Krista CapehartPharmacisat IMZ update
advertisement

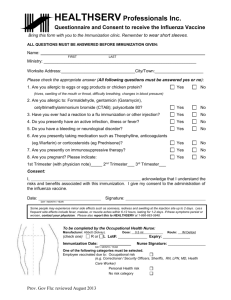
Vaccine Update and Refresher for Immunizations: 2012 Krista D. Capehart, PharmD, MSPharm, AE-C David G. Bowyer, R. Ph. Assistant Professors of Pharmacy Practice University of Charleston School of Pharmacy Objectives • Determine the appropriate vaccine recommendations for a patient based on current immunization schedules. • Apply individual vaccine characteristics to identify anticipated vaccine adverse events. • Explain the Advisory Committee on Immunization Practices (ACIP) recommendations for vaccines pharmacists can administer in West Virginia. • Summarize critical information needed for the administration of influenza and pneumococcal. • Investigate information about the vaccines added to Title 15 Series 12 of the West Virginia Code for immunization rules. Pharmacist Administered Immunizations in WV • HB 3056 passed in 2008 authorizing specially trained pharmacists in WV to administer influenza and pneumococcal polysaccharide • Additional vaccines could be added following joint rulemaking with WV Board of Medicine, WV Board of Osteopathy, and WV Board of Medicine • Summer 2011 joint rule-making occurred and was approved by the 2012 Legislature • Pharmacists can now administer Hepatitis A, Hepatitis B, Tetanus, and Herpes Zoster in addition to influenza and pneumococcal vaccines Current Title 15 – Series12 • Qualifications for pharmacists to administer immunizations: – Any person ≥ 18 years old – Registered with the Board of Pharmacy (BOP) to administer immunizations – Successfully complete immunization training course approved by the BOP – Maintain current certification to basic life-support – Complete 2 hours annually of continuing education related to immunizations Current Title 15 – Series12 • Must have immunization questionnaire and consent form, notify patient’s primary care provider (PCP) within 30 days of administration • Report the administration to the WV Statewide Immunization Information (WVSII) database within 30 days of administration • Must have consent & questionnaire readily retrievable and maintained on file for not less than 5 years • Pharmacists can administer epinephrine and diphenhydramine to manage acute allergic reaction following CDC guidelines • Pharmacists must have readily retrievable emergency response plan as outlined by the CDC and a readily retrievable emergency kit to manage an acute allergic reaction to an immunization administered Pharmacists as Immunizers in WV • As of June 2012, 1663 pharmacists have completed the mandated training course and are registered with the West Virginia Board of Pharmacy as Immunizing Pharmacists. • This represents approximately 50% of the pharmacists practicing in WV. • This addition to the immunizing workforce increases the access to immunizations for the public. Updates to Title 15 – Series 12 • Adds: – – – – Hepatitis A Hepatitis B Herpes Zoster Tetanus (follows CDC recommendations and permits tetanusdiphtheria (Td) or tetanus-diphtheria-pertussis (Tdap) • Pharmacists must report all adverse events to the Vaccine Adverse Events Reporting System (VAERS) and provide a copy to the BOP (available at http://vaers.hhs.gov/index) Case Study 1 • A family comes in to the pharmacy. The mother is a 40yo WF with a 15yo WM and 19 WF children requests immunizations for herself and her family. After discussing with her what she needs, you determine that they all need TIV and her daughter needs Hep B. • What immunizations could the pharmacist currently provide for the family? Advisory Committee on Immunization Practices (ACIP)Recommendations for Adult Influenza Immunizations • Vaccination recommended for all adults (including healthy adults 19-49 years without risk factors) • Live attenuated influenza vaccine – only approved for healthy non-pregnant people age 2-49 years • 65 years and older can get standard-dose Trivalent inactivated influenza vaccine (TIV) or the high does TIV • Give 1 dose every year in the fall or winter • Begin vaccination as soon as vaccine is available and continue until supply is depleted • If 2 or more live virus vaccine are given – give same day or they must be separated by at least 28 days Needle Tips from the Immunization Action Coalition Volume 21 Number 3 July 2011 available at www.immunize.org Advisory Committee on Immunization Practices (ACIP)Recommendations for Adult Influenza Immunizations • Mild illness is not a contraindication • Contraindications: – Previous anaphylactic reaction to vaccine, components, or eggs – LAIV only: pregnancy, chronic pulmonary problems, cardiovascular (except hypertension), renal, hepatic, neurological/neuromuscular, hematologic, or metabolic disorders, immunosuppression • Precautions: – Moderate or severe acute illness – History of Guillain-Barre syndrome within 6 weeks of previous influenza – LAIV only: taking antivirals 48 hours before vaccination and avoid using antivirals for 14 days after vaccination Needle Tips from the Immunization Action Coalition Volume 21 Number 3 July 2011 available at www.immunize.org Estimates of Cumulative Influenza Vaccination Coverage for 2010-2011 Season • • • • West Virginia 48% United States 43% Among those ≥ 18 years in US vaccination rate 40.4% High risk group remains: elderly, young children, pregnant women, and people with chronic conditions • Healthy People 2020 target is: – 80% for persons 6 months – 64 years – 90% for those ≥ 65 years Final state-level influenza vaccination coverage estimates for the 2010–11 season–United States, National Immunization Survey and Behavioral Risk Factor Surveillance System, August 2010 through May 2011 available at http://www.cdc.gov/flu/professionals/vaccination/coverage_1011estimates.htm Influenza Activity U.S. 2010-2011 • Higher rates of hospitalization in ≥ 65 years than in 2011-2012 • 22% of specimens tested were positive with the virus peaking in February 2011 • 74% of positive specimens were Type A and 26% were Type B • Proportion of specimens testing positive was <10% during the week ending April 16, 2011 MMWR 2011;60(21):705-712 Resistance in 2010 to Antivirals • 5,758 influenza viral specimens tested for resistance • All 723 influenza B were sensitive to oseltamivir and zanamivir • 2 of 806 Influenza A (H3H2) were resistant to oseltamivir • All 784 influenza A (H3H2) were sensitive to zanamivir • Of the 4,229 influenza A (H1N1) 39 were resistant to oseltamivir; of the 771 testes with zanamivir, all were sensitive • High resistance to adamantanes (amantadine and rimantadine) MMWR 2011;60(21):705-712 2010-2011 Pneumonia and Influenza Related Mortality • Percentage of deaths attributable to pneumonia and influenza exceeded the epidemic threshold from January 29, 2011 to April 23, 2011 • Peaked at 8.9% week ending February 12, 2011 • From October 3, 2010 to May 21, 2011 had 311 lab confirmed influenzaassociated deaths were reported to CDC MMWR 2011;60(21):705-712 Place of Influenza Vaccination Among Adults US 2010-11 Season • Overall: doctor’s office was the most common place (39.8%), followed by “store” (supermarket or drug store) at 18.4%, and workplace 17.4% • Those 65 and older were most likely (51.5%) to be vaccinated at a doctor’s office than a store (24.3%) • High risk individuals were more likely to get their vaccination in a doctor’s office than those without (49.1% vs 35.7%) MMWR; 60(23): 781-785 . Early Estimates of Cumulative Influenza Vaccination Coverage for 2011-2012 Season • Among adults ≥ 18 years, estimated vaccination coverage was 45.5%, an increase from 41.1% the previous season • Estimated 2011-12 coverage among adults 18-49 years increased by 7 percentage points compared to the 2010-11 season. • Estimated coverage among adults increased with each increase in adult age group. Estimated coverage among adults was highest in adults ≥ 65 years (70.8%) and lowest among adults 18-49 years (35.8%). • Estimated coverage among adults 50 to 64 years or ≥ 65 years did not differ when compared to the same time the previous season. March 2012 National Immunization Survey and National Flu Survey - United States, 2011-12 Influenza Season http://www.cdc.gov/flu/professionals/vaccination/nfs-survey-march2012.htm accessed 6/6/12 Place of Vaccination 2011-12 • The most common place of vaccination among adults (32.5%) was a doctor’s office These results are similar to results from the 2010-11 season when 31.6% of adults were vaccinated in doctor’s offices. • Other common places of influenza vaccination reported for adults during the 2011-12 season included medically related places besides doctor’s offices (24.7%), pharmacies or stores (19.7%), and workplaces (13.8%). • March 2012 National Immunization Survey and National Flu Survey - United States, 2011-12 Influenza Season http://www.cdc.gov/flu/professionals/vaccination/nfs-survey-march2012.htm accessed 6/6/12 Pneumococcal disease • Pneumococcal disease most often occurs in older people as well as in people with a predisposing condition (e.g., pulmonary disease, asplenia). • Pneumococcal disease most commonly presents as a serious infection in the lungs (pneumonia), blood (bacteremia), or brain (meningitis). The annual U.S. case estimate for invasive pneumococcal disease (bacteremia and/or meningitis) is 40,000. • PPSV is 60–70% effective in preventing serious pneumococcal disease; it does not provide substantial protection against all types of pneumonia (viral and bacterial). It is not a “pneumonia” vaccine. Pneumococcal Polysaccharide Vaccination Pocket Guide : http://www.immunize.org/ppvguide/pocketguide.pdf; accessed 6/6/12 Pneumococcal Polysaccharide (PPSV) • Recommended for people 65 years and older; younger than 65 years with chronic illnesses or other risk factors (cardiac, pulmonary, liver disease, alcoholism, diabetes, cigarette smoking); Those at highest risk including asplenia, immunocompromising condition, chemotherapy, or has received organ or bone marrow transplant • Give 1 dose if history is unknown or unvaccinated • Give a 1 time revaccination to: – Age 65 years and older if 1st dose was before age 65 years and more than 5 years ago – Age 19-64 years at high risk of fatal pneumococcal infection and 5 years have elapsed since the 1st dose Needle Tips from the Immunization Action Coalition Volume 21 Number 3 July 2011 available at www.immunize.org Estimated proportion of adults who received Pneumococcal vaccination 2010 • 19–64 yrs, high risk 18.5 • ≥65 yrs 59.7 • Healthy People 2020 goals call for 90 % of the non-institutionalized adults aged 65 years and older and 60% of non-institutionalized high-risk adults aged 18 to 64 years to be immunized. • Neither overall coverage nor coverage for any specific age or racial/ethnic group differed significantly from 2009 coverage. National Health Interview Survey, United States, 2010-MMWR February 3, 2012 / 61(04);66-72 accessed 6/6/12 Case Study 2 • A 70 yo male comes into the pharmacy to be immunized for influenza and pneumococcal. He had his last flu shot last year and pneumococcal when he was 60yo. • He asks about the nasal flu vaccine. Is he a candidate? Why or why not? • He asks about the “high dose” flu vaccine. Is he a candidate? Why or why not? • Should he get his PPSV today? Why or why not? Herpes Zoster (Shingles) – Give Subcutaneous Injection • • • • • For people age 60 years and older Give 1 time dose if unvaccinated, regardless of history of shingles or chickenpox If giving 2 or more live vaccines at same time (MMR, Zoster, Yellow fever), should be given on the same day or must be separate by 28 days Contraindications – Previous anaphylactic reaction to any component of vaccine – Primary cellular or acquired immunodeficiency – Pregnancy Precautions – Moderate or severe acute illness – Receipt of antivirals 24 hours before vaccination; if possible, delay resuming antivirals for 14 days after vaccination Needle Tips from the Immunization Action Coalition Volume 21 Number 3 July 2011 available at www.immunize.org Tetanus • Comes as tetanus-diphtheria (Td), tetanus-diphtheria-pertussis (Tdap), or tetanus (TT) • Give intramuscular • All who do not have written documentation of a primary series of at least 3 doses of tetanus and diphtheria • Booster of Td or Tdap may be needed for wound management • In pregnancy, give Td or Tdap if indicated in 2nd or 3rd trimester. If not given during pregnancy, give Tdap immediate postpartum period • Tdap ONLY: – Adults <65 years who have not already had Tdap – Adults of any agent in close contact with infants < 12 months who have not had a dose of Tdap – Healthcare personnel of all ages – Adults ≥ 65 years without a risk factor may also be vaccinated with Tdap Needle Tips from the Immunization Action Coalition Volume 21 Number 3 July 2011 available at www.immunize.org Tetanus (cont.) • Schedule – Those unvaccinated or behind, complete the primary Td series (spaced at 0, 12months, 6-12 month intervals); substitute a one-time dose of Tdap for one of the doses in the series, preferably the first – Give Td booster every 10 years after primary series has been completed – Tdap can be given regardless of interval since previous Td • Contraindications – Previous anaphylactic reaction to vaccine or components – For Tdap only, history of encephalopathy, not attributable to an identifiable cause, within 7 days following DTP/DTaP • Precautions – Moderate and severe acute illness – Guillian-Barre syndrome within 6 weeks following previous dose of tetanus toxoid containing vaccine – Progressive or unstable neurologic disorder, uncontrolled seizures, or progressive neuropathy Needle Tips from the Immunization Action Coalition Volume 21 Number 3 July 2011 available at www.immunize.org Hepatitis A (Hep A) • Give Intramuscularly • All who want protection from Hep A and those who work or travel anywhere EXCEPT U.S., Western Europe, New Zealand, Australia, Canada, and Japan • Those with chronic liver disease; injecting & non-injecting drug users; men having sex with men; those getting clotting concentrates; those who work in labs with Hep A; some food handlers • People with close contact with an international adoptee from a country of high or intermediate endemicity during the first 60 days following the adoptee’s arrival in the US • Adults age 40 years or younger with recent (within 2 weeks) exposure to Hep A. For older people (<40years), with recent (within 2 weeks) exposure to Hep A immune globulin is preferred over the Hep A Vaccine Needle Tips from the Immunization Action Coalition Volume 21 Number 3 July 2011 available at www.immunize.org Hepatitis A (Hep A) cont. • Give 2 doses; minimum interval between doses 1 and 2 is six months • If 2nd dose is delayed, don’t repeat the first dose, just give the second dose. • Contraindications: – Previous anaphylactic reaction to this vaccine or to any of its components. • Precautions: – Moderate or severe acute illness – Weigh risk versus benefit in pregnancy Needle Tips from the Immunization Action Coalition Volume 21 Number 3 July 2011 available at www.immunize.org Hep A and Hep B Combination (Twinrix®) • For 18 years and older • 3 doses on 0,1, and 6 month schedule • At least 4 weeks between dose 1 and 2 and 5 months between dose 2 and 3 • OR • Alternative schedule: 0, 7day, 21-30 day, and a booster at 12 months Needle Tips from the Immunization Action Coalition Volume 21 Number 3 July 2011 available at www.immunize.org Hep B • Give intramuscularly • All who want to be protected against Hep B • High risk: household contacts, sex partners, injecting drug users, those not in long term mutually monogamous relationships, men having sex with men, people with HIV, persons seeking STD evaluation or treatment, hemodialysis patients, healthcare personnel and public safety workers, inmates at long term correction facilities, chronic liver disease and certain international travel Needle Tips from the Immunization Action Coalition Volume 21 Number 3 July 2011 available at www.immunize.org Hep B (cont.) • 3 doses on a 0, 1, 6 month schedule • At least 4 weeks between dose 1 and 2, at least eight weeks between doses 2 and 3, at least sixteen weeks between doses 1 and 3 • If patients fall behind in schedule, do not start over just pick up where left off • Contraindications: previous anaphylactic reaction to this vaccine or any components • Precautions: Moderate or severe acute illness Needle Tips from the Immunization Action Coalition Volume 21 Number 3 July 2011 available at www.immunize.org Case study 3 • A 70yo patient comes into the pharmacy. She is interested in getting her flu shot, pneumococcal vaccine, and anything else she “needs” before she goes to Arizona to help take care of her new twin granddaughters who are 6 weeks old. • What other information do you need to know? • What vaccinations does she need? • What could the pharmacist give her today? References • • • • • • • • • Needle Tips from the Immunization Action Coalition Volume 21 Number 3 July 2011 available at www.immunize.org Final state-level influenza vaccination coverage estimates for the 2010–11 season–United States, National Immunization Survey and Behavioral Risk Factor Surveillance System, August 2010 through May 2011 available at http://www.cdc.gov/flu/professionals/vaccination/coverage_1011estimates.htm MMWR 2011;60(21):705-712 MMWR 2011; 60(23): 781-785. MMWR 2011:60(33):1128-1132. Questions & Answers Fluzone High–Dose Seasonal Influenza Vaccine available at http://www.cdc.gov/flu/protect/vaccine/qa_fluzone.htm Intradermal Influenza (Flu) Vaccination available at http://www.cdc.gov/flu/protect/vaccine/qa_intradermal-vaccine.htm Vaccines, Blood and Biologics FDA Updated Communication on Use of Jet Injectors with Influenza Vaccines. Available at http://www.fda.gov/BiologicsBloodVaccines/Vaccines/QuestionsaboutVaccines/ucm2 76773.htm accessed on October 26, 2011.