Addison's, Cushing's & Acromegaly
advertisement

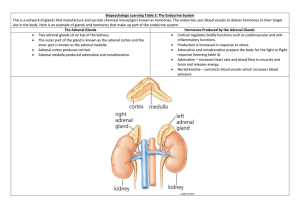
Definitions Aetiology Presentation Investigations Complications Management Prognosis Clinical scenario Definition Autoimmune destruction of the adrenal gland resulting in failure of adrenal steroid hormone production Cortisol & Aldosterone Adrenal failure: 1. Primary adrenal failure › 2. Secondary adrenal failure › 3. Atrophy/destruction of the adrenal gland Inadequate ACTH production Tertiary adrenal failure › Failure of CRH production 1. Primary adrenal failure › › › › › › › Autoimmune ADDISON’S Infection (TB, HIV) Invasion from mets (lymphoma, breast, lung) Haemorrhage (anticoagulants, WaterhouseFriedrichsen Syndrome Infiltration (amyloid, sarcoid, haemochromatosis) Congenital adrenal hyperplasia Drugs (eg ketoconazole, phenytoin, rifampicin) 2. Secondary adrenal failure › 3. Acute steroid withdrawal Tertiary adrenal failure › › › › Chronic high dose glucocorticoid therapy Sarcoidosis Tumour Cranial irradiation Non-specific symptoms: › › › › Abdominal pain Nausea Diarrhoea Lassitude Dizziness › Due to postural hypotension Pigmentation › › › › Buccal Scars Palmar creases Generalised Hypoglycaemia › Cortisol is one of the main insulin antagonists Bed side › Lying and standing BP › ECG › Blood glucose Bloods › U+Es › Serum cortisol (best to be done in the morning) › Adrenal autoantibodies Imaging › MRI head › CT abdo Special tests › Short synacthen test (confirm the Dx) › Long synacthen test (test response of adrenals) Addisonian crisis Occurs when the physiological demand for these hormones exceeds the ability of adrenal glands to produce them › ie, patients with chronic adrenal insufficiency when subject to an intercurrent illness or stress Major or minor infections Injury Surgery Burns Pregnancy General anaesthesia Abrupt withdrawal of steroids Waterhouse-Friedrichsen syndrome Present with hypovolaemic shock and profound hypoglycaemia MEDICAL EMERGENCY! Chronic adrenal failure Glucocorticoid replacement › Hydrocortisone › Double dose if intercurrent illness, infection or surgery Mineralocorticoid replacement › Fludrocortisone Addisonian Crisis IV fluids High dose hydrocortisone Dopamine (if hypotension persists) Treat precipitant Monitor U+Es and glucose Hypothyroidism T1DM Pernicious anaemia Vitiligo Premature ovarian failure Cushing’s Syndrome definition: The clinical condition resulting from prolonged exposure to glucocorticoids from an exogenous or endogenous cause. Cushing’s Disease definition: The clinical condition resulting from prolonged exposure to glucocorticoids from a pituitary adenoma. Cortisol Endogenous ACTH dependent • • Pituitary adenoma • 70% • F>M Ectopic ACTH production • 14% • SCLC • Carcinoid tumour Exogenous ACTH independent • • • Adrenal adenoma • 10% Adrenal carcinoma • 5% Adrenal hyperplasia • 1% Steroid use Use whatever helps you remember! Catabolic effects Glucocorticoid effects Mineralocorticoid effects •Myopathy •Striae •Bruising •Osteoporosis •Diabetes •Truncal obesity •Supraclavicular fat pad •Hypertension •Hypokalaemia S – spinal tenderness W – weight (central obesity) E – easy bruising D – diabetes I – interscapular fat pad S – striae H – hypertension/hypokalaemia Bedside › 24 hour urinary free cortisol (to confirm Cushing’s syndrome) Bloods › U+Es (<3.2 suggests ectopic ACTH production) Imaging › MRI head (for pituitary adenoma) › CT chest (for SCLC) Special tests → to determine the cause › Serum ACTH › Dexamethasone suppression test Distinguishes the ACTH dependent causes Same as complications of steroid use A common question in Finals! If struggling to remember don’t panic! › What can they lead on to? › Eg Diabetes and its complications, cardiovascular disease, infections Treat the cause! Conservative Distinction: • Nelson’s syndrome – postadrenalectomy development of a locally aggressive pituitary tumour (corticotrophinoma) due to lack of negative feedback. › › › › Stop medications! Exercise Diet Smoking cessation › › › › Metyrapone (blocks cortisol synthesis) Ketoconazole (inhibits cytochrome P450) Mitotane (adrenolytic agent) → adrenal carcinoma Radiotherapy (adjuctive therapy/for relapse/if surgery inappropriate/in children – when pituitary adenoma) Medical Surgical › › › Trans-sphenoidal adenomectomy Bilateral adrenalectomy (can’t locate tumour/recurrence post-surgery) Removal of ACTH secreting tumour If treated very good prognosis › Resolution of physical features and psychological disorders › Follow up needed for osteoporosis, glucose intolerance, DM, HTN, subtle mood changes, obesity Untreated = <5 years › Cardiovascular disease › Infection Definition: A hormonal disorder that develops when the pituitary gland produces too much growth hormone during adulthood Pituitary adenoma (≈99%) Ectopic production (≈1%) › Usually a carcinoid tumour Pancreas Lung Adrenals Cause Pituitary adenoma Ectopic production GH secretion Insulin-like growth factors Arteriolar muscle hypertrophy Hypertension Anti-insulin effect Diabetes Soft tissue growth Big tongue Big lips Boggy palms Cardiomyopathy Colorectal cancer Sweat gland hypertrophy Excess sweating Bone growth Typical facies Usually a spot diagnosis Typical facies › › › › Prominent supra-orbital ridges Big ears, nose, lips, tongue Prognathism Wide separation of teeth › › › › › › › Headache Numbness/tingling in hands Excessive sweating Vision problems Hoarse voice Obstructive sleep apnoea Muscle weakness May complain of: Observe: As previous slide Hands: Size – compare with your own Thenar eminence – wasting Check median nerve sensation Sweaty? ‘Bogginess’ of palms Skinfold thickness – increased in active disease Ask for BP Neck Check for goitre JVP Visual fields and acuity Stand from seated position Bedside › › › › › BP Urine dip BM ECG Echocardiogram Bloods › IGF levels Imaging Distinction: • Random GH measurements not helpful because GH secreted in pulsatile manner. • False positives for OGTT + GH • Pregnancy • Puberty • Hepatic disease • Renal disease • Anorexia nervosa • DM › MRI head › Colonoscopy (if ≥50 years) Special tests › Oral GTT with GH measurement Conservative › Exercise › Diet › Smoking cessation Medical › › › › › Octreotide & Lanreotide (somatostatin analogues) Bromocriptine & cabergoline (dopamine agonists) Insulin Metformin resistance Pegvisomant (GH receptor antagonist) Radiotherapy (as adjuvant/when surgery inappropriate) Surgical › Trans-sphenoidal adenomectomy IGF Follow up: › Yearly GH & IGF-1 measurement + OGTT, visual fields, CV assessment. Hypertension (increased risk of stroke & IHD) Diabetes Cardiomyopathy LVH Colorectal cancer ≈5% associated with MEN-1 → Remember ‘3Ps’ › Parathyroid hyperplasia/adenoma › Pancreatic endocrine tumours › Pituitary adenoma Mortality increased 2-3x 28 year old woman is seen in outpatients. She has been referred by her GP who has been unable to find a cause for her symptoms. She has a 6 month history of intermittent abdominal pain which varies in site and intensity. She has also experienced some occasional diarrhoea. She feels generally weak and off her food. She has lost a stone over this period. On examination she has pigmented palmar creases and buccal mucosa but no other specific findings. Her BP is 100/70 lying down, you try to stand her to check it again but she feels dizzy and light headed and has to sit down. You check her BM and it is 2.9. Addison’s disease What are your differentials for this lady? How would you investigate her? How would you manage her? What are the complications of Cushing’s disease? What is the difference between Cushing’s syndrome and Cushing’s disease? Medicine at a glance Ask Dr Clarke Patient.co.uk Oxford handbook of clinical medicine www.mayoclinic.com Special thanks to Dr Thomas Marshall