Surgical Management of Male Infertility: Part I
advertisement

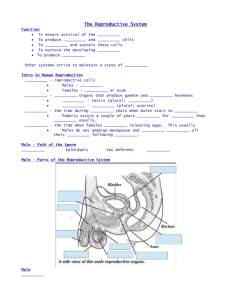
Surgical Management of Male Infertility: Part I By Peter Tran D.O. Garden City Hospital 12/17/2008 Overview • Surgical Treatment can be divided into 3 main categories – Diagnostic procedures • Testis biopsy • Seminal vesicle aspiration • vasography – Procedures to improve sperm production • Varicocelectomy – Procedures to improve sperm delivery • Vasovasostomy • Vasoepididymostomy Epidemiology • Varicoceles are now recognized as the most surgically correctable cause of male infertility. – – – • Varicocele repair remains the most cost-effective procedure in helping a subfertile man establish a pregnancy. – – • They are present in 15% of the normal male population. Up to 40% of patients with male infertility. Approximately 70% of patients with secondary infertility have been found to have a varicocele as an underlying cause. improve spermatogenesis increase serum testosterone Vasectomies – – – ½ million performed per year. 75% by urologist 12% of men aged 20 to 39 years in the United States have had a vasectomy 6% will eventually desire a reversal Diagnostic Procedures • Testicular Biopsy – Azoospermia with normal FSH and normal sized testicles. • Can be due to obstruction, defect in spermatogenesis, or incomplete defect • Obstruction vs. spermatogenic failure? • Can also be therapeutic - consider sperm retrieval for IVF/ICSI. – Should be perform on both testes for nonobstructive azoospermia. – In obstructive azoospermia, should biopsy the larger testis first. Diagnostic Procedures • Testicular Biopsy – Open – Percutaneous Open Testicular Biopsy 1. Cord block with 1% lidocaine and 0.25% bupivicaine with 30-ga needle 2. The scrotal skin and tunica vaginalis are then infiltrated with 2 mL of 1% lidocaine with a 30-ga needle. 3. A 1- to 2-cm transverse incision is made to the parietal tunica vaginalis through the anesthetized region. 4. The tunica vaginalis is then opened with scissors, and the edges are grasped and held apart with two small hemostats or a small self-retaining eyelid retractor. Lidocaine (2 to 3 mL) is dripped onto the exposed tunica albuginea to anesthetize the testicular surface where the biopsy specimen will be taken. Open Testicular Biopsy 5. The tunica albuginea is carefully inspected for the least vascular area for the incision. A 5-0 Prolene suture is passed at one end of the proposed site of incision in the testis. 6. A 4- to 5-mm incision is made in the tunica albuginea by use of a No. 11 scalpel or a microknife, allowing extrusion of the seminiferous tubules. 7. With the "no-touch" technique, fine, sharp iris scissors are used to carefully excise the extruded tubules. 8. The specimen is then placed in Zenker's, Bouin's, or buffered glutaraldehyde solution. The testicular specimen should not be placed in formalin. 9. “Touch imprint” or wet prep done. Touch imprint more predictive in the evaluation of spermatogenesis. Open Testicular Biopsy 10. If sperm are found and cryopreservation of testicular tissue is to be done, additional testicular tissue can be taken from the same site and placed in appropriate medium in individual Eppendorf tubes for processing by the andrology laboratory. 11. The incision is then closed with the previously placed 5-0 Prolene suture. It is important to close the tunica vaginalis over the testis with absorbable suture, such as 4-0 chromic or Vicryl. Percutaneous Testicular Biopsy 1. 2. 3. 4. Percutaneous testicular biopsy can be performed with local anesthesia in an office-based setting, and it is generally associated with less pain and morbidity than an open testicular biopsy. A 95% correlation was described between percutaneous needle and open biopsy techniques as long as sufficient materials are present for diagnosis. Before the biopsy is performed, the skin is punctured with a scalpel to prevent inclusion of scrotal skin with the specimen. To avoid injury to the epididymis and the surgeon's hand, the point of the needle insertion should be from the lower pole toward the upper pole. Testicular Biopsy Complications • Hematoma • Testicular atrophy – rare • Inadvertent epididymal biopsy Varicoceles • • • • • 15% of the normal male population and in up to 40% of patients with male infertility World Health Organization reported that varicoceles were found in 25.4% of men with abnormal semen parameters compared with 11.7% of men with normal semen. Varicoceles have been associated with impaired semen quality and decreased Leydig cell function. – However, varicocele repairs have been shown to improve not only spermatogenesis but also Leydig cell function – most commonly performed surgical procedure in treatment of male infertility. Grading of Varicocele – I - Palpable only with the Valsalva maneuver – II - Palpable without the Valsalva maneuver – III - Visible through the scrotal skin – Repair of larger varicoceles results in significantly greater improvement in semen quality than does repair of smaller varicoceles. – On scrotal US – dilated veins > 3.5 mm Subclinical varicoceles – Diagnosed only on US – Studies have demonstrated that subclinical varicoceles have no impact on fertility and that repair of subclinical varicoceles does not improve fertility rates. Varicoceles • • Four indications for treatment in adult men – The couple has known infertility – The female partner has normal fertility or a potentially treatable cause of infertility – The varicocele is palpable on physical examination, or if it is suspected, the varicocele is corroborated by ultrasound examination – The male partner has an abnormal semen analysis In adolescent men – Reduction in ipsilateral testicular size, otherwise observation and /or semen analysis. Varicoceles • Surgical Approaches – Scrotal • No longer used. High failure rate and testicular artery injury risk. – Retroperitoneal • Palomo – High retroperitoneal ligation of the internal spermatic vein above the internal inguinal ring. – A common complication of the retroperitoneal approach is varicocele recurrence or persistence, estimated to be between 11% and 15%. – The recurrence can be significantly reduced by intentional ligation of the testicular artery. This is thought to ensure ligation of the periarterial/cremasteric veins and thus to prevent recurrence. – Laparoscopic • Excessively invasive for what should be a minor outpatient procedure • laparoscopic varicocele repairs have been associated with a recurrence rate of less than 2% and formation of hydroceles in 5% to 8% of patients Varicoceles • Inguinal and subinguinal approach – Preferred approaches – Less morbidity associated with the subinguinal (infrainguinal) approach than with the laparoscopic and inguinal approach because of the preservation of the muscle layers and the inguinal canal – However, a greater number of internal spermatic veins and arteries lie below the external ring, making this procedure technically more challenging Lap Varicolectomy 1. 2. 3. 4. Essentially the same as the Palomo technique. Establish pneumoperitoneum using Veress or Hassan technique. Parietal peritoneum is incised just lateral to the spermatic cord. The testicular artery and veins are dissected and isolated. Pulling on the testis can help identify the vessels. Once the veins are isolated, they are clipped both proximally and distally with titanium endoclips, and these vessels are then transected. Inguinal Approach 1. 2. 3. 4. 5. 3- to 4-cm oblique incision, two fingerbreadths above the symphysis pubis and just above the external ring, is carried laterally along Langer's lines Incision is carried down to the external oblique aponeurosis, which is incised in the direction of its fibers. Care is taken to identify and to preserve the ilioinguinal nerve . The spermatic cord is mobilized near the pubic tubercle, and a Penrose drain is passed beneath the cord. The Penrose drain is used to elevate the cord and bring it through the incision. (+/-) microscope/loupes Varicoceles generally appear with a typical vascular pattern in which the artery is next to or adherent to several veins, and there is a separate isolated vein nearby. Inguinal Approach 6. Once the dilated veins are isolated, they are doubly ligated with either 2-0 silk sutures or small titanium surgical clips. 7. With the microsurgical technique, the lymphatic channels can be clearly visualized, and these should be preserved to prevent postoperative hydrocele formation. 8. The floor of the inguinal canal, near the external ring, should also be inspected to identify and ligate any external cremasteric veins. 9. The cord is placed back into the canal, and the external oblique fascia is closed with a 30 Vicryl suture. The subcutaneous layer is reapproximated with a 3-0 plain catgut suture, and the subcuticular layer is closed with a 4-0 Monocryl suture. The incision is infiltrated with 1% lidocaine mixed with an equal amount of 0.5% bupivacaine. Varicocelectomy Microsugical vs. Non-microsurgical Approach • Significant reduction in postoperative complications, such as testicular artery injury, hydrocele formation, and varicocele recurrence. • Complication rates for hydrocele formation with the non-microsurgical technique range from 3% to 39%, whereas hydrocele formation is rarely reported in association with a microsurgical technique • The recurrence rate for microscopic inguinal varicocelectomy has been reported between 1% and 2%, compared with 9% and 16% for nonmicroscopic inguinal varicocele repair • The recurrence rate for non-microscopic subinguinal varicocele repair is reported to be 5% to 20% Varicocelectomy • Percutaneous Embolization – Cut-down to femoral or internal jugular vein – embolization of the spermatic veins can be accomplished with coils, balloons, or sclerotherapy – Overall success rate – 68% – Percutaneous varicocele embolization is especially useful in a recurrent or persistent varicocele, when the anatomy causing the varicocele needs to be radiographically clarified. Varicocelectomy • • Outcomes – studies have shown that repair of varicoceles can retard further damage to testicular function – overall rate of improvement in semen parameters after varicocelectomy ranged from 51% to 78% – improve not only semen motility, density, and morphologic features but also serum FSH and testosterone levels – No difference noted between laparoscopic and open approach, but higher complications in the lap. Group Predictors of successful repair – Sperm concentration > 5million/ml or density > 50 million per ejaculate – lack of testicular atrophy – sperm motility of 60% or more – serum FSH values less than 300 ng/mL (normal, 50 to 300 ng/mL) Varicolectomy Complications Technique Artery Preserved Hydrocele (%) Recurrence (%) Retroperitoneal No 7 11-15 Conventional inguinal No 3-39 9-16 Laparoscopic Yes 5-8 <2 Radiographic Yes 0 4-11 Microscopic inguinal or subinguinal Yes 0 <2 Cost Effectiveness • • Probability of a live birth after a varicocelectomy was 29.7% versus 25.4% after IVF-ICSI. The cost per delivered baby was $26,268 after varicocelectomy compared with $89,091 with IVF-ICSI. Vasectomy Reversal • • • • • 6% of men who have undergone vasectomy will subsequently request a vasectomy reversal Chances for success (patency or pregnancy) based on the personal experience of the surgeon, the patient's health history, and the results of examination of the man and the age and reproductive potential of his partner are discussed. Epididymal obstruction appears, in most instances, to be a time-related phenomenon – 62% of patients who underwent reversal 15 years or more after their vasectomy required either a unilateral or a bilateral vasoepididymostomy – VE depends on quality of fluid from proximal vas • when the material coming from the proximal vas lumen is thick, pasty, and devoid of sperm; if the fluid is creamy, containing only debris. microsurgical vasectomy reversal are superior to results of nonmicrosurgical techniques No significant difference if a multilayer anastomosis is performed as opposed to a modified single-layer technique but the success is physician-dependent. Vasovasostomy Instruments A. Nonlocking needle holder. B. Suture scissors. C. Dissecting scissors. D,E. Very fine pointed and roundtipped scissors. F. Round-handled platform forceps. G. Curved dilating forceps. H. Round-handled small knife blade holder. I. Microtip bipolar cautery Vasovasostomy Anesthetic Considerations 1. 2. General vs. local? Preparing the vas for anastomosis 1. 2. 3. Vas grasped through skin above the vasectomy site. Once the vas is exposed, injection of a mixture of 0.5% bupivacaine and 1% lidocaine into the distal perivasal sheath will provide sufficient anesthetic coverage for the vasal anastomosis to be performed. Placement of 6-0 Prolene sutures just into the muscularis holds the vas above the incision and make it easily accessible for anastomosis. Vasovasostomy 4. The vas above and below the vasectomy site should be transected with use of the operating microscope Once the point of the vas that is to be cut is chosen, the vasal vessels are secured with 7-0 Prolene sutures just proximal to the point of transection. Some experienced microsurgeons prefer to cut the vas deferens through the groove of a nerve-holding forceps to ensure a straight cut. 5. A few drops of fluid from the testicular end of the vas lumen are placed on a sterile glass slide and examined by light microscopy. 6. If there are sperm or sperm parts (sperm heads, sperm with partial tails) in large numbers or the fluid is clear and copious with no visible sperm, vasovasostomy is generally indicated. If the fluid is thick, pasty, and devoid of sperm or contains only a few sperm heads, vasoepididymostomy should be considered. Vasovasostomy Multilayer Anastomosis 1. 2. 3. 4. The anastomosis is begun by passing a 9-0 suture through the muscularis and the adventitia at the 5- and 7-o'clock positions . A double-armed 10-0 suture is passed through the lumen at the posterior 6-o'clock position and tied. The next sutures are placed in the wall of the lumen on either side of the first. These sutures are tied after both are in place. Three to five more sutures are placed equidistant from one another to close the remainder of the lumen but are left untied until all the sutures have been placed. Vasovasostomy Multilayer Anastomosis 5. 6. Once the anastomosis of the lumen has been completed, the 90 suture is again used to bring the muscularis together. A suture is placed at the 12-o'clock position first, then sequentially around the cut end of the vas until the first two sutures are reached . The adventitia is brought together over the muscularis suture line with interrupted 9-0 sutures to further enhance the blood supply at the level of the anastomosis. Vasovasostomy – Single Layer Anastomosis 1. 2. 3. 4. A double-armed 10-0 suture is passed full thickness through the edge of the proximal and distal lumen at the 6-o'clock position. Two more sutures are placed, full thickness, at the 4- and 8-o'clock positions and tied. Three more full-thickness sutures are passed at the 10-, 12-, and 2o'clock positions and then tied. The anastomosis is completed by closing the muscularis and adventitia to the opposite side, placing two 9-0 sutures between each of the 10-0 full-thickness sutures. Vasovasostomy • • • Consider sperm retrieval/cryo during vasovas – 8-14% of pts. Use their cryopreserved sperm – Can always do testis biopsy and sperm extraction at a later date. Post-op Care – Moderate activity for the first week after surgery and to refrain from heavy exercise and sexual activity for 3 weeks. Examination of the semen occurs at 1 month and every 3 months in the year after surgery. Most patients will have sperm in their semen within 4 weeks after vasovasostomy. – If sperm are not present by 6 months, the operation is considered a failure. • Repeated surgery or sperm retrieval and IVF-ICSI may be offered. Complications – Secondary obstruction and consequent azoospermia after initially successful vasovasostomy have been reported to occur in 3% to 12% of men. • marked decrease in motility and the appearance of sperm heads along with some normal sperm Vasovasostomy Years of Obstruction Patency (%), Sperm Present Pregnancy (%) <3 86/89 (97) 56/74 (76) 3-8 525/600 (88) 253/478 (53) 9-14 205/261 (79) 92/209 (44) ≥15 32/45 (71) 11/37 (30) Vasoepididymostomy • • • Epididymal Obstruction – Can be idipathic, inflammatory, iatrogenic, congenital. – Time-dependent with vasectomy. – Decision to perform a vasoepididymostomy is based primarily on the quality of fluid found at the proximal (testicular) vas. 3 microsurgical techniques – Direct end-to-end – End-to-side – End-to-side intussusception Pre-op Consideration – General/epidural anesthetic – Cryopreserve sperm? – Patient positioning/comfort/safety Vasoepididymostomy 1. Testis biopsy to confirm spematogenesis. 2. Incision is enlarged and the testis delivered out of the scrotum and examined. In most instances, the epididymis will be visibly dilated, even without optical magnification . 3. Mobilize the distal vas. 4. Confirm vasal patency with vasography. Vasoepididymostomy : End to End 1. 2. 3. The epididymal tail can be dissected free from the inferior aspect of the testis and the epididymis transected at its distal end. When the epididymis is cut proximal to the obstructed area, there will be a continuous flow of sperm-laden fluid from one opened epididymal tubule. The lumen of the vas deferens is anastomosed to the cut, open tubule exuding sperm. The first step is to secure the cut end of the abdominal vas to the epididymal tunic with two 9-0 nylon sutures passed through the edge of the epididymal tunic and into the adventitia and muscularis of the vas deferens at the 5- and 7-o'clock positions. Four equally spaced doublearmed 10-0 sutures are placed into the edge of the epididymal tubule, inside out, and then carried through the vas lumen, beginning at the 6-o'clock position. The first suture is tied, but the sutures at the 3-, 9-, and 12-o'clock positions are not tied until all are placed. Vasoepididymostomy : End to End 4. The muscularis and adventitia of the vas deferens are secured to the tunic of the epididymis with interrupted 9-0 sutures . Vasoepididymostomy : End to Side 1. 2. 3. 4. The rationale is that there is far less dissection required, less troublesome bleeding from the transected epididymis, and therefore a clearer field. Beginning at the level of the cauda, a 0.5-cm incision is made in the tunic of the epididymis, pushing the tubule toward the tunic surface. The anterior surface of this loop is incised along its longitudinal axis with a microknife, making an opening of approximately 0.5 mm. Fluid is examined for normalappearing sperm. Vasoepididymostomy : End to Side 5. Once the patent loop is identified and opened, three 10-0 double-armed sutures are placed (inside-out) in a triangular fashion equidistant from one another 6.The vas deferens is brought through the uppermost portion of the tunica vaginalis . 7. Two 9-0 nylon sutures are used to hold the muscularis and adventitia of the vas deferens to the opened epididymal tunic. Vasoepididymostomy : End to Side 8. The apical suture that was passed into the epididymal lumen is now passed into the lumen of the vas deferens and secured. 9. Three other sutures are then placed in between the previous one and tied posteriorly to anteriorly. Vasoepididymostomy : End to Side 10. The muscularis and adventitia of the vas deferens are approximated to the epididymal tunic, in a circumferential fashion, with eight to ten 9-0 sutures. Vasoepididymostomy : 3 Suture Intussusception 1. This technique differs from the end-to-side technique in that the lumen is opened after the sutures are positioned in the epididymal loop. Vasoepididymostomy : 2 Suture Intussusception 1. In the two-suture modification, once the dilated epididymal loop is identified and the end of the vas brought in close to the epididymal loop, it is secured to the tunic with a single 9-0 suture, and two parallel sutures are passed into the tubule and left in position. Vasoepididymostomy • • Post-op Care – Similar to VasoVas Complications – Infection – Hematoma – DVT – Injury to testicular artery • Results – Very wide variation even with microsurgical techniques.