OBJECTIVE #4: Pathogens Transmissible by the Oral Cavity

Pathogens and the Oral Cavity
Wilkins CH 4
Concorde Career College
Preclinical Sciences DH101
Lisa Mayo, RDH, BSDH
Staci Janous, RDH, BS
Pathogens Transmissible by the Oral Cavity
Wilkins CH4
Tuberculosis p.44-45
Viral hepatitis p.45-50
HIV p.54-58
Herpetic infections p.50-54
Tuberculosis
Tuberculosis: special consideration when sterilization and disinfection methods are selected and administered
Transmission: Inhalation of fresh droplets containing tubercle
bacilli disseminated from sputum & saliva of infected individual by coughing, sneezing, or breathing heavily
Areas of infection: lungs (most common), lymph nodes, meninges, kidneys, bone, skin, & oral cavity
Factors affecting transmission
Maximum communicability is just before the disease is diagnosed
Tuberculosis
Clinical management: CDC recommendations
1.
Annual risk assessment
2.
Screening of all newly employed DHCP
3.
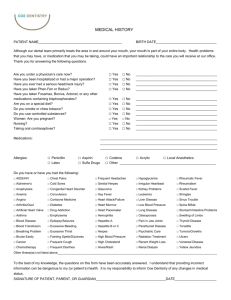
Taking and updating medical history
4.
Referral of patients with suggestive TB history or symptoms
5.
Deferral of elective dental treatment
6.
Urgent dental care be provided in a facility that can offer isolation
(Source: McInnes ME. Essentials of communicable disease. 2nd ed. St. Louis: The C.V. Mosby Co.; 1975).
Review
Tuberculosis infection occurs most commonly in which area?
A) Lymph nodes
B) Lungs
C) Kidneys
D) Liver
Answer
B) Lungs is the correct answer.
Tuberculosis infection occurs most commonly in the lungs, although it can occur in lymph nodes, kidneys, bone, skin,
& the oral cavity.
Viral Hepatitis
Inflammation of the liver
Causes
Viral & bacterial infections
Toxins & certain medications
Heavy alcohol use
Viral Hepatitis
Categories
A & E: Oral-fecal route. Unsanitary food & water
B, C, & D: Blood-borne route. Impacts DH
F & G: New, transfusion-transmitted
HEPATITIS B
Hepatitis B (HBV)
Serious, endemic, worldwide disease
Use of strict sterilization of equipment & materials, aseptic techniques, & self-protection measures is mandatory
Transmission (cont’d next slide)
• Blood & other body fluids
• Childbirth (mom to child)
• Accidental needle stick
• Exchanging contaminated needles, syringes, & other IV drug paraphernalia
1.) Sexual exposure
2.) Infection from blood transfusion & blood products
Hepatitis B
Prevention: critical occupational hazard for DH due to close association with potentially infected body fluids of patients
Preventive measures
Prenatal testing of all pregnant women for HBsAg
Universal immunization: available since 1982
Blood bank control measures (screening of donors, strict testing for all donated blood)
Public education
Hepatitis C
General facts: Serologic test for antibody to HCV was developed in
1991, routine blood screening was implemented in 1992.
Transmission: primarily parenteral
No documentation of transmission from intact or non-intact skin exposures to blood
Sexual contact with infected partner most common
Prevention & control: No vaccine is available for HCV
Education & behavior modification
Standards precautions in dental office
Hepatitis D
Delta hepatitis virus causes infection ONLY in the presence of
HBV infection (Memory trick: ‘B’ BEFORE ‘D’)
Transmission
Delta infection is superimposed on HBsAg carriers
Multiple exposures to HBV, especially those with hemophilia and IV drug use
Transmission similar to that of HBV
Prevention: same measures used to prevent HBV
Immunization with HBV vaccine also protects the recipient from delta hepatitis infection (NBQ)
Diagram shows the delta antigen surrounded by HBsAg.
(Source: Hoofnagle JH. Type D hepatitis and the hepatitis delta virus. In: Thomas HC, Jones EA, editors.
Recent advances in hepatology. Edinburgh: Churchill Livingstone; 1986).
Herpes
1. Description
2. HSV1 & 2: Primary Herpetic Gingivostomatitis, Herpes Labialis,
Herpetic Whitlow, Ocular/Ophthalmic Herpes, Genital herpes
3. HSV3: Varicella-Zoster Virus
4. HSV4: Epstein-Barr Virus
5. HSV5 Cytomegalovirus
6. HSV8 Kaposi’s Sarcoma
Herpes Virus Diseases Description
Endemic worldwide
Public health problem
8 strains known to infect humans
Herpes viruses produce diseases with latent, recurrent, malignant tendencies
HS type 2 has been implicated in cervical cancer
HS type 1 in oral cancer
Epstein-Barr virus with various types of cancer
After infection: virus can remain latent & cause recurrent infections
Herpes Virus Description
Relation to periodontal disease
Human herpes viruses occur in periodontitis, found in pocket flora with relatively high prevalence
Viruses can suppress a patient ’ s immunity – allows for opportunistic pathogens – makes perio more severe
Herpes Virus Description
HSV-1: primary infection usually occurs in children
Antibodies (anti-HSV) are produced – does NOT guarantee immunity to recurrent herpes or other herpes virus infections
Sulcular epithelium: reservoir for the viruses
Trauma from dental procedures can reactivate virus
Herpes Virus Diseases
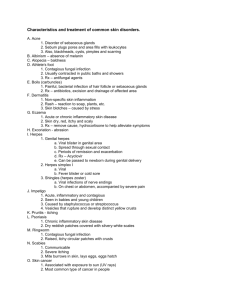
Primary Herpetic Gingivostomatitis
Primary infection of HSV-1
Widespread oral ulcers that may involve pharyngeal areas
Fever, malaise, inability to eat, swollen lymph nodes
Reactivation may also lead to herpetic ulcerations of the lip, the typical “ cold sore ”
Herpes Virus Diseases: Labialis
Herpes labialis (cold sore, fever blister)
HSV-1 & HSV-2 cause genital & oral-facial infections (cannot distinguish between the 2)
Reactivation of oral-facial HSV-1 infections are more frequent than oral-facial HSV-2
Recurrent triggers: stress, sunlight, illness, trauma (dental appts)
Prodromal : prior lesion appearance, burning, stinging, tingling sensations with slight swelling may appear
Clinical characteristics
Group of vesicles form and eventually ruptures & may coalesces
Crusting follows and healing may take up to 10 days
The lesions are infectious, with viral shedding
Care must be taken by the patient because autoinfection (to eye, nose, or genitals) is possible, as is infection of other people
Laser dentistry
Herpes Virus Diseases Labialis
Clinical management: Use patient-friendly terms such as
“ cold sore ” or “ fever blister ” or “ulcer” NEVER SAY
HERPES LESION!!
POSTPONE appointment for patient with active lesion
Explain problems that can occur
Irritation to the lesion can prolong the course & increase severity of the infection
Prodromal state MOST contagious!!
Latent infection of herpes simplex virus. Path of the virus traced from point of viral penetration on lip to establishment of latent infection in the trigeminal ganglion
Herpes Virus Diseases: Whitlow
Herpetic whitlow
HSV-1 infection of the fingers that results from viral entry through minor skin abrasions
Most frequently found around a fingernail
Prevention is with use of protective gloves during dental procedures
Extinct in dentistry with standard precautions
Herpes Virus Diseases
Ocular/Ophthalmic Herpes
Can be primary or recurrent infection in the eye from
HSV-1 or HSV-2
Transmission from splashing saliva or fluid from a vesicular lesion directly into an UNPROTECTED eye
Prevention: PPE
Herpes Virus Diseases HSV2
Herpes simplex virus type 2 (HSV-2)
Commonly known as genital herpes, but can also occur as an oral and ocular infections
Herpes Virus HSV3 Varicella-Zoster Virus
Varicella-zoster virus
1.
Chicken pox: highly contagious, may be transmitted by direct contact, droplet
(possibly air-borne), or indirect contact with articles soiled by discharge from vesicles and the respiratory tract.
2.
Shingles: chickenpox leaves lasting immunity, but the VZV remains latent in the dorsal root ganglia. Secondary infection.
Herpes Virus HSV4: Epstein-Barr Virus
EBV virus causes:
1.
Infectious mononucleosis
• Prevention: minimize contact with saliva by frequent handwashing, avoiding drinking from a common container, follow standard precautions
2.
Oral hairy leukoplakia
• High incidence in HIV/AIDS patients
• Tongue lesions appear as white linear lesions along the lateral borders
Infectious Mononucleosis
Oral Hairy Leukoplakia
Herpes Virus HSV5 Cytomegalovirus
Cytomegalovirus (CMV)
Common in HIV/AIDS
Most severe form developing in infants affected in utero
Transmission
• Virus from mother may affect infant in utero, in birth canal, through breast milk
• Blood transfusion, post-transplant infection, sexual, respiratory droplet (daycare rate high)
Prevention
• Standard precautions, handwashing
HSV8
Kaposi’s sarcoma-related herpes virus in immunocompromised host
Major cofactor in production of Kaposi sarcoma
“AIDS-defining” lesion
HSV TYPE VIRUS
HSV 1
HSV 2
HSV 3
HSV 4
HSV 5
HSV 8
DISEASE
Varicella-zoster Chicken-pox
Shingles
Epstein Barr Mono
Oral hairy leukoplakia
Cytomegalovirus
Ulcers eyes, fingers, mouth, genitals
Ulcers genitals
Kaposi Sarcoma
HIV
HIV-1 Infection
• General facts
• First recognized in 1981 as cluster of diseases characterized by loss of cellular immunity
• Major types
1.
HIV-1 (more prevalent in U.S. & Europe)
2.
HIV-2
• Can persist within cells such as macrophages (WBC) for long periods
Transmission: semen, vaginal secretions, breast milk, blood
Serological tests:
Diagnosis: ELISA, confirmed with Western blot or IFA test
T-helper cell % marker for progression
Review
Which of the following tests determines the progression of
HIV?
a.
IFA b.
T-cell % c.
Western blot d.
ELISA
Review
Which of the following tests determines the progression of
HIV?
a.
IFA b.
T-cell % c.
Western blot d.
ELISA
Review
The majority of cases of transmission of HIV in adults is due to which of the following?
A) Blood transfusion
B) Needle sharing
C) Sexual contact
D) Contact with saliva
Answer
C) Sexual contact is the correct answer.
Sexual contact is the most common way HIV is transmitted among adults. Transmission via blood transfusions is rare, especially in developed countries.
Needle sharing is a method of transmission, but not as common. No cases of transmission via saliva are known.
Clinical Course of HIV-1
Seroconversion = when antibody can be detected
6wks-6mo after exposure
Incubation period: Range from time infection → AIDS symptoms
Could be 15+yrs
Clinical Course of HIV-1
Early symptomatic HIV disease
CD4+ T lymphocytes 200-500 cells; continued increase in viremia;
Many systemic symptoms
Late-stage disease: AIDS
CD4+ count below 200
Pneumonia common cause of death
• Death in 1 to 3 years (if untreated)
Oral Manifestations of HIV-1
Extraoral examination: Lymphadenopathy, Skin lesions
Intraoral examination
Fungal infections: Candidiasis
Viral infections: Kaposi Sarcoma, Herpes, Oral Hairy Leukoplakia,
Chickenpox, Verrucca vulgaris, HPV, Cytomegalovirus
Bacterial infections: Linear Gingival Erythema, NUG/NUP
Dental hygiene management: Refer symptomatic patients, help maintain quality of life, educated on home care
Prevention of HIV Infection
Community education
Goals
Primary prevention: lower incidence rate
HIV testing required for all pregnant women, all newborns
Secondary prevention: For seropositive individuals to reduce the rate of transmission and introduce treatment early.
Early intervention may postpone severe clinical manifestations of advanced illness
Factors to Teach the Patient
Postpone visit due to herpes infection
Don’t touch/scratch lesion
Avoid transferring virus to objects
Keeping medical history up-to-date
Maintaining oral health