A Taxonomy of Research Design Peter T. Donnan Professor of
advertisement

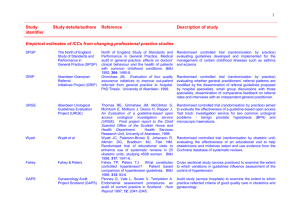
Statistics for Health Research A Taxonomy of Research Design Peter T. Donnan Professor of Epidemiology and Biostatistics Objectives of session • Realise importance of design • Understand difference between • • • experimental and observational design Choose appropriate design Understand main forms of experimental design Understand main forms of observational design Why is design important? • Poor design may not answer question • Choice of design determines the type of analysis • Incorrect design leads to waste of resources • Poor design is unethical if patient exposed to danger for little return A Taxonomy of Research Design • Experimental Randomised Controlled Trials Factorial design Crossover Cluster randomisation n.b. All are prospective since following experimental units forward in time A Taxonomy of Research Design • Non-randomised - Observational 1) Cohort (Prospective and Retrospective) 2) Case-Control 3) Cross-sectional 4) Time series RANDOMISED CONTROLLED TRIAL (RCT) •Gold standard method to assess Efficacy of treatment or demonstrate causal relationship •First proper clinical trials from 1940s in tuberculosis •Ethical requirements set out in Declaration of Helsinki, 1960 RANDOMISED CONTROLLED TRIAL (RCT) Random allocation to intervention or control so likely balance of all factors affecting outcome Hence any difference in outcome ‘caused’ by the intervention Randomised Controlled Trial Eligible subjects RANDOMISED Intervention Control RANDOMISED CONTROLLED TRIAL (RCT) •RCT necessary to demonstrate efficacy •Cost-effectiveness (ICER) •NICE and SMC assessment for recommendation to NHS Examples of RCT •Trials of tamoxifen for treatment of early breast cancer1 •Reduction in recurrence of 29% •Reduction in mortality by 14% in women with oestrogen receptor positive cancers •Trial published recently in Lancet on herceptin (trastuzumab) 1. Lancet 1998; 351: 1451-67. RANDOMISED FACTORIAL DESIGN Patients are randomised more than once All possible combinations of interventions are studied Simple 2-way factorial has 4 combinations Randomised Factorial Trial Eligible subjects RANDOMISED Intervention 1 RANDOMISED Intervention 2 Control 2 Control 1 RANDOMISED Intervention 2 Control 2 Example factorial design • Scottish Trial of steroids or acyclovir in Bell’s Palsy • Recruited 500 patients 1. Steroids / Placebo 2. Steroids / Acyclovir 3. Acyclovir / Placebo 4. Placebo / Placebo Strengths and Weaknesses of factorial design • Efficient – two trials for the price of one • Relies heavily on assumption of no interaction between treatments i.e. effects of treatments are additive • Results – Sullivan, Swan, Donnan et al, Early treatment with prednisolone or acyclovir and recovery in Bell’s palsy. NEJM 2007; 357: 1598-607 Crossover designs •In this design each patient receives ALL treatments •Order of receipt is randomised •Requires a wash-out period between treatments •Only applicable to transient effects in chronic conditions e.g. asthma, pain Crossover Trial Eligible subjects RANDOMISED Intervention Wash-out Control Wash-out Control Intervention Example of Crossover Trial •2-period 2-treatment trial of acarbose vs. placebo in type 2 diabetes •Mean difference in HbA1c was 0.3% with SD of 0.5% •No significant effect Strengths and Weaknesses of crossover design • Within patient characteristics remain same as matched analysis • Smaller sample size needed compared with parallel design • Not suitable for intervention that ‘cures’, used in chronic pain, asthma, diabetes. • Carry-over effect needs wash-out period Senn S. (1993) Crossover trials in clinical research. Chichester, John Wiley CLUSTER RANDOMISATION Man is a unit of the greater beasts, the phalanx. The individual relates to the large unit or phalanx John Steinbeck WHY USE CLUSTER RANDOMISATION? •Intervention at the group level e.g.new appointment system in general practice •Sometimes only practical design •Can reduce contamination •Easier to implement intervention (e.g counselling to reduce smoking) Intervention at practice level & effects on patients Practice level IMPLICATIONS OF USING RANDOMISATION BY PRACTICE? Sample size needs to be inflated: Subjects within practice more alike than subjects in different practices so independence assumption of statistical tests is incorrect IMPLICATIONS OF USING RANDOMISATION BY PRACTICE? Sample size obtained with no clustering is inflated by factor: IF = 1 + (m - 1) ρ Where is the intra-cluster correlation and m is the mean cluster (practice) size Inflation or DESIGN EFFECT depends on size of intra-cluster correlation Assume 40% reach lipid target on new statin and 30% on old statin •Total(ind) Inflation 1 Total(Cl) • 944 0.000 944 •944 •944 0.001 0.01 1.029 1.29 1218 •944 0.05 2.45 2312 971 How do you know degree of intra-cluster correlation? •Obtain from pilot work •Previous published values •HSRU, Aberdeen Outcomes 0.05 Process 0.05 – 0.15 IMPLICATIONS OF USING RANDOMISATION BY PRACTICE? Ethical issues: Cluster-cluster – guardian decides on behalf of all patients Cluster-individual – both patient and GP decide on consent IMPLICATIONS OF USING RANDOMISATION BY PRACTICE? Analysis: Need to take clustering into account e.g. Multi-level modelling Study Design - Observational •Cohort •Case-Control •Cross-sectional survey •Time series Walker & Stampfer ...”should not denigrate the observational nature of the data. Most of what we learn, and will continue to learn, about adverse drug effects are from observational studies” Lancet 1996;348:489 Cohort Design A cohort consists of a group of individuals from a well-defined population (exposure and characteristics known) followed up over time to observe what happens to which groups and when n.b.sociologists call these panels How many smokers and nonsmokers died? Non-smokers Smokers Events Simple Cohort study Smokers vs. non in Tayside population Non-smoker 1/1/2006 TIME Framingham cohort study Followed up 5,573 people white, initially free of CVD, but including people with hypertension and diabetes from 1968 onwards Developed predictive algorithms for CHD Summary Statistics in Cohort Study •Drug safety study of NSAIDS and hospitalisation for GI bleed •Rate of hospitalisations for GI bleed in NSAID and non-NSAID users over 1 year •Relative risk (RR) is ratio of rates Relative Risk Hosp GI bleed Yes No Exposed NSAIDS a b Unexposed c d RR = a/(a+b) / c/(c+d) Example Relative Risk Hosp GI bleed Yes No Exposed NSAIDS 136 4,390 Unexposed 2,104 126,060 RR = a/(a+b) / c/(c+d) = 1.83 Example Relative Risk Risk in exposed = 136/(136+4390) = 0.0300 or 30 per 1000 people Risk in unexposed = 2104/(2104+126060) = 0.0164 or 16 per 1000 people Hence RR = 0.0300/0.0164 = 1.83 Interpretation RR = 1.83 and 95% CI (1.19, 2.82) which is highly statistically significant (p < 0.001) 83% higher risk of hospitalisation for GI bleed in those exposed to NSAIDS compared with those not exposed Limitations In reality subjects have different length of follow-up – so need event rates per person-years follow-up e.g. 30 events per 1000 person years Raw unadjusted rates and Relative Risk – Need to take account of confounding through regression Retrospective Cohort Design •In this design group of subjects or cohort is identified in the past •Follow-up is then to the present •Advantage that most data already collected and events have occurred •Cheaper to perform as do not have to wait long period before analysis Log-rank test generalised Wilcoxon 21 = 10.6, p = 0.001 21 = 7.5, p = 0.006 Donnan et al Prognosis following first acute myocardial infarction in type 2 diabetes: A comparative population study. Diabetic Med 2002; 19: 448-455. Case-Control Design •In this design group of subjects with disease or condition are identified (Cases) •Suitable Control group identified without the condition •Frequency of Exposure or risk factor compared in cases and controls Case-Control Design Past Unexposed Present CASES Exposed Unexposed Exposed CONTROLS Example of Case-Control Study •Early studies of leukaemia around nuclear power stations •Consumption of red meat and risk of colorectal cancer •Use of mobile phones and RTAs Case-Control Design •May be matched or unmatched •Selection of cases and controls prone to bias •Sometimes have both hospital and population controls •Ascertainment of exposure prone to bias (e.g. recall bias) •Relatively cheap to carry out but difficulties with confounding Cross-sectional survey Present Events Exposed Unexposed No Events Exposed Unexposed Cross-sectional Design •Both exposure and events measured at same time •Often questionnaire–based surveys •Prone to volunteer bias and poor response •Relatively cheap to perform •Main difficulty in ascertaining temporal direction •Examples are postal surveys such as census Time series •Can be considered a set of regular crosssectional surveys over time •Examples are rainfall on daily basis, performance of stocks and shares, no. of hospitalisations on daily basis •Requires sophisticated analyses which account for autocorrelation – ARIMA models •Interrupted time series can be powerful method of assessing change following policy or organisational changes Example Time series 9.00 Mean HbA1c (t2) 8.00 7.00 6.00 5.00 89 87 85 83 81 79 77 75 73 71 69 67 65 63 61 59 57 55 53 51 49 47 45 43 41 39 37 35 33 31 29 27 25 23 21 19 17 15 13 11 9 7 5 3 1 Month (1=Jan 1998) Change in mean HbA1c following introduction (vertical line) of web-based Managed Clinical Network for diabetes in Tayside Study Design What design could be utilised to answer following questions? •Mobile phone use and brain cancer •Effect of Herceptin on later stage breast cancer •Methadone and deaths in drug users •Intensive management of high risk patients to prevent emergency hospitalisation •Effect of MMR vaccination and development of autism Study Design •Design is critical to success •Design determines type of analysis •Remember ‘Chance favours the prepared mind’