New Nutritional Approaches for the Treatment of Hyperlipidemia
advertisement

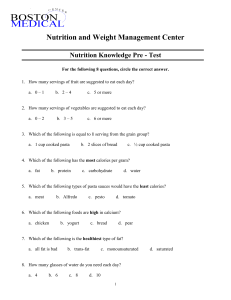
New Nutritional Approaches for the Treatment of Hyperlipidemia Laura S. Kinzel, M.S., R.D. October 3, 2001 Intervention Most successful when tailored to specific stages of change, goals, and challenges Effort is worthwhile: changes can be made and are an important adjunct to other therapies for CVD Incorporates lifestyle changes (+ drug therapy) Optimizing Change Team approach: time spent w/RD + Cognitive-behavioral approach: correlated with degree stages of change of cholesterol lowering goal setting 3 visits: 88% post-MI contracting at Step II diet at 90 self-monitoring days after admission stimulus control type II DM: any reinforcement contact w/RD feedback produced better individualization medical outcomes What Motivates Change? Ernst, D; Berg-Smith S; Brenneman, D; Johnson M. WHI Intensive Intervention Protocol, August 1999 If you are told what to do, there is a good chance that you will do the opposite People want to feel in control Values and beliefs Link behavior change to core values Beliefs more influenced by what you hear yourself say than by what is said to you One’s own reasons are most persuasive What Motivates Change, cont. Ambivalence is normal Stage of change: Contemplation Weighing pros/cons of choice can help Decisional balance Knowledge/perceived harm or benefit Provide personal feedback, advice and/or education Need to believe it can be done Voice confidence in patient’s ability to change Interaction between provider and client powerfully influences resistance, compliance and change Never underestimate the power of relationship % of the Treatment-Eligible Population Receiving Treatment (Hoerger et al. Amer J Cardiol 1998;82:61-5 Receiving Diet Receiving Drug Receiving No Rx < 2 Risk Factors > 2 Risk Factors CHD 33% 26% 29% 2% 6% 13% 64% 68% 58% Adapted from McKenney JM and Becker DM: Conference presentation at Advances in Cholesterol Management, June 3-5, 2001 New Features of ATP III Modifications of Lipid and Lipoprotein Classification Identifies LDL cholesterol <100 mg/dL as optimal Raises categorical low HDL cholesterol from <35 mg/dL to <40 mg/dL Lowers the triglyceride classification cutpoints to give more attention to moderate elevations (normal: <150 mg/dL) ATP III: More Therapeutic Options Plant stanols/sterols (2g/day) Increased viscous (soluble) fiber (10-25 g/day) Weight reduction Increased physical activity Third Report of the National Cholesterol Education Program Expert Panel on Detection, Evaluation, and Treatment of High Blood cholesterol in Adults (Adult Treatment Panel III). NIH Publication No. 01-3670, May 2001. Maximizing LDL Reduction Platt R; Prev Cardiol. 2000;3:83-87 Intervention Component LDL Reduction Estimates (%) amount/type of fat dietary cholesterol weight loss 10-25 functional foods 5-15 pharmacological intervention 25-50 (loss of 10 lbs.; elimination of excess kcal) (stanols/sterols; soluble fiber; soy protein; n-3 fatty acids) 5 Nutrient Composition of Therapeutic Lifestyle Changes Diet (ATP III, May 2001) Nutrient Recommended Intake Saturated fat <7% of total calories Polyunsaturated fat Up to 10% total kcals Monounsaturated fat Up to 20% total kcals Total fat 25-35% of total kcals Carbohydrate 50-60% of total kcals Cholesterol <200 mg/day “First Line” Approach Starting point for those with hyperlipidemias who are overweight: Lower total fat to approximately 25% to promote weight loss Emphasize low saturated fat intake Carbohydrate: Promote complex sources and high soluble fiber Tailor to individual medical/lifestyle needs Carbohydrate Controversy: HighCHO, Low-Fat Eating Patterns Hypertriglyceridmeia associated with risk ASHD Austin MA et al. Am J Cardiol 1998;81:7B-12B Gotto AM Am J Cardiol 1998;82:22Q-25Q Miller M Eur Heart J 1998;19(suppl):H18-22 High CHO, low fat eating patterns linked to hypertriglyceridemia, as well as to low HDL Added CHO (not removal of fat): hypertriglyceridemia More CHO, less fat = greater in TG when isoenergetic, remaining elevated for at least several months Weight loss, fiber,physical activity modify TG response Parks, EJ and Hellerstein MK Am J Clin Nutr 2000;71:412-33 Metabolic Syndrome: > 3 Risk Factors enhance risk for CHD at any given LDL cholesterol level (ATP III, May 2001) Risk Factor Abdominal Obesity Men/Women Triglycerides HDL Cholesterol Men/Women Blood Pressure Fasting Glucose Defining Level Waist Circumference >102 cm/>88cm 150 mg/dL <40 mg/dL/<50 mg/dL 130/85 mmHg 110 mg/dL Metabolic Syndrome Control LDL cholesterol (lifestyle + drugs) weight and physical activity : lower LDL, raise HDL improves insulin resistance, cardiac fitness Consider modifying eating pattern further: Moderate CHO, high fiber, low sugar ~30% fat (low sat. fat, high MUFAs) which may promote LDL and HDL Nydahl MC et al. Am J Clin Nutr1994;59:115-22 Lichtenstein AH et al. Arterioscler Thromb. 1993;13:1533-42 Reaven P et al. Am J Clin Nutr 1991;54:701-06 High-CHO, Low-Fat Diets… Do incremental increases in carbohydrate and gradual decreases in fat attenuate the rise in triglycerides? High-CHO, Low-Fat Diet: Lower Plasma Lipids and Lipoproteins w/o Producing HyperTG? Ullmann D et al. Arterioscler Thromb 1991;11:1059-67 Phases (10 days each) Composition Control 1 2 3 4 CHO(%) 45 50 55 60 65 Fat (%) 40 35 30 25 20 P:S ratio 0.4 0.7 1.0 1.3 1.6 Cholesterol 179 143 107 71 36 (mg/1000 kcal) High-CHO, Low-Fat Diet: Lower Plasma Lipids and Lipoproteins w/o Producing HyperTG? Ullmann D et al. Arterioscler Thromb 1991;11:1059-67 Cholesterol Levels % kcals as CHO 1 50 Phases 2 3 55 60 4 65 P values for ANOVA Total 223+15 216+15 209+14 198+13 0.0001 VLDL 43+7 41+6 41+5 42+7 0.9280 LDL 144+16 141+16 134+14 126+15 0.0001 HDL 43+4 41+3 44+4 36+3 0.0190 High-CHO, Low-Fat Diet: Lower Plasma Lipids and Lipoproteins w/o Producing HyperTG? Ullmann D et al. Arterioscler Thromb 1991;11:1059-67 TG Levels P values for ANOVA Phases 1 2 3 4 50 55 60 65 Total 23237 23730 23037 23035 0.7042 VLDL 16942 17137 17146 15737 0.9280 %CHO High-CHO, Low-Fat Diet: Lower Plasma Lipids and Lipoproteins w/o Producing HyperTG? Ullmann D et al. Arterioscler Thromb 1991;11:1059-67 Investigators’ conclusion: Although sudden increases in dietary carbohydrate often lead to increases in triglyceride levels, a high-CHO, low-fat eating pattern fed gradually may achieve significant reductions in total- and LDLcholesterol without carbohydrate-induced hypertriglyceridemia A very low-fat diet is not associated with improved lipoprotein profiles in men with a predominance of large, low-density lipoproteins Dreon DM et al. Am J Clin Nutr 1999;69:411-18 Previous work: (FASEB J 1994;8:121-6) phenotype A men (larger LDL) on 40% fat diet show less benefit with 22% fat than men with phenotype B (small, dense LDL) 1/3 phenotype A on high fat converted to phenotype B when switched to low fat eating pattern 38 men with phenotype A, after being on both 40% and 22% fat diets for 4-6 wk, on 10% fat diet x 10 days Replaced fat with carbohydrate No change in cholesterol content or ratio poly:sat fat 12 converted to phenotype B (change group) LDL did not differ from 22% fat diet in either group Higher TG, apoB, more small LDL, less HDL and apoA-I In this subset, changes are suggestive of coronary risk Summary Notes: High-CHO, Low-Fat Patterns Lower fat eating patterns optimize weight loss and LDL reduction Weight reduction, fiber and physical activity attenuate rise in triglycerides Rise in triglycerides may be transient Certain individuals may have improved response to moderate CHO intake, combined with careful use of mono- and polyunsaturates Incremental increases in CHO may help blunt potential rise in triglycerides