somalia Sudan Sudan (Southern) Tanzania Tanzania Tanzania Tanzania Togo Togo Uganda Uganda Uganda Zambia Zambia Zambia5 Zambia Zambia5 Zambia5 Zimbabwe Zimbabwe 2009 20107 2003 2008 2010 2000 2005 2007 2000 2005 2006 2008 2000 2005 2008 2006 2006 2009 1999 2004 2007 2010 2000 2006 2000 2006 2009 2000 2001 2006 2007 2008 2010 2005 2009 80.5 78.4 3.1 7.6 45.0 1.81 11.8 53.8 4.81 22.2 38.4 69.9 0.91 6.5 36.7 11.0 18.46 50.6 0.1 13.8 32.6 63.4 1.51 42.5 0.31 14.0 47.7 3.31 10.9 37.9 53.7 66.3 72.9 7.2 28.2 10652 6450 4291 23346 4175 2410 8165 6229 6500 4296 1807 6304 1961 2375 4328 3768 24036 2316 2669 7576 6662 7414 2411 4312 6793 7480 3761 2896 5112 1786 4469 2882 2766 6229 7420 0.8 0.82 0.6 0.4 1.5 0.52 0.7 1.32 0.52 1.1 2.3 1.6 0.4 0.5 1.5 0.5 0.52 2.12 0.12 1.0 1.2 1.1 0.52 0.9 0.72 0.9 2.2 0.72 0.9 3.0 1.8 2.7 1.72 0.8 1.0 79.0 – 82.0 76.4 – 80.4 1.9 – 4.2 6.8 – 8.5 42.0 – 48.0 0.7 – 2.9 10.5 – 13.1 51.3 – 56.3 3.8 – 5.8 20.1 – 24.3 33.9 – 43.0 66.7 – 73.0 0.0 – 1.7 5.4 – 7.5 33.7 – 39.7 10.0 – 12.1 17.4 – 19.4 46.5 – 54.7 0.0 – 0.4 11.8 – 15.8 30.2 – 35.0 6.2 – 65.6 0.5 – 2.4 40.8 – 44.2 0 – 1.7 12.2 – 15.9 43.3 – 52.1 2.0 – 4.6 9.2 – 12.6 32.1 – 43.7 50.1 – 57.3 60.9 – 71.7 69.6 – 76.2 5.6 – 8.7 26.2 – 30.2 ONS ONS DHS DHS MIS MICS DHS MIS MICS DHS MIS MIS MICS MICS DHS MICS ONS MIS DHS DHS AIS DHS MICS MICS DHS DHS MIS MICS DHS MIS DHS MIS MIS DHS DHS Vector control: Houses protected by either ITNs and/or IRS CAR: Central African Republic DRC: Democratic republic of Congo 1. These estimates are derived from the ratio of children sleeping under an ITN the night before 2. These standard errors are estimated using Formula 1 3. Estimate was derived using the ratio of mosquito nets to ITNs of Burkina Faso 2003 4. Data available were only for Bioko Island 5. Estimated with households protected by either ITNs or IRS; all others just use ITN household possession 6. Estimate is total country, not specific to rural 7. Estimated using ratio of total ITN coverage to rural ITN coverage from previous year 29 Table 2: Model-derived estimates of proportion of households with ≥1 ITN, estimated from cumulative ITN procured model 1 (Table 1). These estimates are not used directly in the LiST analysis; they are only used to derive the percent increase in ITN coverage between survey rounds 2004-2008. Country Angola Benin Burkina Faso Burundi Cameroon CAR Chad Congo Cote d’Ivoire DRC Ethiopia Gambia Ghana Guinea Guinea-Bissau Kenya Liberia Madagascar Malawi Mali Mauritania Mozambique Namibia Niger Nigeria Rwanda Senegal Sierra Leone Somalia Sudan Tanzania Togo Uganda Zambia Zimbabwe 2004 11 8 9 12 4 10 8 8 5 3 5 11 5 9 12 6 11 10 9 9 9 7 0 9 0 11 10 11 11 4 13 16 16 8 9 2005 16 13 14 17 8 14 13 12 9 8 10 15 10 13 18 11 16 15 23 13 15 20 1 14 0 26 26 16 16 9 18 27 20 13 14 2006 26 26 21 25 12 19 18 17 14 14 27 23 24 20 22 30 34 34 27 29 19 27 10 39 0 34 33 22 25 15 22 32 26 33 18 2007 41 33 27 40 17 26 23 25 21 20 44 30 39 30 39 54 50 43 33 43 25 33 20 44 0 55 44 56 33 22 26 38 37 43 24 2008 55 57 36 48 21 39 29 31 28 28 49 49 46 36 42 60 70 58 43 75 28 43 44 49 1 63 63 62 39 35 31 31 45 68 30 CAR: Central African Republic DRC: Democratic republic of Congo 30 Table 3: malaria in pregnancy intervention coverage estimates from household surveys 2000-2010 Country Year Angola Benin Burkina Faso Cameroon CAR Chad Congo (Brazzaville) Cote d’Ivoire DRC DRC Equatorial Guinea4 Gambia Ghana Gambia Ghana Ghana Guinea Guinea Guinea-Bissau Guinea-Bissau Kenya Kenya Liberia Liberia Malawi Malawi Malawi Malawi Mali Mali Mozambique Niger Niger Nigeria Nigeria Nigeria Senegal Senegal Senegal Sierra Leone Sierra Leone Somalia Sudan (Southern) Tanzania Tanzania Tanzania Togo Uganda Uganda Zambia Zambia Zambia Zambia 2006 2006 2006 2006 2006 2010 2005 2006 2007 2010 2008 2006 2003 2010 2006 2008 2005 2007 2006 2010 2003 2007 2005 2009 2000 2004 2006 2010 2006 2010 2007 2006 2010 2003 2008 2010 2005 2006 2008 2005 2008 2006 2009 2004 2007 2010 2006 2006 2009 2006 2007 2008 2010 Rural HH estimate 26.41 2.31 0.3 8.9 4.7 17.7 3.23 7.2 4.4 42.51 19.0 33.8 0.9 67.2 26.1 43.5 1.2 3.3 7.1 29.31 4.4 12.8 4.33 44.8 28.3 42.53 45.7 50.7 5.61 41.9 16.1 4.9 71.31 0.2 3.7 38.7 10.0 46.5 54.2 1.1 29.31 0.7 31.6 18.6 27.9 59.21 18.5 16.2 43.61 52.5 59.1 58.1 65.2 Sample Size 269 1962 156 685 2510 1616 933 2258 2130 1024 503 2052 1076 2760 944 811 2122 1669 531 540 1802 1644 510 1009 4180 4246 9279 213 1896 1986 1016 1311 91989 1544 8311 586 3126 1352 4450 103 238 1426 421 1908 2550 788 1213 2956 368 1030 1830 1658 1595 Rural HH standard error 1.6 0.2 0.2 1.3 0.62 1.2 0.92 0.7 0.8 2.6 2.6 1.1 0.3 1.2 1.6 2.5 0.3 0.92 0.7 2.5 0.6 1.02 1.02 2.9 0.9 1.0 0.7 6.92 0.5 2.2 1.32 0.3 0.72 0.1 0.3 4.0 0.8 2.3 1.4 1.02 1.3 0.2 4.52 1.0 1.5 2.5 1.3 0.9 4.0 1.9 1.8 1.7 2.4 95% confidence interval 23.3 – 29.5 1.9 – 2.7 0.0 – 0.7 6.4 – 11.5 3.5 – 5.9 15.4 – 20.0 1.5 – 4.9 5.9 – 8.5 2.9 – 5.9 37.2 – 47.7 16.0 – 24.0 31.8 – 35.9 0.3 – 1.5 64.8 – 69.6 22.9 – 29.3 38.6 – 48.3 0.7 – 1.7 1.6 – 5.0 5.8 – 8.4 24.3 – 34.3 3.3 – 5.5 10.4 – 14.4 10.4 – 14.4 39.0 – 50.5 26.6 – 30.0 40.5 – 44.4 44.3 – 47.1 37.3 – 64.1 4.5 – 6.6 37.6 – 46.2 13.6 – 18.6 4.4 – 5.4 70.6 – 71.9 0.0 – 0.4 3.1 – 4.3 30.8 – 46.6 8.4 – 11.7 41.9 – 51.1 51.3 – 57.0 0.0 – 3.0 26.8 – 31.8 0.3 – 1.1 22.7 – 40.5 16.6 – 20.7 25.0 – 30.8 54.3 – 64.0 15.9 – 21.1 14.4 – 18.0 36.0 – 51.6 48.6 – 56.3 55.5 – 62.7 54.7 – 61.5 60.5 – 69.9 Survey MIS DHS MICS MICS MICS MICS DHS MICS DHS MICS [17] MICS DHS MICS MICS DHS DHS ONS MICS MICS DHS MIS MIS MIS DHS DHS MICS MIS DHS MICS MIS DHS ONS DHS DHS MIS DHS MIS MIS MICS DHS MICS MIS DHS AIS MIS MICS DHS MIS MIS DHS MIS MIS 31 Zimbabwe 2005 7.4 1642 1.0 5.5 – 9.4 DHS Malaria in pregnancy interventions: IPTp or ITNs, whichever is higher CAR: Central African Republic DRC: Democratic republic of Congo 1. These estimates are pregnant women sleeping under an ITN the night before the survey; all others are IPTp received among women giving birth in the past 2 years 2. These standard errors are estimated using formula 1 3. These estimates were not specified as 2+ doses of SP received at ANC 4. Data available were only for Bioko Island 32 Table 4: Estimated malaria deaths in children 1-59 months prevented by vector control scale-up 2001-2010 Uncertainty Country Malaria deaths 2000 2001 2002 2003 2004 2005 2006 2007 2008 2009 2010 Angola 13,991 3 274 565 937 1,443 2,502 4,182 5,967 6,732 7,543 Benin 10,759 6 57 110 166 423 1,220 1,625 3,162 3,502 Burkina Faso 20,089 58 118 178 628 1,163 1,885 2,601 3,767 4,284 1 38 77 118 189 294 510 21,332 4 8 12 11 171 350 537 CAR 5,488 34 70 106 142 225 318 466 712 770 Chad 18,594 75 155 242 332 634 1,012 1,417 1,903 3,272 4,863 21 43 66 90 185 290 443 566 610 Cote d’Ivoire 19,210 0 0 0 0 16 504 878 1,271 DRC 78,901 0 319 655 1,054 1,761 2,593 3,502 267 0 0 0 0 143 129 1,705 231 463 712 752 783 Ethiopia 20,658 70 143 218 294 Gambia 2,101 20 41 62 Ghana 26,873 151 305 464 Guinea 16,687 21 33 55 2,130 84 172 265 Kenya 20,761 113 225 344 Liberia 4,583 23 46 Madagascar 14,235 153 Malawi 10,545 Mali Burundi Cameroon Congo (Brazzaville) Equatorial Guinea (Bioko Island) Eritrea Guinea-Bissau Mauritania Mozambique Total Lower Bound Upper Bound 30,148 20,103 42,128 3,841 14,112 9,425 19,801 4,496 5,247 20,141 13,955 27,758 634 1,024 1,428 4,313 3,166 5,574 730 815 883 3,521 1,365 6,640 831 3,674 2,458 5,147 4,692 13,734 8,006 21,165 658 2,972 987 5,321 1,374 1,494 5,537 3,076 8,856 4,595 14,970 25,721 55,170 37,543 76,542 148 167 171 175 934 677 1,185 811 839 861 891 918 7,261 141 8,634 379 4,177 7,125 7,915 9,102 10,326 39,749 30,087 48,133 85 253 589 866 1,128 1,162 1,198 5,404 3,726 7,353 590 1,394 3,922 4,976 6,025 7,254 8,490 33,571 22,972 46,327 67 91 225 772 964 1,333 1,712 5,273 2,992 8,289 359 546 698 708 718 727 734 5,011 3,675 6,454 367 872 3,353 6,387 7,124 7,868 8,906 35,559 25,662 48,200 70 96 143 252 358 490 1,588 1,983 5,049 2,696 7,533 311 464 629 1,078 2,644 3,517 4,790 5,392 5,995 24,973 16,122 33,510 330 676 1,036 1,408 1,851 2,319 2,918 3,922 4,046 4,170 22,676 16,550 29,536 22,029 405 831 1,292 1,764 2,899 6,653 10,425 11,255 11,544 11,821 58,889 42,160 76,497 1,212 0 0 0 20 33 45 60 72 88 105 423 233 606 31,019 187 381 579 775 3,031 4,140 5,285 7,055 7,948 8,893 38,274 20,436 55,421 33 Niger 13,840 138 290 455 642 1,154 4,110 4,938 5,739 8,825 8,876 35,167 25,199 46,139 334,546 823 1,672 2,541 2,663 2,784 2,903 4,075 12,805 53,745 95,587 179,598 116,497 258,931 Rwanda 1,997 10 20 31 43 135 442 744 874 1,008 1,142 4,449 3,615 5,729 Senegal 12,006 64 132 202 276 1,328 2,623 3,655 5,315 6,091 6,868 26,554 18,579 35,766 Sierra Leone 8,289 43 88 136 189 299 658 1,783 2,036 2,347 2,676 10,255 7,080 14,074 Somalia 2,273 11 23 35 48 78 137 197 242 272 303 1,346 928 1,796 Sudan 35,621 161 324 488 647 1,728 3,376 5,087 8,247 10,145 12,439 42,642 30,245 57,163 Tanzania 41,517 826 1,672 2,560 3,492 4,689 6,112 9,000 10,867 14,902 19,184 73,304 54,025 93,550 5,627 161 327 499 675 1,173 1,405 1,697 1,715 1,978 2,252 11,882 8,692 15,427 Uganda 43,518 518 1,065 1,619 2,231 2,963 3,906 5,870 7,404 14,724 16,620 56,920 37,793 75,542 Zambia 14,517 641 661 678 694 1,104 3,174 4,685 5,966 5,995 6,787 30,385 21,884 42,498 Nigeria Togo Zimbabwe Total 151 1 1 2 2 4 6 9 12 22 27 86 39 150 886,218 5,386 10,982 16,815 22,283 37,141 69,772 102,278 137,007 216,722 290,509 908,896 612,789 1,243,375 Vector control: Houses protected by either ITNs and/or IRS CAR: Central African Republic DRC: Democratic Republic of Congo 34 Table 5: Child deaths prevented due to scale-up of malaria prevention in pregnancy across sub-Saharan Africa Uncertainty Angola Neonatal deaths in 2000 35,765 11 22 34 47 61 75 90 106 124 143 713 395 961 Benin 9,942 0 1 1 1 2 2 2 3 3 4 19 9 25 Burkina Faso 19,352 0 0 0 0 0 1 1 2 2 3 9 3 30 Cameroon 17,463 0 0 0 3 8 12 17 22 27 32 121 61 188 CAR 7,450 0 0 0 1 2 4 5 6 8 9 35 19 53 Chad 18,779 0 0 0 3 7 11 15 20 25 30 111 73 148 Congo (Brazzaville) 3,496 0 0 0 0 1 1 2 2 3 4 13 2 27 Cote d’Ivoire 25,092 0 0 0 0 9 18 29 39 51 62 208 111 317 DRC Equatorial Guinea (Bioko Island) Gambia 123,220 0 0 0 6 14 21 29 110 201 297 678 411 952 1,169 0 0 0 0 0 0 1 1 1 1 4 2 8 2,503 0 1 3 4 5 7 9 10 13 15 67 43 85 Ghana 22,418 0 0 1 14 27 41 56 72 89 106 406 248 558 Guinea 14,667 0 0 0 0 1 3 4 6 8 9 31 9 58 Guinea-Bissau 2,524 0 0 0 0 1 3 5 7 9 12 37 22 52 Kenya 32,642 2 3 5 7 10 12 15 38 61 72 225 122 324 Liberia 5,919 1 1 2 3 4 11 20 30 40 51 163 90 231 Madagascar 18,524 14 28 35 47 59 72 84 97 111 125 672 355 911 Malawi 13,359 7 14 24 31 36 42 47 53 56 61 371 192 634 Mali 32,298 4 8 12 17 22 27 70 116 167 221 664 378 906 Mozambique 49,257 0 0 0 0 0 1 1 1 1 1 615 355 898 Niger 19,853 2 4 7 9 12 15 67 126 191 263 696 446 900 Nigeria 188,,910 0 2 4 16 30 46 64 83 435 847 1,527 792 2,169 Senegal 14,455 0 0 0 6 12 57 65 73 95 118 426 0 559 Sierra Leone 11,971 0 0 0 0 1 1 2 3 4 6 17 276 485 Somalia 15,567 0 0 0 0 1 1 2 3 4 5 16 219 34 Sudan 48,404 17 33 51 68 87 105 124 143 163 183 974 7 1,255 Tanzania 39,691 14 29 47 50 60 71 82 116 151 189 809 478 1,067 Country 2001 2002 2003 2004 2005 2006 2007 2008 2009 2010 Total Lower Bound Upper Bound 35 Togo 7,537 0 0 0 0 4 9 14 19 24 29 99 56 147 Uganda 33,991 6 12 19 27 35 45 72 102 134 155 607 332 883 Zambia 14,584 20 40 64 88 113 140 163 168 184 198 1,178 714 1,495 Zimbabwe 9,043 0 0 0 1 2 3 4 5 6 7 28 15 46 Total 875,200 98 198 309 449 626 896 1,240 1,703 2,555 3,465 11,539 6,425 14,635 Malaria prevention in pregnancy: Woman received IPTp during last 2 pregnancies or currently pregnant women used ITNs previous night CAR: Central African Republic DRC: Democratic Republic of Congo Countries without stable malaria transmission or a policy of IPTp were excluded 36