Board Review: Cardiac testing Arrhythmias
advertisement

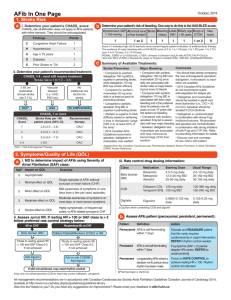
Board Review: Arrhythmias Katie Bever August 20, 2013 Overview of Arrhythmias • • • • • • Diagnostic testing Review of bradycardias Review of tachycardias Antiarrhythmic agents Cardiac devices Questions! Diagnostic testing • Resting ECG (if you’re lucky!) • Continuous ambulatory ECG (24-48hrs) • Event recorders: triggered by patient o Looping recorder o Postsymptom recorder • Implantable loop recorder (up to 3 years battery life) • • • • Others to consider: TTE to evaluate for structure heart disease Ischemia evaluation if life-threatening arrhythmia EP testing to provoke arrhythmia and potentially ablate Overview of Bradycardia • 2/2 disorders of impulse generation (impaired automaticity) or impulse conduction (heart block) • Reversible causes include Lyme disease, drugs, hyperkalemia and thyroid disease • Symptoms: syncope, LH, fatigue, dyspnea, exerciseintolerance, ventricular arrhythmias • Evaluation includes documentation of bradycardia with symptoms • Management includes atropine/transcutaneous pacing if unstable, treatment of reversible causes, PPM Impaired automaticity • Sinus brady not necessarily pathologic (i.e. athletes) • Causes of pathologic sinus bradycardia o o o o o o Sick sinus syndrome/SA node dysfunction Infarction or cardiac surgery Infiltrative processes (amyloidosis, sarcoidosis) Increased vagal tone (Valsalva, vomiting) Medications (ie BB, CCB) Genetic diseases • Pacemaker is indicated for symptomatic sinus bradycardia Heart Block • 1st degree and 2nd degree Mobitz 1 block usually 2/2 disease within the AV node • 2nd degree Mobitz 2 and 3rd degree block usually His bundle or below • 1st degree block associated with increased risk afib, pacemaker implantation and all-cause mortality • “Advanced” or “high-grade” 2nd degree heart block if 2+ nonconducted P’s before each QRS • Pacemaker indicated for advanced 2nd degree or 3rd degree AV block (CHB) • Reversible causes of CHB include medications and Lyme disease Overview of tachycardia • Narrow complex tachycardias o Atrial fibrillation/atrial flutter o Supraventricular tachycardias • Wide complex tachycardias o SVT with aberrancy o Ventricular arrhythmias Acute management of afib • Immediate synchronized cardioversion if hypotension, angina or heart failure • If HD stable, goal HR 60-110/min with BB, CCB or digoxin • Consider elective cardioversion: o If duration afib<48hrs, can proceed with DCCV o If duration >48hrs or unknown: anticoagulate for 3+ weeks prior to DCCV, or anticoagulate then TEE to rule out intracardiac thrombus prior to DCCV o Anticoagulation must continue after cardioversion for 4 weeks Long-term management of afib • Increased risk of embolic stroke, heart failure and all-cause mortality • Anticoagulation based on risk factors (ie CHADS2, rheumatic MS, or mechanical heart valve) o o o Warfarin > aspirin + plavix > aspirin alone Direct thrombin inhibitors (ie dabigatran) Rivaroxaban (oral factor Xa inhibitor) • Rate control • Rhythm control if symptoms despite adequate rate control o Consider “pill-in-the-pocket” approach with flecainide or propafenone for symptomatic paroxysmal afib (remember to rate control as well!) • Ablation, esp if aflutter • AV nodal ablation • Maze surgery Supraventricular tachycardias • AVNRT – fast and slow pathways within AV node • AVRT – circuit includes AV node and bypass tract o o Anterograde conduction leads to preexcitation: short PR interval, delta wave (WPW) Retrograde conduction -> concealed bypass tract • Atrial tachycardia – ectopic focus or area of micro-reentry • Management includes AV nodal blocking agents, antiarrhythmics or catheter ablation • EXCEPTION!: do not give AV nodal blockers to pts with WPW syndrome and afib -> procainamide or amio are preferred Ventricular Arrhythmias • Premature ventricular contractions o o o o Present in up to 75% of healthy persons More common in persons with HTN or structural heart disease Tx symptoms with B-blocker or CCB Antiarrhythmics or ablation if refractory symptoms • Ventricular tachycardia o o o o o Increased risk of SCD in patients with structural heart disease Idiopathic VT carries better prognosis B-blockers for patients with HF or ischemic heart disease ICD for primary or secondary prevention Antiarrhythmics may reduce frequency of shocks but not mortality • Inherited arrhythmia syndromes o o o o Long QT syndrome -> torsades Short QT syndrome -> afib, VT/VF, SCD Brugada syndrome -> VF, SCD Catecholaminergic polymorphic VT -> polymorphic or bidirectional VT during exercise/stress, SCD o ARVC -> epsilon waves, monomorphic VT Antiarrhythmic Medications VaughanWilliams Classification Mechanism of Action Examples Effect Use Class IA Na-channel blockade, some Kchannel blockade Quinidine, procainamide, disopyramide Slows conduction, prolongs repolarization Preexcited afib, SVT, ventricular arrhythmias Class IB Na-channel blockade Lidocaine, mexiletine, phenytoin Slows conduction in diseased tissures, shortens repolarization Ventricular arrhythmias Class IC Na-channel blockade Flecainide, propafenone Markedly slows conduction, slightly prolongs repol Afib, aflutter, SVT, ventricular arrhythmias Class II Beta blockade Metoprolol, propranolol, Suppresses automaticity and slows AV nodal conduction Rate control of arrhythmias, SVT, ventricular arrhythmias Class III Potassium channel blockade Sotalol, amio, dofetilide, dronedarone Prolongs action potential duration Afib, aflutter, ventricular arrhythmias Class IV Calcium channel blockade Verapamil, diltiazem Slows SA node automaticity and AV nodal conduction SVT, rate control of atrial arrhythmias, triggered arrhythmias A1 receptor agonist Adenosine Slows or blocks SA node automaticity and AV node condunction Termination of SVT Increasing vagal activity Digoxin Slows AV nodal conduction Rate control of arrhythmias Indications for PPM • Symptomatic bradycardia (HR<40/min) or sinus pauses • Symptomatic CHB or 2nd degree heart block (type 1 or 2) • Asymptomatic CHB or advanced 2nd degree HB • Afib with pauses >= 5 seconds • Alternating bundle branch block • After catheter AV nodal ablation Overview of ICD • Indicated for primary and secondary prevention • Management perioperatively: shock function should be turned off during procedures using electrocautery • Management of device infection: removal of entire system Question 1 76yo F is evaluated in ED for dizziness, SOB, and palpitations that began acutely 1 hr ago. She has a hx of HTN and HFPEF. Medications are HCTZ, lisinopril, and aspirin. On exam, she is afebrile, BP 80/60, pulse 155/min, and respiration rate is 30/min. O2 sat is 80% with 40% oxygen by face mask. Cardiac auscultation reveals irregularly irregular rhythm, tachycardia, and some variability in S1 intensity. Crackles are heard bilaterally one-third up in the lower lung fields. ECG demonstrates afib with RVR. Which one of the following is the most appropriate acute treatment? (A) Adenosine (B) Amiodarone (C) Cardioversion (D) Diltiazem (E) Metoprolol Answer: cardioversion The patient is hemodynamically unstable and should undergo immediate cardioversion. She has hypotension and pulmonary edema in s/o rapid afib. In patients with HFPEF, the loss of atrial “kick” with afib can sometimes lead to severe symptoms. The best treatment in this situation is immediate cardioversion to convert the patient to normal sinus rhythm. Although there is a risk of thromboembolic event since she is not anticoagulated, she is currently in extremis and is at risk of imminent demise if not agressively treated. Adenosine is useful for diagnosing an SVT and can treat AV nodedependent tachycardiacs, but is not useful in the treatment of afib. Amio can convert afib to NSR as well as provide rate control, but immediate treatment is needed and amio may take several hours. Oral amio may be a reasonable long-term option given the severity of her symptoms. Metoprolol and dilt would slow her heart rate; however, she is hypotensive and these medications could make her BP lower. In addition, she is in active heart failure. Question 2 75yo M w/HTN is evaluated during his 1st outpatient visit after an acute MI. He is now asymptomatic and reports no CP or symptoms of heart failure since discharge. He had a lateral infarction, and a DES was placed in the left cx artery. He had two episodes of symptomatic afib during hospitalization associated with presyncope and a rhythm control approach was chosen; his LVEF was normal. His medications at the time of discharge were metoprolol, aspirin, dronedarone, clopidogrel, warfarin and atorvastatin. On exam, he is afebrile, BP is 130/78, pulse 68/min and regular, RR 12/min. There is an S4 but the remainder of the cardiac exam is normal. Lungs are clear and there is no peripheral edema. Labs are normal except for a serum creatinine of 1.5. Which of the following meds is most likely to have caused the increase in serum creatinine level? (A) Atorvastatin (B) Clopidogrel (C) Dronedarone (D) Metoprolol Answer: dronedarone Dronedarone is the newest antiarrhythmic approved for treatment of afib or flutter and has been shown to reduce combined endpoint of hospitalizations and mortality. It is chemically related to amiodarone, has an improved safety profile, but causes an average decrease in creatinine clearance of 18% compared with baseline; up to 5% of patients will have a significant increase in creatinine level. This is due to partial inhibition of tubular transport of creatinine (no change in GFR). Dronedarone has black box warning for patients with heart failure; it is contraindicated in those with NYHA class IV or class II-III with recent decompensation. Question 3 56yo M is evaluated in the hospital for paroxysmal afib. The patient develops increasing SOB during these episodes. 5 days ago, he was admitted for an acute MI and cardiogenic shock and received a DES in the LAD. Medications are lisinopril, digoxin, furosemide, aspirin, clopidogrel, eplerenone, simvastatin, and unfractionated heparin. On exam, the patient is afebrile, blood 92/65, pulse 75. O2 sat is 95% with 3L NC. Cardiac exam reveals estimated CVP of 12cm H2O. Heart sounds are distant and regular. There is a grade 2/6 holosystolic murmur at the cardiac apex. A summation gallop is present. Crackles are ausculated bilaterally in the lower lung fields. Transthoracic echocardiogram shows LVEF 32%. Which of the following is the most appropriate treatment for this pt’s afib? (A) Amiodarone (B) Disopyramide (C) Dronedarone (D) Flecainide (E) Sotalol Answer: amiodarone Amiodarone is the best option for managing symptomatic afib in the setting of heart failure. Patients with heart failure and MI are at increased risk for development of afib. Although amio has may extracardiac side effects, it is most effective agent for preventing afib recurrences, and it is one of the few agents proved safe in patients with heart failure, LVH, CAD, or previous MI. In addition, amio has B-blocking properties that can help with rate control. Disopyramide has negative inotropic effects, which can be detrimental to someone with reduced LVEF and heart failure. Dronedarone increases mortality in pts with NYHA class IV or class II-III HF with recent decompensation. Flecainide is contraindicated after MI because of increased risk polymorphic VT. Like amio, sotalol is class III antiarrhythmic but because of more potent B-blocking effects, it should not be used in acute heart failure. Question 4 61yo M is evaluated during follow up exam. He has a 4 year hx of afib and underwent afib ablation 6 mos ago. He has had no symptoms of palpitations, fatigue, SOB, or presyncope since the procedure. He has HTN and DM2. Medications are lisinopril, atenolol, metformin, and warfarin. BP is 124/82 and pulse 72/min. Cardiac exam discloses regular rate and rhythm. The rest of the exam is normal. ECG demonstrated NSR. Which of the following is the most appropriate treatment? (A)Continue warfarin (B)Switch aspirin (C)Switch to clopidogrel (D)Switch to aspirin and clopidogrel Answer: continue warfarin For the first 2-3 months after afib ablation, all patients should take warfarin. Thereafter, anticoagulation should proceed as if ablation did not occur (i.e. based on CHADS2 score). Switching to aspirin or clopidogrel does not provide the same protective benefit, and it is not appropriate to discontinue all anticoagulation. If CHADS2 score is 0, aspirin alone is preferred. If CHADS2 score is 1, aspirin or warfarin is acceptable. If CHADS2 score is >1 and patient cannot take warfarin, aspirin+clopidogrel is better than aspirin alone. Question 5 38yo F is evaluated during a follow-up visit for 2 syncopal episodes experienced in the past 2 years. The 1st episode occurred 18 months ago at rest. The 2nd episode occurred 5 months ago while she was walking. The patient describes an “uneasy” sensation preceding the events, but reports no dyspnea, chest discomfort, palpitations, or loss of bowl or bladder control. A looping event recorder worn for 30 days did not reveal arrhythmia. She is employed as a school bus driver. She takes no meds. On exam, she is afebrile, BP 120/60, pulse rate is 60/min and regular. The remainder of the exam is normal. Baseline ECG is normal. Which of the following is the most appropriate testing option? (A) Continuous ambulatory ECG monitor (B) Implantable loop recorder (C) Postsymptom event recorder (D) No further testing Answer: implantable loop recorder (ILR) Significant concern for arrhythmia given previous syncopal events and occupation. ILR is placed subcutaneously under local anesthesia and is capable of storing up to 42 minutes of ECG rhythm. Battery life is approx 3 years, likely long enough to capture an event in this patient. Continuous ambulatory ECG may detect asymptomatic arrhythmias but only worn for 24-48hrs. External event recorders are used for more infrequent symptoms and record ECG tracings only when triggered by the patient. No further testing would not be appropriate in this patient with high-risk occupation and has experienced syncope at rest. Question 6 60yo M w/paroxysmal afib is scheduled to undergo screening colonoscopy. Warfarin must be discontinued in case a biopsy is needed. When the patient is in afib, he is asymptomatic. He also has HTN and DM2. He has never had a stroke, TIA or VTE. Medications are metoprolol, metformin, and warfarin. On exam, pulse is 65/min. Other vitals signs are normal. Cardiac rhythm is irregularly irregular. Labs reveal an INR of 2.3. In addition to discontinuing warfarin, which of the following is the most appropriate treatment? (A)Switch to aspirin (B)Switch to clopidogrel (C)Switch to IV UFH (D)Switch to therapeutic doses of LMWH (E)No bridging agent is needed Answer: no bridging is needed For this patient with CHADS2 score of 2 (HTN and DM2), no periprocedural bridging is needed. Periprocedural management of AC in s/o afib depends on patient’s risk of developing VTE and having an adverse bleeding event. The CHADS2 score is one commonly used risk stratification tool for the perioperative period: Low risk: CHADS2 0-2 -> no bridging or bridge with low-dose LMWH is appropriate Moderate risk: CHADS2 3-4, hx of TIA/CVA, or mechanical aortic valve -> bridging with therapeutic LMWH or UFH is reasonable High risk: CHADS2 5-6, recent TIA/CVA, mechanic MV or rheumatic valvular disease -> bridging with therapeutic LMWH or UFH should be provided. Question 7 54yo M is evaluated in the ED for 2hr history of palpitations. He reports no syncope, presyncope, chest pain, SOB and has had no previous episodes of palpitations. Medical hx is significant for nonischemic cardiomyopathy; EF was most recently measured at 38%. Medications are carvedilol and candesartan. On exam, he is afebrile, BP 125/86, pulse rate is 110/min. Cardiac evaluation reveals a regular rate and rhythm, although the intensity of S1 is variable. Cannon a waves are seen in the jugular venous pulsation. The ECG is shown. Which of the following is the most appropriate treatment? (A)Immediate cardioversion (B)IV adenosine (C)IV amiodarone (D)IV verapamil Answer: amiodarone The ECG demonstrates a regular, monomorphic wide-complex tachycardia in a LBBB pattern. The differential diagnosis is SVT with aberrancy, antidromic AVRT, and ventricular tachycardia. In a patient with wide-complex tachycardia with hx of CAD or CMY, VT should be the assumed diagnosis. The presence of AV dissociation in this ECG confirms the diagnosis of VT. In addition, the patient has variable S1 as well as cannon a waves, which are caused by atrial contraction against a closed tricuspid valve, confirming AV dissociation. Hemodynamic stability does not rule out VT. First line therapy for hemodynamically stable VT is IV antiarrhythmic agent such as amiodarone. Procainamide and sotalol are also acceptable, and lidocaine is secondline. Adenosine may be given for stable wide-complex rhythm to determine whether SVT or VT, but in this instance, the ECG and exam demonstrate VT. Verapamil or B-blockers are not indicated in patients with stable CT because they can lease to severe hemodynamic deterioration, Vfib, and cardiac arrest. Patient should be offered an ICD for long-term sudden death prevention. Distinguishing SVT from VT 1. VT more likely when interval between R and S is >100ms 2. Irregular RR interval is suggestive of SVT 3. AV dissociation with RR<PP interval is hallmark of VT 4. Typical RBBB or LBBB QRS morphology more likely SVT Question 8 62yo F is awaiting a procedure in the presurgical area. She has a single-chamber ICD and is about to undergo a hemicolectomy for colon cancer. Medical history is pertinent for ischemic cardiomyopathy, chronic afib, complete heart bock, and pacemaker dependence. Medications are aspirin, carvedilol, lisinopril, digoxin, warfarin (withheld), and rosuvastatin. Perioperative anticoagulation is provided with UFH. Which of the following is the most appropriate perioperative management of the patient’s ICD? (A)Insert a temporary pacemaker (B)Place a magnet over the ICD (C)Turn shock therapy off and change to asynchronous mode (D)No programming changes needed to ICD Answer: turn shock therapy off and change to asynchronous mode When a patient with ICD undergoes surgery, the use of electrocautery affects what the device “thinks” is happening with cardiac activity. It will treat the patient as if vfib is occurring, by inhibiting pacing and delivering a high-energy shock. Therefore, for a patient with ICD who is pacemaker dependent, the best management is to reprogram the device to turn off shock therapy and change to an asynchronous mode such as VOOO, which means that ventricular pacing will continue regardless of any native electrical activity or electrocautery. Placing a magnet over an ICD disables the shock function but does not affect the pacemaker settings. Question 1 60yo M is evaluated for chest pain of 4 months’ duration. He describes the pain as sharp, located in the left chest, with no radiation or associated symptoms, that occurs with walking 1-2 blocks and resolves with rest. Occasionally, the pain improves with continued walking or occurs during the evening hours. He has hypertension. Family history does not include CV disease in any 1st degree relatives. His only medication is amlodipine. On physical exam, he is afebrile, blood pressure 130/80mmHg, pulse rate is 72/min, and respiration rate is 12/min. BMI 28. No carotid bruits are present, and normal S1 and S2 with no murmurs are heard. Lung fields are clear, and distal pulses are normal. ECG is normal. Which of the following is the next mose appropriate diagnostic test to perform next? (A) Adenosine nuclear perfusion stress test (B) Coronary angiography (C) Echocardiography (D) Exercise treadmill test Answer: exercise treadmill test Most appropriate test to establish the diagnosis of CAD in this patient is an exercise treadmill test. The description of CP has both typical and atypical features. Based on pt’s age and sex, the pretest likelihood that his symptoms represent angina are increased, giving him an intermediate probability of CAD. The patient is able to exercise and has a normal baseline ECG. In this setting, an ETT is the most appropriate non-invasive test. Other choices: A: pharm stress test such as adenosine nuclear perfusion stress test is useful when a patient cannot exercise (ie arthritis, deconditioning, advanced lung disease) and in the s/o abnormal ECG B: coronary angiography has a small but inherent risk of vascular complications and is therefore usually not the first choice. Indications for cath: lifestyle-limiting angina despite optimal medical therapy, high-risk criteria on stress testing, or resuscitation from sudden cardiac death. C: echo is useful to evaluate left ventricular systolic function (EF), assess for WMA, and exclude significant valvular heart disease. Normal echo would not exclude underlying CAD. Choice of stress testing Question 33 68yo F is evaluated for palpitations. Her symptoms occur daily during both rest and exertion. She describes the papitations as intermittent “hard” beats that “take her breath away.” Her symptoms are made worse by caffeine consumption. She reports no dizziness or syncope. Medical history is significant for hypertension and hyperlipidemia. Medications are ACE inhibitor and statin. On physical exam, she is afebrile, BP 138/80mmHg, pulse rate 83/min, and respiration rate is 18/min. On cardiac examination, the rhythm is regular. There are no murmurs or extra sounds. The lungs are clear. The remainder of the general physical exam is normal. The ECG shows NSR with minor ST-segment abnormalities. What is the most appropriate testing option to utilize next in this patient? (A) Electrophysiologic study (B) 24-hour continuous ambulatory electrocardiographic monitor (C) Implantable loop recorder (D) Postsymptom event recorder Answer: 24-hr continuous ambulatory ECG monitoring When evaluating palpitations, it is important to capture the rhythm using ECG, continuous ambulatory ECG monitoring, an event recorder, or implantable loop recorder, depending on frequency of symptoms. The pt describes symptoms c/w premature ventricular contractions (PVCs). A PVC is followed by a compensatory pause, often described by pts as a “skipped beat.” PVCs often associated with caffeine, EtOH, nicotine. If no structural heart dz or fam hx SCD, PVCs are likely benign and reassurance is sufficient. Other answers: (A) EP testing is indicated for pts with rhythm d/o or other sx such as syncope who are at risk for sustained ventricular tacharrhythmia or SCD. (C) and (D) Event recorders are useful for symptoms that do not occur daily. Loop recorders record several seconds of the rhythm prior to device triggering. Postsymptom recorder is held to the chest when sx occur, and is useful only when symptoms last long enough for pt to activate the device. Question 40 41yo M is evaluated for progressive SOB over several months. Medical hx is significant for Hodgkin lymphoma, dx’d when he was a teenager. At that time he received doxorubicin, bleomycin, vinblastine, and dacarbazine with mantle radiation. He is currently in remission and takes no meds. On exam, he is afebrile, BP 128/70, pulse rate 74/min and regular. Estim CVP is 6cm H2O. An inspiratory decline in CVP is noted. The S1 is regular, with resp variation of S2. A II/VI midpeaking systolic murmur is heard. Lungs are clear. Given pt’s symptoms, TTE is ordered and shows normal biventricular size and systolic function. Diastolic indices show impaired left ventricular relaxation with normal left ventricular filling pressure. Pulmonary systolic pressure is 25-30mmHg. The IVC is of normal diameter, with full inspiratory collapse. Mild thickening of the aortic valve and mitral valve is observed. ECG shows NSR with 1st degree AVB and is otherwise unremarkable. Which of the following is the most appropriate diagnostic test to perform next? (A) Cardiac CT (B) Exercise ECG stress testing (C) Right heart catheterization (D) Transesophageal echocardiography Answer: exercise ECG stress testing Because of his hx of Hodgkin lymphoma treated with chemo and radiation regimens, there are multiple potential contributing factors to dyspnea present, including systolic and diastolic dysfunction, restrictive CMY, radiation valve disease, and CAD. CAD 2/2 radiation exposure is classically proximal, most commonly LAD. Risk of MI in survivors of HL is up to 7-fold greater than the general population, and persists beyond 20yrs after completing tx. Other common late CV complications include valve d/o, diastolic dysfunction, restrictive CMY, and pericardial constriction. Other answers: (A) Cardiac CT is helpful in evaluating pericardial constriction by visualizing pericardial thickness. Pt’s exam is not c/w this (no Kussmaul sign, no RHF, normal CVP and echo). (C) RHC is helpful in diagnosing pericardial constriction in pts w/compatible exam findings. Findings on RHC c/w constriction include equalization of diastolic pressures in PA and cardiac chambers, early diastolic “dipand-plateau” pattern on tracings and steep y descent. (D) TEE would provide little incremental diagnostic benefit to diagnose late-onset valvular disease, given that the valves were visualized with TTE. The II/VI midpeaking systolic murmur is c/w aortic sclerosis. Question 92 68yo F is evaluated for 3-week history of intermittent exertional chest pain. She walks several days per week. She has DM2 and HTN. Her father had an MI at age 54yrs. Medications are ASA, metformin, glyburide, and lisinopril. On exam, she is afebrile, BP 128/90, pulse rate is 83/min, and respiration rate is 18/min. BMI is 35. Cardiac sounds are distant but otherwise unremarkable, without extra sounds or murmur. An ECG is shown. Which of the following is the most appropriate diagnostic test to perform next? (A) Cardiovascular MRI with gadolinium enhancement (B) Exercise ECG stress test (C) Exercise stress echocardiography (D) Pharmacologic perfusion imaging study Answer: exercise stress echocardiography