Treatment

Chronic otitis and its management
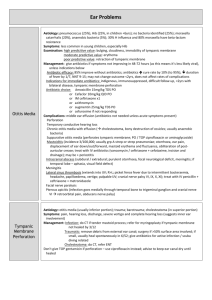
Otitis media chronica
(OMCH)
Chronic inflamatory changes on the eardrum, middle ear mucosa, ossicles, bone of the intercellular septs in the mastoid system, sometimes with the extension to the inner ear, facial nerve, middle andosterior fossa, sigmoid sinus etc.- complications
Classifications according to
Course – constantly, intermitently discharging ear, residua post otitidem
Localisation - epitympanic, mesotympanic, epimesotympanic OMCH
Extension of the pathologic changes – OMCH simplex ( changes on the middle ear and mastoid mucosa ), cum ostitide ( changes on the mucosa and ossicles, temporal bone event. ), cum cholesteatomate
( changes on the mucosa, bones and ossicles cause dby cholesteatoma )
Type of the discharge – serous, purulent, Otitis media with effusion
(OME)
Otitis media with effusion
(OME), Glue ear…
Chronic secretory otitis – OME - first staduim of the pathology continuing by adhesive – retraction process (retraction pockets) than cholesteatoma and or tympanosclerosis
Eustachian tube dysfunction followed by decreasement of the middle ear air pressure (resorbtion by the mucosa overweights the aeration via Eustachian tube that irritates the mucosa to produce the exsudate or transudate
Increasement of the resistence of the ossicular chain – conductive hearing loss.
Chronic changes in longer duration – mucosal metaplasia – cubic and spinocelular epithelium changes in cylindric with goblet cells that produce more viscous secretion creation of the cholesterin granulomas, hypertophia of the connective tissue in submucosal layers and finally complete transformation of the middle ear mucoperiost in the hyperplastic respiration type mucosa (with polyps in extreme cases) with Ig production enzymatic activity etc. This further accelerates the vitious circle of the deficit middle ear aeration
Time factor - If lasting longer than 3months – significantly increased the risk of the progressive adhesive – retraction process with retraction pockets and cholesteatoma creation
GER as one of the causes esp. In cleft palate population
OME, tympanostomy
OMCH without cholesteatoma
Chronic suppurative (purulent) otitis (Constantly +
Intermitently discharging ear)
Residua post otitidem (Constantly dry ear with perforation)
Symptoms:
Secretion
Conductive or combined hearing loss
Pain, ear fulness or pressure
Vertigo
Tinnitus
OMCH without cholesteatoma - perforation
OMCH without cholesteatoma
Pathogenesis
Infection via Eustachian tube or eardrum perforation
Mucosal inflammatory changes, ostitis, aseptic necrosis – vascular obliteration subepitelially – predilection - long process of incus anastomosis of r. stpadius
Important factors – tubal function, type and extension of the pneumatisation, communication between spaces – Prussak ś space, aditus ad antrum..(ahesive changes). Type and virulence of the pathogens, type and thickness of the mucosa.
Imunology + general conditions – allergy, diabetes,cachexia…
OMCH without cholesteatoma
Diagnostics
History – secretion, hypacusis, tinnitus,vertigo.. otomicroscopy central perforation, scarrs, incrustations (esp. p. tensa), mucosal changes
Imaging methods – X-ray Schueller , HRCT decreased pneumatisation, bone sclerotisation
Audiometry – conductive or combined heaing loss various grade
OMCH without cholesteatoma
Treatment – goal – to dry the mucosa
Conservative – evacuation of the secretion-suction the most important medicamentous – local – ATB drops (ciprofloxacine, gentamycine…) sometimes + corticosteroids
- decreasment of pH – Boric Acid in powder
Surgical – sanation and reconstruction phase if possible in one session
Extension of the sanation according to the extension of the pathology – tympanotomy, atticotomy, atticoantrotomy, atticoantromastoidectomy, petrosectomy
Reconstruction – tympanoplasty + reconstruction of the posterior canal wall
Course and prognosis : Attacks of secretion, minimal ostelysis – coomplications intracranial rare local unusual, good timing of surgery helps to avoid progression of destruction i.e. surdity and secretion
OMCH without cholesteatoma
Diff. Dg.
Cholesteatoma – marginal eardrum perforation typical otomicroscopy, HRCT finding
TBC – multiple eardrum perforation, more sever hypacusis including sensorineural
Tumours esp. Ca – marginal perforation accentation of pain, in initial stages difficult
OMCH with cholesteatoma
Symptoms
Pain
Putrid secretion
Progressive hypacusis , tinnitus vertigo
Pathogenesis
Differs according to the type of cholesteatoma (usually retraction – invagination of the thinned part of the eardrum and dislocation of the epidermal tissue to the middle ear + presence of the pathologic secretion) common features – proliferation activity of epidermal tissue accelerated by cytokins, progressive osteolysis caused by enzymatic activity (Collagenase, alc.phosphatase) in perimatrix and by activation and transformation of osteoclasts
Several types of cholesteatoma classification according to various criteria - primary, secondary (acquired), localisation …
Conditions for the cholesteatoma creation
Middle ear ventilation and drainage disturbance
Dislocated epidermal cells in middle ear in contact with mucosa
Increased proliferation tendency because of purulent inflammation
CHolesteatoma types
1.
2.
6.
7.
8.
9.
3.
4.
5.
Flaccida cholesteatoma (Epitympanic cholesteatoma attiku) retraction of Shrapnells membrane - attikus, event. aditus ad antrum, antrummastoideum, intersinofacial tract, processus mastoideus middle ear
Sinus cholesteatoma retraction of the eardrum superior posterior quadrant reaching sinus tympani, medially from the ossiclesin atticus,aditus ad antrum antrum,no anterior part of middle ear
Tensa cholesteatom retraction of pars tensa, reaching the supraubar recess anterior epitympanum and tubal ostium
Cholesteatoma of the external auditory canal dislocation of the epidermal tissue under the skin of the ext. Auditory canal – trauma, cleaning..
Posttraumatic cholesteatoma – epidermal tissue dislocated to the middle ear by trauma(often explosion
Congenital cholesteatoma (primary, occult, behind the intact eardrum…) from epidermoid tissue closed to the tubal ostium that survives from prenatal times
Residual cholesteatoma – after cholesteatoma surgery behind the reconstructed eardrum
Recurrent cholesteatoma – cholesteatoma after previous cholesteatoma surgery
Iatrogenic cholesteatoma – dislocation of the epidermal tissue behind the eardrum after previous non cholesteatoma surgery
Cholesteatomas
Cholesteatoma
Diagnostics
Otomicroscopy – charakteristic pearl appearance (if not covered by crust or polyp), marginal eardrum perforation, purulent secretion event.
Imaging methods –HRCT osteolysis, destruction of tegmen tympani, tegmen antri, lateral semicircular canal or Fallopian canal wall
Audiometry – conductive or combined hearing loss, .
Vestibulometry – asymetric finding +fistula sign can indicate destruction of the labyrinth – labyrinthine fistula
Treatment
Conservative treatment can calm the mucosa, suction can reduce the mass of cholesteatoma, but treatment of coice is surgical sanation
Course and prognosis
Non treated cholesteatoma can whenever cause the intracanial ol local life threatening complication
Specialcourse in children – the younger is the child the more rare nad agressive is the cholesteatoma. In elderly is higher tendency to asymptomatic and complicated course.
Diff dg.
OMCH without cholesteatoma, Tumour, TBC, WG otomicrosckopy, HRCT, sometimes surgery
HRCT – cholesteatoma of the pyramid apex
Approaches to the middle ear
Endaural
Endomeatal
Retroauricular
Retraction pocket
Retraction classification
Tensa retractions (Sadé)
1. Mild retraction without contact if the eardrum and IS joint
2. Eardrum in contact with IS joint
3. Eardrum in contactwith promontory without fixation
4. Eardrum in contact with promontorywith fixation
Bordered retractions - retraction pockets (Charachon )
1. Controlled pocket without fixation
2. Controlled pocket with fixation
3. Non controlled pocket with fixation
Flaccida retractions (Tos)
1.Mild retraction without contact to the malleus neck
2. Retraction in contact with malleus neck without bony erosion
3. Retraction in contact with malleus neck with erosion of scutum
4. Retraction in the contactwith the malleus neck and head and erosionof the scutum
Retraction pocket surgery
Goal –to resect or elevate non controlled or otherwise problematic retraction pockets via tympanotomy, atticotomy or atticoantrotomy to prevent the creation of cholesteatoma in retraction pocket
Preventive surgery
Surgical anatomy of the middle ear
Surgical anatomy of the middle ear
Surgical anatomy of the middle ear – sinus tympani
Surgical anatomy of the facial nerve
Surgical sanation
Lege artis always using microscope (rarely endoscope)
Extention according to the pathology of the finding.,the goal is to remove the cholesteatoma completely in toto
Principles of minimum invasive surgery former tympanomastoidectomies and radical operations are very rare, nearly abandonded
Restitution of „normal“ anatomic conditions if possible - trepanation cavity is divided from external auditory canal by its posterior wall – closed technique
Either the posterior canal wall is left intact - canal wall up (CWU) surgery – worse view –primary closed technique
Or the posterior wall is drilled out – better view and in the end of surgery reconstructed (cartilage, bone usually autologous or ionomer cement) – secondary closed technique
Closed technique enables better postoperation comfort of the patient
(swimming, diving,no infection from outwards to the trepanation cavity) and better hearing results.
Surgical sanation
Alternative solution not very suitable in cholesteatoma because of bad control and ossiblemuscle atrophy for opened cavities is obliteration by muscle flaps – Palva´s,m. temporalis flap, cartilage, bony or ionomer cement particles
Second – look – in closed technique surgery (especially secondary) in cases of large or problematically localized cholesteatomas is second surgery check up after 12 months indicated. The aim is to remove event. persistent cholestatomaby minimum invasive means until.it makes a large destruction. Sometimes endoscopically, indication as a matterof discussionV
If no security of sanation is reached, in extreme cholesteatomas andin complications trepanation cavity is left open to to the external auditory canal – opened technique more secure, worse hearing results, discomfort for patient
Extension of the surgery -
Atticotomy Atticoantrotomy
Extension of the surgery -
Atticoantromastoidectomy
CWU CWD
CWU left CWD right
St.p. AAME CWD +
Reconstruction of the posterior canal wall by cartilage CT scans
Secondary closed technique
( CW reconstructed by cartilage) healed
Inflammatory Complications of OMCH - local
Mastoiditis
Extension of the inflammation from the mucosa to the bone of the mastoid cell septs
Pathogenesis
The further inflammatory changes extension from mucosa to the bone depends on :
–anatomical conditions – narrow aditus ad antrum – wrong aeration of the antrum
– patient ´s health (diabetes, renál, hepatal pathology, immunity etc.)
Diagnostics symptomatic trias – ear discharge, painful palpation of mastoid process and planum, oedema of the retroauricular fold sometimes modified by ATB therapy
Otomicroscopy vidíme perforation of eardrum or posterior wall of the canalpurulent scretion, descensus of the wall
Otapostasis or Oedemas of the zygomatic, or lateral collar triangle in abscesses – subperiostal, rare cases -. Bezold, Mouret,
Moure´s
Blood count Leukocytosis, elevated sedimentation + CRP
Imaging methods X ray Schuller or Stenvers projection, HRCT osteolysis of mastoid cellar septa, obstruction of the mastoid cells měkkotkáňových hmot, tekutiny a osteolýzy sept sklípků je nejspolehlivějším zobrazením
Treatment
Cortical mastoidectomy AAME resp., ATB general and local administration.
Course and prognosis
Sometimes very rapid in hours, sometimes weeks, prognosis in adequate surgical treatment good, if non treated - high risk of complications
Diff dg.
Mastoidismus in external otitis (no elevation of the lab. Values, no finding on imaging methods)
Labyrinthitis
Symptoms
Peripheral vertigo, tinnitus, sensorineural or mixed hypacusis
Pathogenesis
Toxin or pus diffusion via oval or round window membrane or perilyphatic fistula (cholesteatoma, fractures of temporal bone, iatrogenic trauma).
Diagnosis
Otomicrscopic finding of discharge, cholesteatoma, fracture resp. together with typical cochleovestibular symptoms
Treatment
Medicamentous -Antibiotics, vazodilatators, corticosteroids i.v., middle ear drainage via paracentesis (in serous labyrintitis)
Surgery – mastoidectomy in facial nerve palsy, intracranial complication, perilymphatic or liquor fistula, cholesteatoma, Mastoidectomy + labyrinthectomy in purulent labyrinthitis Course and prognosis
Differs according to the form, extension and complications Diferenciální diagnostika
M. Menière attack, SHL , Acute vertigo – normal otomicroscopy finding, no otitis
Complications intracranial
Epidural empyema – non specific sympotms,
Otogenic meningitis Cefalea, nuchal stiffening, lost of the consciousness,. Restlessness, tonic- clonic spasms.
spread of the infection through lytic bone of tegmen antri or tympani or via perforator canals, through labyrinth (in labyrintitis, internal auditory canal, vv. Diploicae (in tromboflebitis) - meningitis
Diagnosis - HRCT, neurologic investigation, liquor analysis – increased proteins, decreased glucosa, chlorid ions- meningitis.
Every unclear meningitis is potentially otogenic – i.e. otogenic (and sinogenic) origin must be excluded!
Treatment
Mastoidectomy, exposition of the dura, drainage , I.v. ATB
Course and prognosis
Good in case of adequate and in time surgical treatment .
Complications intracranial
Otogenous sigmoid sinus thrombosis
Septicaemia + non specific symptoms (headache, septic T curve, nuchal stifness..)
Infection spreads in the dissolved bone to the sinus, there perisinous absces, phlebitis, creation of thrombs that growtowards sinus transversus and sagittalis, and to jugular vein bulb , emissaria mastoidea (Griesinger ´s sign)
Diagnosis septicaemia in chronic otitis , painful induration of VJI, splenomegaly, HRCT
Every unclear septicaemia is potentially otogenous(or tonsillogenous)
– must be excluded!!!
Treatment – mastoidectomy + exposition of the sigmoid sinus , iv.
ATB, heparin
Course and prognosis
80 % cured in adequate in time treatment
Complications intracranial
Otogenous brain abscess
Symptoms – meningism, cefalea, nausea, febrilities – first stage, second stage – non specific, third stage psychiatric changes + topical changes aphasia, ataxia alexia, agraphia , nystagmus , III.-VIII n. palsy etc.
Pathogenesis
– direct infection spread in lytic bone through tegmen tympani, antri..
– preformed spaces – int. auditory canal, vv. diploicae
Diagnosis
Neurootology, neuroophtalmology, neurology incl. EEG + liquor analysis,
HRCT, MRI
Treatment Surgery AAME + neurosurgery – exstirpation of the abces or evacuation of pus + ATB, corticosteroids
Course and prognosis rare complication with 20% mortality even though adequately treated, frequent residual neurological disordes
Diff. Dg. Intracranial Tu, Multiple sclerosis, in cerebellar a. labyrintitis, vestibulopathy
Complications intracranial
Petrositis
Symptoms Otorrhea, trigeminal neuralgy, abducens palsy+ diplopia
– Gradenigo ´s sy, vertigo, surdity pain „deep in head“
Pathogenesis – spread of infection medially to the hyperpneumatised pyramid to the supra, perilabyrinthine and apical tract (that are not in normal pneumatisation fully developed) osteomyelitis of the pyramid apex, lesions of the V and VI. Th cranial nerve and VII., IX., and X. event. + labyrintitis event.
Diagnosis Gradenigo trias + Imaging methods - Schueller, Stenvers projection, HRCT.
Neurology, Ophtalmology
Treatment – Surgery – mastoidectomy, labyrinthectomy, drianage of the apical cells + ATB, corticosteroids
Course and prognosis rare complication with quite good prognosis quoad vitam in early dg. and adequate treatment frequent neurology deficits after healing – localised meningitis in pontocerebellar angle