File
advertisement

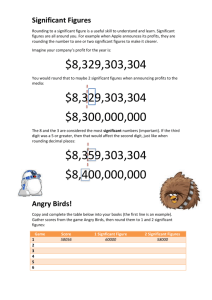
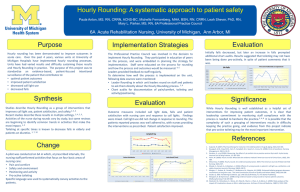
Running head: IMPACT OF HOURLY ROUNDING ON PATIENT FALLS The Impact of Nurse Hourly Rounding on Patient Falls An Integrated Literature Review Kristina A. Zurita University of Central Florida 1 IMPACT OF HOURLY ROUNDING ON PATIENT FALLS 2 Abstract Patients fall in the hospital is a significant problem that health care organizations are facing today. Falls are one of the leading causes of adverse events in the hospital and can cause injuryrelated deaths to the elderly population. Patient falls are also costing hospitals millions of dollars and insurance companies are no longer reimbursing for falls and related injuries that happened in the hospital. There is clearly a need for intervention to reduce patient falls and increase patient safety. Hourly rounding is being used as a means to answer this need. Hourly rounding is an autonomous intervention in which the nurse checks on the patient every hour to make sure basic needs are being met which includes assisting the patient to the bathroom to ensure safety. Since most patient falls occur in or near the bathroom, rounding has been indicated as a method to reduce fall rates. This integrative literature review aims to show the impact that nurse hourly rounding has on adult patient falls in the acute care setting. A literature search was conducted using a number of databases that yielded 10 articles that matched the inclusion/exclusion search criteria. The results showed that hourly rounding may decrease the incidence of patient falls in the hospital setting. Additionally, the research showed that hourly rounding may also increase patient satisfaction and decrease patient call light usage. Proper training, implementation, and commitment to the process are needed to ensure quality hourly rounding is being conducted. Overall, hourly rounding has been demonstrated to be an effective intervention that promotes patient safety and satisfaction, leading to better patient outcomes. IMPACT OF HOURLY ROUNDING ON PATIENT FALLS 3 Table of Contents Abstract…………………………………………………………………………………………..2 Significance and Background…………………………………………………………………….4 Research Question………………………………………………………………………………..5 Methods…………………………………………………………………………………………..5 Search Strategies……………………………………………………………………….....5 Definitions and Terms…………………………………………………………………….6 Inclusion/Exclusion Criteria………………………………………………………………6 Validity and Level of Evidence……………………………………………………….......6 Findings...…………………………………………………………………………………………7 Study Characteristics……………………………………………………………………...7 Sample Characteristics…………………………………………………………………….8 Themes……………………………………………………………………………….........8 Recommendations for Nursing Practice……………………………………………………........10 Conclusion……………………………………………………………………………………….11 References………………………………………………………………………………………..13 Appendix A………………………………………………………………………………………16 Appendix B………………………………………………………………………………………23 IMPACT OF HOURLY ROUNDING ON PATIENT FALLS 4 The Impact of Nurse Hourly Rounding on Patient Falls: An Integrative Literature Review Significance and Background The American Nurses Association-National Database of Nursing Quality Indications defines a fall as “an unplanned descent to the floor” (Tucker et al., 2012, p. 19). Patient falls can result in morbidity, mortality, and an increased fear of falling again and are one of the most common adverse events in the acute care setting (Tucker et al., 2012). The number of falls on an inpatient unit have been reported to range from 1.7 to 25 falls per 1,000 patient days (Tucker et al., 2012), with approximately 30% of these falls resulting in a serious injury (Goldsack, Bergey, Mascioli, & Cunningham, 2015). It is estimated that falls can cost hospitals $5,317 per patient fall and can cost $19,440 over one year period for an older adult patient fall (Tucker et al., 2012). By 2020, patient falls are projected to cost hospitals over $54 billion in direct and indirect annual costs (Hicks, 2015). The Centers for Medicare and Medicaid Services in 2008 recognized the financial costs of these falls and no longer reimburse hospitals for these conditions, stating that these falls could have been prevented (Hicks, 2015). The occurrence of patient falls now has an impact on hospital rankings as well as payment systems; therefore falls prevention has become of great interest to hospital administrators, nurse managers, and nursing staff (Goldsack et al., 2015). The majority of falls in the hospital setting have been reported to occur near the patient’s bed, in the room, or in the bathroom (Tucker et al., 2012). Most frequent falls are occurring during ambulation to or from using the bathroom or bedside commode (Tucker et al., 2012). Research shows that about one-third of falls could have been prevented (United States Department of Health and Human Services, 2015). Nurses can play an important role in preventing patient falls and maintaining patient safety (Cann & Gardner, 2011). There are a IMPACT OF HOURLY ROUNDING ON PATIENT FALLS 5 variety of interventions that have been studied and utilized in order to reduce patient falls: falls risk assessments, bed alarms, lab belts, direct observation, falls prevention agreements, and restraints. One of the most current interventions is the use of nurse hourly rounding to improve patient safety and prevent falls (Hicks, 2015). The use of hourly rounding has been noted to be a promising intervention in preventing patient falls (Tucker et al., 2012). It has been reported that hourly rounding can reduce patient falls as much as 50% in the acute care setting (Hicks, 2015). Hourly rounding has also been reported to increase patient satisfaction, reduce call-light use, reduce medication errors, and increase staff satisfaction (Cann & Gardner, 2011; Olrich, Kalman, & Nigolian, 2012). Research Question In the adult acute care setting, how does nurse hourly rounding impact patient falls? Methods Search Strategies A literature search was performed in a variety of databases, including Medline, Academic Search Premier, the Cochrane Database of Systematic Reviews, and Cumulative Index to Nursing and Allied Health Literature (CINAHL) Plus. The following keywords were used as search criteria: “adult”, “acute care”, “hospitalization”, “nurse”, “rounding/hourly rounding”, “falls/fall prevention” and “patient safety”. After conducting a search of peer-reviewed articles published from 2010-2015, 12 articles were found in CINAHL Plus, 10 articles in Medline, 12 articles in Academic Search Premier, and none were found in the Cochrane Database of Systematic Reviews for a total of 34 articles. 10 articles were used for this review based on the inclusion/exclusion criteria. IMPACT OF HOURLY ROUNDING ON PATIENT FALLS 6 Definitions and terms Hourly rounding can be referred to as “intentionally rounding”, “rounds”, “nursing rounds”, “comfort rounds”, “routine rounds”, “care rounds”, “Model of Care”, “patient-centered hourly rounding”, and “patient rounds”. Hourly rounding is the process of intentionally checking on the patient to addresses a patient’s basic needs by the nursing staff at regular intervals (Hicks, 2015). Hourly rounding by the nurse requires the nurse to assess the patient’s need to use the bathroom, repositioning, pain management, ensure a clean surrounding and patient’s personal items within reach, and telling the patient when the nurse will return to reduce patient anxiety (Mitchell, Lavenberg, Trotta, & Umscheid, 2014). Hourly rounding occurs every hour, though some hospitals utilize a 2-hourly rounding during the evening hours to minimize sleep disturbances of patients. Inclusion/Exclusion Criteria Articles that were included in this search addressed the adult population on an inpatient unit in a hospital, nurses who implemented patient hourly rounding on the unit and those who do not, and articles where patient safety and/or falls prevention was evaluated. Exclusion criteria consisted of articles that included pediatric patients, articles that focused primarily on leader rounding only or rounding by personnel other than the nurse, and studies that were conducted on outpatient or emergency department units. Validity of Findings and Level of Evidence Each of the 10 articles used in this literature review were assessed for validity using the Quelly tool (2007). Three studies yielded a score of 11 points (Hicks, 2015; Krepper et al., 2012; Spanaki, 2012), six studies scored 10 points (Cann & Gardner, 2012; Goldsack et al., IMPACT OF HOURLY ROUNDING ON PATIENT FALLS 7 2015; Kessler et al., 2015; Mitchell et al., 2014; Olrich et al., 2012; Saleh et al., 2011) and one study scored 9 points (Tucker et al., 2012). According to Quelly (2007), all of the articles used in this review were ranked a level 3, meaning they were high quality studies. The level of evidence was assessed based on the “rating system for the hierarchy of evidence for intervention/treatment questions” published by Melnyk & Fineout-Overholt (2011). Eight articles were ranked level III (Cann & Gardner, 2011; Goldsack et al., 2015; Kessler et al., 2012; Krepper et al., 2012; Saleh et al., 2011; Spanaki et al., 2012; Olrich et al., 2012; Tucker et al., 2012) and two articles were ranked level II (Hicks, 2015; Mitchell et al., 2014). Most of the studies used a pre/post implementation design. Findings Study Characteristics All of the articles included in this literature review were peer reviewed and ranked as Level II systematic reviews or Level III cohort/quasi-experimental studies. All ten articles addressed the impact that hourly rounding has on patient falls and some of studies stated other benefits of hourly rounding as well. All of the studies compared hourly rounding to the previous standard of care in the adult population. The measurement tool used for the cohort studies (Cann & Gardner, 2012; Kessler et al., 2012; Spanaki et al., 2012; Tucker et al., 2012) and the quasiexperimental studies (Krepper et al., 2012; Olrich et al., 2012; Saleh et al., 2011) were that of a pre/post evaluation design. The two systematic reviews (Hicks, 2015; Mitchell et al., 2014) evaluated studies of a pre/post design as well. The standard method of previous care for all studies was that of not using hourly rounding as a method of preventing patient falls. Five studies implemented a 2-hourly rounding protocol during the evening hours (Hicks, 2015; IMPACT OF HOURLY ROUNDING ON PATIENT FALLS 8 Kessler et al., 2012; Mitchell et al., 2014; Olrich et al., 2012; Saleh et al., 2011). The time periods for assessing the impact of hourly rounding varied among the studies, lasting as short as 30 days to as long as 6 years. The majority of the studies lasted about one year. Limitations to these studies included non-randomization samples, weak research design, small sample sizes, and variations in the length of time that these studies were conducted. Follow-up on these studies were also lacking. Sample Characteristics Of the ten studies reviewed, eight of the studies were conducted in the United States, one in Australia (Cann & Gardner, 2012) and one in Saudi Arabia (Saleh et al., 2011). The majority of the studies included both male and females of the adult population on medical-surgical units. One study was conducted on an all male stroke unit (Saleh et al., 2011), one on an epilepsy monitoring unit (Spanaki et al., 2012), and another study was done on an orthopedic unit (Tucker et al., 2012). The age range of these subjects was from 18 to 90 years old. The total number of participants could not be determined due to some studies not reporting the sample size. Themes Decreases patient falls. Nine of the studies reviewed concluded that some form of hourly rounding has a positive impact on reducing patient falls. Of these nine studies, two studies provided statistically significant results. Saleh et al. (2011) had 25 falls in a 4 week period prior to implementation and then only 4 falls during implementation of hourly rounding, (p < 0.01). Goldsack et al. (2015) compared two units that implemented hourly rounding. One unit had trained and actively engaging staff participating in hourly rounding, while the other unit IMPACT OF HOURLY ROUNDING ON PATIENT FALLS 9 had no training and non-compliant staff that did not engage regularly in hourly rounding (Experimental Unit: p=0.006, Control Unit: p=0.799). The other studies in this review showed increases in patient safety with the implementation of hourly rounding; however, they did not show statistical significance. Cann & Gardner (2012) used a “Model of Care” where hourly rounding was one component of a patientcentered quality improvement framework. There was improvement in falls post-implementation (p=0.500), but not enough to show significance. Kessler et al. (2012) and Olrich et al. (2012) had a decrease in the fall rate post implementation (p=0.07; p=0.672). Spanaki et al. (2012) and Tucker et al. (2012) also showed that hourly rounding reduces fall rates but did not report statistically significant results (p=0.694; p=0.088). The two systematic reviews showed that hourly rounding did have an effect on decreasing patient falls. Hicks (2015) found 10 studies where falls were decreased, 3 studies that showed no change and 1 study that had variations in the results. Mitchell et al. (2014) found 9 studies where the median fall reduction rate was 57% and two studies were able to report statistically significant decreases when hourly rounding was implemented. Krepper et al. (2012) showed that fall rates on the experimental and control units were similar and no conclusions could be made. Increases patient satisfaction. Five of the studies in this literature review addressed the impact that hourly rounding has on patient satisfaction. Cann & Gardner (2012), Kessler et al. (2012), Olrich et al. (2012), and Saleh et al. (2011) concluded that hourly rounding has the potential to increase patient satisfaction but none of the studies showed statistically significant data (p=0.081; not reported; p=0.383; p<0.05). One of the systematic reviews found 4 studies that showed statistically significant improvements in patient satisfaction (Mitchell et al., 2014). IMPACT OF HOURLY ROUNDING ON PATIENT FALLS 10 Decreases call light usage. Four studies in this review addressed the impact that hourly rounding has on patient call light usage. These studies revealed that hourly rounding significantly reduces the amount of times a patient presses the call light. Mitchell et al. (2014) revealed a median reduction of 54% in call light usage in 10 studies reviewed. Krepper et al. (2012), Olrich et al. (2012), and Saleh (2011) all stated statistically significant decreases in call light usage due to hourly rounding implementation (p=0.001; number not reported; p<0.001). Proper implementation and compliance is necessary for success. Four studies discussed the importance of how proper implementation is essential for hourly rounding to be successful (Goldsack et al. 2015; Kessler et al., 2012; Olrich et al., 2012; Tucker et al., 2012). Proper compliance by staff was also addressed in these four studies. Hourly rounding appears to be effective when the patient trusts that the nurse will return when he/she says they will (Olrich et al., 2012). If the nurse is not efficient in properly implementing the rounds, then the patient will not trust the nurse, therefore leading to a breakdown in the process (Tucker et al., 2012). Validation and consistency by those implementing hourly rounding is the key to success (Kessler et al., 2012). The buy-in, commitment, and accountability by the staff become a crucial component to hourly rounding (Goldsack et al., 2015). Recommendations for Nursing Practice The impact that patient falls have on hospital costs and overall patient well-being is significant. The evidence reviewed in these studies indicates that hourly rounding positively impacts the prevention of patient falls. Despite most of the evidence not demonstrating statistically significant results, there is a decrease in patient falls when hourly rounding is implemented. Using the Strength of Recommendation Taxonomy (SORT), the strength of IMPACT OF HOURLY ROUNDING ON PATIENT FALLS 11 recommendation for implementing hourly rounding to prevent patient falls in the acute care setting yields a recommendation A (Ebell et al., 2004). Of the ten articles reviewed, two Level II systematic reviews and seven Level III cohort/quasi-experimental studies all found that hourly rounding should be implemented as it may help nurses to keep patients safe by reducing patient falls. A number of studies reviewed showed evidence that hourly rounding does not only impact patient falls, but also plays a crucial role in reducing call light usage and increasing patient satisfaction (Mitchell et al, 2014). When patients believe in the process, they begin to build a trusting relationship with the nurse which may lead them to not use the call light as often because they know the nurse will be returning soon to care for their needs. Hourly rounding has a positive impact on reducing call light usage and increasing patient satisfaction which can lead to better patient outcomes (Mitchell et al., 2014). Hourly rounding may be more effective if proper nursing training and implementation is provided. Hourly rounding is an autonomous intervention that nurses can perform to keep their patients safe (Hicks, 2015). Without commitment and believability of the process, a positive outcome for hourly rounding is unattainable (Hicks, 2015). Hospital administration should be aware that for proper implementation of hourly rounding, special attention should be placed on training, promoting commitment to the cause, and compliance by nursing staff members (Olrich et al., 2012). Conclusion Hourly rounding is an autonomous intervention that nurses can easily implement to ensure patient safety and reduce patient falls. When nurses are trained properly and believe in IMPACT OF HOURLY ROUNDING ON PATIENT FALLS 12 the process and cause of the intervention, hourly rounding has been shown effective to increase a patient’s safe stay in the hospital. This review has also shown there are secondary benefits to hourly rounding, such as an increase in patient satisfaction and a decrease in call light usage. Hospital administrators and managers should consider implementing hourly rounding, as it may also reduce unnecessary hospital costs as a result of patient falls. This review demonstrated the benefits of hourly rounding in the acute care setting. Further longitudinal research may be beneficial to ascertain the sustained effects of hourly rounding. IMPACT OF HOURLY ROUNDING ON PATIENT FALLS 13 References Cann, T., & Gardner, A. (2012). Change for the better: An innovative model of care delivering positive patient and workforce outcomes. Collegian, 19(2), 107-113. doi:10.1016/j.colegn.2011.09.002 Ebell, M. H., Siwek, J., Weiss, B. D., Woolf, S. H., Susman, J., Ewigman, B., & Bowman, M. (2004). Strength of recommendation taxonomy (SORT): A patient-centered approach to grading evidence in the medical literature. Journal of the American Board of Family Practice, 17 (1), 59-67 Goldsack, J., Bergey, M., Mascioli, S., & Cunningham, J. (2015). Hourly rounding and patient falls: What factors boost success? Nursing, 45(2), 25-30. doi:10.1097/01.NURSE.0000459798.79840.95 Hicks, D. (2015). Can hourly rounding reduce patient fall in acute care? An integrative literature review. MEDSURG Nursing, 24(1), 51-55. Kessler, B., Claude-Gutekunst, M., Donchez, A. M., Dries, R. F., & Snyder, M. M. (2012). The merry-go-round of patient rounding: Assure your patients get the brass ring. MEDSURG Nursing, 21(4), 240-245. Krepper, R., Vallejo, B., Smith, C., Lindy, C., Fullmer, C., Messimer, S., & ... Myers, K. (2014). Evaluation of a standardized hourly rounding process (SHaRP). Journal For Healthcare Quality: Promoting Excellence In Healthcare, 36(2), 62-69. doi:10.1111/j.19451474.2012.00222.x IMPACT OF HOURLY ROUNDING ON PATIENT FALLS 14 Melnyk, B. & Fineout-Overholt, E. (2011). Evidence-based practice in nursing and healthcare: A guide to best practice (2nd ed.). Philadelphia: Lippincott Williams & Wilkins. Mitchell, M. D., Lavenberg, J. G., Trotta, R. L., & Umscheid, C. A. (2014). Hourly rounding to improve nursing responsiveness: A systematic review. The Journal Of Nursing Administration, 44(9), 462-472. doi:10.1097/NNA.0000000000000101 Olrich, T., Kalman, M., & Nigolian, C. (2012). Hourly rounding: A replication study. MEDSURG Nursing, 21(1), 23-36. Quelly, S. (2007). Determining quality and validity of findings. Saleh, B. S., Nusair, H., AL Zubadi, N., Al Shloul, S., & Saleh, U. (2011). The nursing rounds system: Effect of patient's call light use, bed sores, fall and satisfaction level. International Journal Of Nursing Practice, 17(3), 299-303. doi:10.1111/j.1440172X.2011.01938.x Spanaki, M. V., McCloskey, C., Remedio, V., Budzyn, D., Guanio, J., Monroe, T., & ... Schultz, L. (2012). Developing a culture of safety in the epilepsy monitoring unit: A retrospective study of safety outcomes. Epilepsy & Behavior: E&B,25(2), 185-188. doi:10.1016/j.yebeh.2012.06.028 Tucker, S. J., Bieber, P. L., Attlesey-Pries, J. M., Olson, M. E., & Dierkhising, R. A. (2012). Outcomes and challenges in implementing hourly rounds to reduce falls in orthopedic units. Worldviews on Evidence-Based Nursing, 9(1), 18-29. doi:10.1111/j.17416787.2011.00227.x IMPACT OF HOURLY ROUNDING ON PATIENT FALLS 15 United States Department of Health and Human Services. (2015). Preventing falls in the hospital. Retrieved from http://www.ahrq.gov/professionals/systems/hospital/fallpxtoolkit/ Running head: IMPACT OF HOURLY ROUNDING ON PATIENT FALLS 16 Appendix A Literature Table Citation Cann & Gardner (2012) Patient Group and Sample Size Study Design and Level of Evidence 29-bed surgical Pre/post test unit over a one design year period: Cohort study 1115 patients pre-implement, 1069 postLevel III implement Outcome Variables Comfort rounds, previous care, patient safety N=2,184 Key Results Validity DATA Per 100,000 patient Quelly score: 10 hours: Possible bias due Preto self reporting, implementation: no randomization 13.9 Large sample size PostAdequate length of implementation: time 10.9 Themes “Model of Care” (hourly rounding) increases patient safety “Model of Care” increases patient satisfaction. P=0.500 Not statistically significant Goldsack et al. (2015) Unit 1: 35 beds Unit 2: 40 beds Pre/post implementation evaluation Hourly rounding, previous care, nurse compliance, Unit 1: P=0.006 Quelly score: 10 Unit 2: P=0.799 Short pilot period, convenience sampling, no Hourly rounding is effective in falls prevention IMPACT OF HOURLY ROUNDING ON PATIENT FALLS For 30 days Cohort study 17 patient falls Statistically significant for Unit 1 randomization Staff compliance and leadership involvement is critical to implementation Hourly rounding, 2-hourly rounding, previous care, patient falls Fall rates decreased in 10 studies, unchanged in 3 studies, and varied in 1 study. Quelly score: 11 Hourly rounding has an effect on decreasing patient falls Hourly rounding, previous care, nurse compliance, patient safety Hourly rounding fall rate: 2.19% Quelly score: 10 Level III Hicks (2015) Kessler et al. (2012) 14 studies reviewed addressing fall rates Systematic Review of nonRCT Two critical care units and three medicalsurgical units Pre/post implementation surveys Level II Cohort study 6 year study Previous care fall rate: 5.46% P=0.07 Level III Not statistically significant No randomization, varying sample sizes, varying lengths of time Decrease in patient falls due to hourly rounding Length of time (6 year study), variations in staff members Hourly completing rounds, rounding can no randomization promote patient and staff satisfaction Staff compliance and continuation is key in implementation IMPACT OF HOURLY ROUNDING ON PATIENT FALLS Krepper et al. (2012) Two 32-bed cardiovascular surgery units 6-month study period, 6month post study A two-group quasiexperimental design Level III Quality/safety of patient care, hourly rounding with extensive training, hourly rounding with very little training, previous care 18 Prior to study: Experimental: 3.97 Control: 2.6 P=0.25 During study: Experimental: 2.68 Control: 2.42 P=0.70 6-montsh post study: Experimental: 2.42 Control: 1.43 P=0.07 Not statistically significant Quelly score: 11 No significant differences Small sample size, possibly due to no randomization infrequency of Adequate length of falls time Hourly rounding significantly reduced call light usage. IMPACT OF HOURLY ROUNDING ON PATIENT FALLS Mitchell et al. (2014) 11 studies reviewed, 9 studies focused on reduction of falls (pre/post test) Systematic review of nonRCTs Hourly rounding, 2-hourly rounding, previous care Level II 19 Reduction in falls ranged from 24%80%, with a median reduction of 57% 2 studies were able to report statistically significant decrease in falls rate Quelly score: 10 Variations sample size and length of time, no randomization, publication bias Hourly rounding reduces patient falls Reduction in call light use Improves patient satisfaction Improves patients’ perceptions of nursing staff responsiveness Olrich et al. (2012) Two med-surg units over 1 year N=4,418 Quasiexperimental Level III Rounding, previous care, patient falls Experimental unit: 23% reduction in falls, P=0.672 Control unit: falls increased Not statistically significant Quelly score: 10 Small sample size, no randomization, hospital-wide patient census decreased during study Hourly rounding decreased fall rates. Proper implementation is needed to gain positive results Hourly rounding has the IMPACT OF HOURLY ROUNDING ON PATIENT FALLS 20 potential to increase patient satisfaction Hourly rounding has the potential to decrease call light usage. Saleh et al. (2011) Male stroke unit (26 beds), 104 patients over 4 month period N=104 Quasiexperimental non-equivalent groups design Level III Hourly rounding, 2-hourly rounding, previous care, fall incidence Hourly rounding: 4 Quelly score: 10 falls during Short study period, implementation no randomization (second 4 weeks) Reduction in fall incidence due to hourly rounding Previous care: 25 falls prior to implementation (first 4 weeks) Hourly rounding yielded a significant reduction in call bell usage P<0.01 Hourly rounding reduced the occurrence of pressure ulcers Statistically significant Hourly rounding increased IMPACT OF HOURLY ROUNDING ON PATIENT FALLS 21 patient satisfaction Spanaki et al. (2012) 971 consecutive patients in a 4 year study on epilepsy monitoring unit Pre/post implementation evaluation Retrospective cohort study Hourly rounding, previous care, “falls prevention agreement” Two 29-bed postoperative orthopedic units Descriptive and repeated measures design Cohort study 2,295 hospitalizations Level III during study timeframe (682 baseline period, 775 intervention period, 838 post- Quelly tool: 11 Post: 7 falls Large sample size, adequate length of time for study, all patient data used on this specific unit, no randomization 15% reduction P=0.694 Level III Tucker et al. (2012) Pre: 12 falls Not statistically significant Fall rates, fall risk scores, hourly rounding fidelity, previous care Implementation vs. baseline: P=0.088 Postimplementation vs. baseline: P=0.375 Postimplementation vs. implementation: P=0.319 Not statistically significant Quelly tool: 9 Fidelity of implementation, no randomization, no control group, low baseline fall rates, large sample size Hourly rounding decreased fall rates Hourly rounding significantly decreased the amount of missed seizures Rounding reduces fall rates Proper and consistent implementation effects outcomes of rounding IMPACT OF HOURLY ROUNDING ON PATIENT FALLS intervention) 1 year study Primary Theme: Hourly rounding decreases patient falls. Secondary Themes: Hourly rounding increases patient satisfaction. Hourly rounding decreases call light usage. Proper implementation and compliance is necessary for the success of hourly rounding. 22 Running head: IMPACT OF HOURLY ROUNDING ON PATIENT FALLS Appendix B Determining Quality and Validity of Findings 1. Research question, hypothesis, or problem is clearly stated. 2. Purpose is clearly stated and relevant to research question or problem. 3. Review of literature and background evidence supports study purpose. 4. Research design is appropriate for research question or purpose. 5. Variables are appropriate for study purpose. 6. Methodology is strong and clearly stated. 7. Sampling method is appropriate and adequate in size and demographics to support external validity. 8. Instrument validity and reliability are appropriate and clearly described. 9. Data is collected and managed systematically. 10. Analysis of results is complete and sound. 11. Study limitations are acknowledged and described. 12. Conclusions are supported by analysis of findings. Each criterion receives 1 point and evaluated from total points as: Level 3 (High quality): 9 – 12 Level 2 (Moderate quality): 5–8 Level 1 (Low quality): 0–4 23