PowerPoint - GRECC Audio Conferences
advertisement

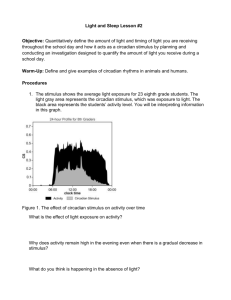
Rest-Activity and Light Exposure Patterns in Older Adults: Methodological Implications Thomas Hornick MD Patricia Higgins RN, PhD 1 Objectives Understand the influence of circadian rhythm disruptions on overall health. Identify clinical characteristics of circadian rhythm disturbances in older adults Recognize the importance of chronobiology in elders’ sleep-wake disturbances. Describe results from preliminary studies assessing the use of circadian light therapy in a nursing home unit and measurement of circadian light exposure in a case study of home-dwelling older adults. 2 Biological Rhythms Types of rhythms 1. 2. 3. 4. Ultradian (heart beat, respirations, appetite) Infradian (menstrual cycle) Circannual (annual breeding cycles) Circadian (sleep-wake cycle) Rhythms allow organisms to time events and anticipate change! 3 Arendt 2006 4 With Zeitgeber 5 Disruption of circadian rhythm • • • • Poor performance/fatigue (Reinberg et al, 2007, Laposky et al 2008) Weight gain(Knutson et al, 2007) Breast cancer (Stevens et al 2001) Other conditions 6 Why older adults? • • • Sleep disorders are common Complaints among caregivers of persons with dementia frequently revolve around disordered day/night cycles Medications for sleep are less safe in this population 7 Aging and light • Older adults spend much of their time in muted indoor lighting. • 35 minutes/day of bright light exposure compared to approximately 58 minutes of bright light per day for middle-aged adults. (Sanchez 1993) • Reduced light exposure compounded due to physiologic changes • senile meiosis, cataract formation, and/or increased light absorption by the crystalline lens. (Charmin 2003) • Attenuation of light exposure by more than 80% in normal older adults relative to young adults. 8 Age related losses in retinal illumination Turner et al Br J Ophthalmol. 2008 November; 92(11): 1439–1444 9 . Wikipedia, accessed 10/30/09 10 Role of Retinal Receptors Three known retinal receptors: process visual and circadian timing information Rods and cones: visual data Intrinsically photosensitive retinal ganglion cells (iPRGC): primarily light-dark data 11 Spectral sensitivity of photopic, scotopic and circadian (melatonin suppression) photoreception Turner et al Br J Ophthalmol. 2008 November; 92(11): 1439–1444 12 iPRGCs: History 1998: Melanopsin in light-sensitive cells on frog skin (Provencio et al, Proc Natl Acad Sci ) 2000: Melanopsin-containing cells found in retinal ganglion cell layer (Provencio et al, J Neuroscience) Most likely comprise the retinohypothalamic tract Sensitive to wavelengths in the 484-500 nm (blue light) 2002: Light responses from melanopsincontaining ganglion cells in humans (Berson et al, Science) 13 Intrinsically photosensitive retinal ganglion cells (iPRGCs) Timing Photoreceptors • Located throughout retina (~3000) • Express melanopsin • Blue light sensitive(peak 460nm) Regulate photoperiodism (sensitivity to length of day and night) • Higher excitatory threshold than rods/cones • Transmits to SCN 24-hour light-dark pattern on the retina is the most efficient stimulus for entrainment of circadian rhythms in humans • 14 Suprachiasmatic nucleus (SCN) is master pacemaker 1. 2. 3. 4. Activity in SCN correlates with circadian rhythms Lesions of SCN abolish free-running rhythms Isolated SCN continues to cycle Transplanted SCN imparts rhythm of the donor on the host 5. SCN is known to be compromised in older adults with dementia. (Harper et al 2008) 15 Role of Melatonin Melatonin • • Primary role in humans is to convey information about the daily light-dark cycle to physiological systems Peaks during sleep, suppressed by light. 16 Melatonin Rhythms and Aging Age 65-81, mean 68 Average (±SEM) plasma melatonin in young (top, n=90) and older (bottom, n=29) subjects during a normally phased sleep episode (closed boxes) and a constant routine where they remained awake at the same clock hours (open circles). Data were aligned such that each subject's wake time was graphically adjusted to 08:00 and the data from the baseline day and night and from the CR(constant routine) expressed relative to wake time; sleep time is from 24:00 to 08:00. Melatonin data were averaged hourly within and then across subjects Zeitzer et al Sleep. 2007 November 1; 30(11): 1437–1443. 17 Plasma melatonin suppression by bright light in 65 year old man Plasma melatonin data from subject 19G7, a 65 year old man who was exposed to a 3,527 lux light stimulus. Upper panel: plasma melatonin data from the initial circadian phase estimation procedure (CR1); middle panel: plasma melatonin data from the intervention day, with the 6.5-h experimental light exposure indicated by the open box; lower panel: plasma melatonin data from the final circadian phase estimation procedure (CR2) shown in the solid symbols, with data from CR1 replotted from above in the open symbols. During CR1, the fitted peak of the melatonin secretion (MELmax) occurred at 03:45, 3.5 h before habitual wake time. During CR2 MELmax occurred at 06:30, a 3.5 h phase delay. Melatonin was suppressed by 78% during the 6.5-h 3,527 lux light stimulus. Duffy et al Neurobiol Aging. 2007 May; 28(5): 799–807. 18 Melatonin suppression with bright light Phase shift of fitted plasma melatonin peak (MELmax) vs. illuminance of experimental light stimulus. Data from each of the ten subjects are plotted individually and shown with square symbols. Solid line represents the 4parameter logistic model fit to the data, with the 95% confidence interval of the model shown in the dotted lines. For comparison, the 4parameter logistic model fit to the data from our previous study in younger adults [64] is shown in the dashed line. Duffy et al Neurobiol Aging. 2007 May; 28(5): 799–807. 19 Circadian light transfer function Figueiro, et al. 2006 20 Clinical applications 21 Turner et al Br J Ophthalmol. 2008 November; 92(11): 1439–1444 22 Therapeutic light 2 Hours bright light in AM Improved sleep efficiency in NH residents Fetveit et al, 2003 30 minutes sunlight for five days Decreased napping Increased participation Alessi et al, 2005 Daytime bright light Improved sleep/wake cycle in persons with dementia (van Someren et al,1997) 23 Riemersma-van de Lek et al JAMA 2008 6/12 Homes randomized for lighting intervention Installed fluorescent fixtures, both real and sham 1000 lux horizontal at eyes in intervention Caregivers unaware which arm randomized to Melatonin randomized by patient 3.5 year follow up 24 MMSE, Depression 25 Riemersma-van der Lek, R. F. et al. JAMA 2008;299:2642-2655. Schedule change: Shift work Light at night (LAN) Nurses’ Health Study (Willet, PI) Effects of Light at Night on Circadian System in Nurses (Schernhammer, PI, RO1-OH008171) 26 Circadian phase shifters Can have negative effects on health Abrupt: jet lag, shift work Gradual: institutionalization Timed light exposure: reset clock Sensitivity age-related Bright light in morning advances the clock Bright light in evening delays the clock Delays easier than advances 27 Circadian Lighting in Longterm Care: A feasibility study 28 Methods 3 participants, residents of Ward 62B Lighting: GE fluorescent ceiling lamps 14,000 K Instruments Sleepwatch-L© (AMI, Ardsley, NY) Neuropsychiatric Inventory-Nursing Home Version DaysimeterTM (Lighting Research Center, Rensselear Polytechnic Institute) 29 Methods/Instrumentation for Sleep/Light Data Subject wore Sleep Watch-L© for 7 days Wrist-worn electronic measure of body movement and light Software calculates activity/inactivity and light © Ambulatory Monitoring Inc 30 31 Lighting Installation VAMC safety standards 1st phase: 3 ‘blue lamp’ prototypes by GE: 8000 Kelvin (K); 14,000K;16,000K 2nd: 13 standard fluorescent lighting ceiling light fixtures in Dayroom 7 of 13 changed to 14,000 K (6 remained @ 5000 K) Timer controlled blue lighting on, 8a-6p Lighting after 6pm: sufficient for visual acuity 32 33 Mean of light measurements taken at eye level (horizontally) at 8 points in the room in the 4 cardinal directions, using PMA 2200 Photoradiometer, SnP Meter Photopic SL3103001, S/N 9829 Light Conditions Photopic (cones) Lux Scotopic (rods) Lux S/P Ratio Brightness Visual Effectiveness all on 517 1178 2.24 781 1818 14,000 K only 381 918 2.26 606 759 standard 333 725 2.14 491 609 all off 222 489 2.17 328 412 34 Results & Conclusions Wrist actigraph well accepted Light sensor on wrist covered much of the time by clothing? New blue lighting well received 3 subjects exposure to blue lighting (time in Dayroom/ 10 hr period): 77 minutes, 371 mins, 373 mins Next time: Change installation pattern?, use DaysimeterTM 35 Rest-Activity and Light Exposure Patterns in the Home Setting: A Methodological Study P. Higgins, T. Hornick, M. Figueiro American J Alzheimer’s Disease and Other Dementias, 2010 36 Purpose Assess the feasibility and reliability of using a circadian light meter (DaysimeterTM) in a field setting and use the human circadian phototransduction model’s analyses to provide clinically relevant results 37 Dyad Caregiver – Wife, 73 years, “good health”, no vision problems, no sleep-aid meds. Primary caregiver Elder – Husband, 80 years, vascular dementia plus multiple co-morbidities, continent, needed assistance for all ADL’s and IADL’s, multiple meds included antidepressant but no sleep-aid Elder received all primary care from the Cleveland VA Geriatrics Clinical team. 38 Methods Procedure - Light exposure and restactivity data were collected over 7 consecutive days in November, 2007 Instruments Assessment of sleep quality and habits Home visit Sleepwatch-L© (AMI, Ardsley, NY) DaysimeterTM (Lighting Research Center, Rensselear Polytechnic Institute) 39 DaysimeterTM Research prototype Two light meters measure photopic and circadian light exposure Actigraph measures movement 40 Results 41 Built Environment Independent living complex for seniors Apartment: 640 square feet Brown paneling and beige paint and carpet One south facing window in bedroom Sliding glass door onto porch (south facing) Standard florescent lighting: kitchen and bath Incandescent lighting: floor and table lamps 42 Ambient light exposure/24 hrs when out of bed (lux) Light Norms (in lux)* Dyad data Elder Caregiver Range 0-449 0-3990 Mean mins: > 20 lux > 500 lux >1000 lux 191.5 0.0 0.0 635.5 18.0 8.0 Sunlight /reflective surfaces Overcast Day Avg nursing home Avg living room Twilight Full Moon 150,000 1,000 50 50-200 10 1 *From Turner, 2008. Br J Opthalmology 43 ACTIGRAPHY Caregiver wife Demented husband 70 257 81 446 81 119 17 105 31 96 0.71 0.69 0.95 44 0.76 Sleep-rest - Mean sleep efficiency % - Mean night sleep (mins) - Mean sleep latency (mins) - Mean wake after sleep onset [WASO] (mins) - Mean napping/24 hr (mins) Intra-daily variability (0-2) Inter-daily stability (0-1) 24-hour Sleep and Light Caregiver Elder 45 Caregiver 46 Entrained vs Disrupted Entrained Human 47 Disrupted Conclusions Daily light levels are very low Little variation in light levels Sleep Neither caregiver or elder sleep well Caregiver: poor circadian entrainment Sleep disruption causes Low lighting, little contrast Frequent wake times at night 48 Support VISN 10 GRECC, Cleveland VAMC Frances Payne Bolton School of Nursing, Case Western Reserve University, Cleveland, OH Lighting Research Center, Rensselear Polytechnic Institute, Troy NY General Electric Company, Nela Park, East Cleveland, OH 49 Team Tom Hornick, MD1,2 Patricia Higgins, PhD1,2 Mariana Figueiro, PhD3 Mark Rea, PhD3 Andy Bierman, MS3 John Bullough, PhD3 Bill Biers, PhD4 Mark Duffy, PhD4 Ed Yandek, BS4 1Case Western Reserve University 2Cleveland Veterans Affairs Medical Center 3Lighting Research Center, Rensselaer Polytechnic Institute 4General Electric Lighting, Nela Park 50 Next Steps “Methodology issues in a tailored light treatment for persons with dementia" R01 – M. Figueiro, PI 51 Wikipedia, accessed 5/2010 52 53